ADM Ezine Issue 4
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vocal Cord Dysfunction JAMES DECKERT, MD, Saint Louis University School of Medicine, St
Vocal Cord Dysfunction JAMES DECKERT, MD, Saint Louis University School of Medicine, St. Louis, Missouri LINDA DECKERT, MA, CCC-SLP, Special School District of St. Louis County, Town & Country, Missouri Vocal cord dysfunction involves inappropriate vocal cord motion that produces partial airway obstruction. Patients may present with respiratory distress that is often mistakenly diagnosed as asthma. Exercise, psychological conditions, airborne irritants, rhinosinusitis, gastroesophageal reflux disease, or use of certain medications may trigger vocal cord dysfunction. The differential diagnosis includes asthma, angioedema, vocal cord tumors, and vocal cord paralysis. Pulmo- nary function testing with a flow-volume loop and flexible laryngoscopy are valuable diagnostic tests for confirming vocal cord dysfunction. Treatment of acute episodes includes reassurance, breathing instruction, and use of a helium and oxygen mixture (heliox). Long-term manage- ment strategies include treatment for symptom triggers and speech therapy. (Am Fam Physician. 2010;81(2):156-159, 160. Copyright © 2010 American Academy of Family Physicians.) ▲ Patient information: ocal cord dysfunction is a syn- been previously diagnosed with asthma.8 A handout on vocal cord drome in which inappropriate Most patients with vocal cord dysfunction dysfunction, written by the authors of this article, is vocal cord motion produces par- have intermittent and relatively mild symp- provided on page 160. tial airway obstruction, leading toms, although some patients may have pro- toV subjective respiratory distress. When a per- longed and severe symptoms. son breathes normally, the vocal cords move Laryngospasm, a subtype of vocal cord away from the midline during inspiration and dysfunction, is a brief involuntary spasm of only slightly toward the midline during expi- the vocal cords that often produces aphonia ration.1 However, in patients with vocal cord and acute respiratory distress. -

Full Text (PDF)
REVIEW COPD Physiological and clinical relevance of exercise ventilatory efficiency in COPD J. Alberto Neder1, Danilo C. Berton1,2, Flavio F. Arbex3, Maria Clara Alencar4, Alcides Rocha3, Priscila A. Sperandio3, Paolo Palange5 and Denis E. O’Donnell1 Affiliations: 1Respiratory Investigation Unit and Laboratory of Clinical Exercise Physiology, Queen’s University and Kingston General Hospital, Kingston, ON, Canada. 2Division of Respiratory Medicine, Federal University of Rio Grande do Sul, Porto Alegre, Brazil. 3Pulmonary Function and Clinical Exercise Physiology, Respiratory Division, Federal University of Sao Paulo, Sao Paulo, Brazil. 4Division of Cardiology, Federal University of Minas Gerais, Belo Horizonte, Brazil. 5Dept of Public Health and Infectious Diseases, Sapienza University of Rome, Rome, Italy. Correspondence: J. Alberto Neder, 102 Stuart Street, Kingston, Ontario, Canada K7L 2V6. E-mail: [email protected] @ERSpublications Ventilatory efficiency is a key measurement for the interpretation of cardiopulmonary exercise testing in COPD http://ow.ly/1nsY307pbz8 Cite this article as: Neder JA, Berton DC, Arbex FF, et al. Physiological and clinical relevance of exercise ventilatory efficiency in COPD. Eur Respir J 2017; 49: 1602036 [https://doi.org/10.1183/13993003.02036- 2016]. ABSTRACT Exercise ventilation (V′E) relative to carbon dioxide output (V′CO2) is particularly relevant to patients limited by the respiratory system, e.g. those with chronic obstructive pulmonary disease (COPD). ′ − ′ High V E V CO2 (poor ventilatory efficiency) has been found to be a key physiological abnormality in symptomatic patients with largely preserved forced expiratory volume in 1 s (FEV1). Establishing an ′ − ′ association between high V E V CO2 and exertional dyspnoea in mild COPD provides evidence that exercise intolerance is not a mere consequence of detraining. -

The Use of Heliox in Treating Decompression Illness
The Diving Medical Advisory Committee DMAC, Eighth Floor, 52 Grosvenor Gardens, London SW1W 0AU, UK www.dmac-diving.org Tel: +44 (0) 20 7824 5520 [email protected] The Use of Heliox in Treating Decompression Illness DMAC 23 Rev. 1 – June 2014 Supersedes DMAC 23, which is now withdrawn There are many ways of treating decompression illness (DCI) at increased pressure. In the past 20 years, much has been published on the use of oxygen and helium/oxygen mixtures at different depths. There is, however, a paucity of carefully designed scientific studies. Most information is available from mathematical models, animal experiments and case reports. During a therapeutic compression, the use of a different inert gas from that breathed during the dive may facilitate bubble resolution. Gas diffusivity and solubility in blood and tissue is expected to play a complex role in bubble growth and shrinkage. Mathematical models, supported by some animal studies, suggest that breathing a heliox gas mixture during recompression could be beneficial for nitrogen elimination after air dives. In humans, diving to 50 msw, with air or nitrox, almost all cases of DCI can be adequately treated at 2.8 bar (18 msw), where 100% oxygen is both safe and effective. Serious neurological and vestibular DCI with only partial improvements during initial compression at 18 msw on oxygen may benefit from further recompression to 30 msw with heliox 50:50 (Comex therapeutic table 30 – CX30). There have been cases successfully treated on 50:50 heliox (CX30), on the US Navy recompression tables with 80:20 and 60:40 heliox (USN treatment table 6A) instead of air and in heliox saturation. -

Estimating Your Air Consumption
10/29/2019 Alert Diver | Estimating Your Air Consumption Estimating Your Air Consumption Advanced Diving Public Safety Diving By Mike Ange Mastering Neutral Buoyancy and Trim Military Diving Technical Diving Scientific Diving and Safety Program Oversight Seeing the Reef in a New Light ADVERTISEMENT Do you have enough breathing gas to complete the next dive? Here's how to find out. It is a warm clear day, and the Atlantic Ocean is like glass. As you drop into the water for a dive on North Carolina's famous U-352 wreck, you can see that the :: captain has hooked the wreck very near the stern. It is your plan to circumnavigate the entire structure and get that perfect photograph near the exposed bow torpedo tube. You descend to slightly below 100 feet, reach the structure and take off toward the bow. Unfortunately, you are only halfway, just approaching the conning tower, when your buddy signals that he is running low on air. Putting safety first, you return with him to the ascent line — cursing the lost opportunity and vowing to find a new buddy. If you've ever experienced the disappointment of ending a dive too soon for lack of breathing gas or, worse, had to make a hurried ascent because you ran out of air, it may surprise you to learn that your predicament was entirely predictable. With a little planning and some basic calculations, you can estimate how much breathing gas you will need to complete a dive and then take steps to ensure an adequate supply. It's a process that technical divers live by and one that can also be applied to basic open-water diving. -
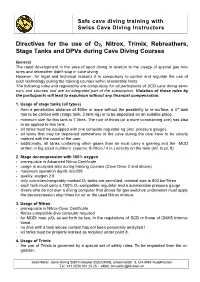
Directives for the Use of O 2, Nitrox, Trimix, Rebreathers, Stage Tanks
Safe cave diving training with Swiss Cave Diving Instructors Directives for the use o f O 2 , Nitrox, Trimix, Rebreathers, S tage Tanks and DPVs during Cave Diving Courses General The rapid development in the area of sport diving in relation to the u sage of special gas mi x- tures and rebreather didn't stop in cave diving. However, for legal and technical reasons it is compulsory to control and regulate the use of such tec h nology during the training courses within reasonable limits. The following rules a nd regulations are compulsory for all participants of SCD cave diving sem i- nars and courses and are an integrated part of the subscription. Violation of those rules by the participants will lead to expulsion without any financial compensation. 1. Usage of stage tanks (all types) - from a penetration distance of 500m or more without the possibility to re - surface, a 3 rd tank has to be carried with (stage tank, 3 tank rig) or to be deposited on an suitable place. - minimum size for this tank is 7 litres. The r ule of thirds (or a more constraining one) has also to be applied to this tank. - all tanks must be equipped with one complete regulator rig (incl. pressure gauge). - all tanks that may be deposited somewhere in the cave during the dive have to be clearly marked with the name of the user . - addition ally , a ll tanks containing other gases than air must carr y a gas - tag and the MOD written in big sized numbers (approx. -

Underwater Photography Made Easy
Underwater Photography Made Easy Create amazing photos & video with by Annie Crawley IncludingIncluding highhigh definitiondefinition videovideo andand photophoto galleriesgalleries toto showshow youyou positioningpositioning andand bestbest techniques!techniques! BY ANNIE CRAWLEY SeaLife Cameras Perfect for every environment whether you are headed on a tropical vacation or diving the Puget Sound. These cameras meet all of your imaging needs! ©2013 Annie Crawley www.Sealife-cameras.com www.DiveIntoYourImagination.com Edmonds Underwater Park, Washington All rights reserved. This interactive book, or parts thereof, may not be reproduced in any form without permission in writing from the publisher, Dive Into Your Imagination, LLC a company founded by Annie Crawley committed to change the way a new generation views the Ocean and themselves. Dive Into Your Imagination, Reg. Pat. & Tm. Off. Underwater Photography Made Easy shows you how to take great photos and video with your SeaLife camera system. After our introduction to this interactive book you will learn: 1. Easy to apply tips and tricks to help you create great images. 2. Five quick review steps to make sure your SeaLife camera system is ready before every dive. 3. Neutral buoyancy tips to help you take great underwater photos & video with your SeaLife camera system. 4. Macro and wide angle photography and video basics including color, composition, understanding the rule of thirds, leading diagonals, foreground and background considerations, plus lighting with strobes and video lights. 5. Techniques for both temperate and tropical waters, how to photograph divers, fish behavior and interaction shots, the difference in capturing animal portraits versus recording action in video. You will learn how to capture sharks, turtles, dolphins, clownfish, plus so much more. -

Respiratory Therapy Pocket Reference
Pulmonary Physiology Volume Control Pressure Control Pressure Support Respiratory Therapy “AC” Assist Control; AC-VC, ~CMV (controlled mandatory Measure of static lung compliance. If in AC-VC, perform a.k.a. a.k.a. AC-PC; Assist Control Pressure Control; ~CMV-PC a.k.a PS (~BiPAP). Spontaneous: Pressure-present inspiratory pause (when there is no flow, there is no effect ventilation = all modes with RR and fixed Ti) PPlateau of Resistance; Pplat@Palv); or set Pause Time ~0.5s; RR, Pinsp, PEEP, FiO2, Flow Trigger, rise time, I:E (set Pocket Reference RR, Vt, PEEP, FiO2, Flow Trigger, Flow pattern, I:E (either Settings Pinsp, PEEP, FiO2, Flow Trigger, Rise time Target: < 30, Optimal: ~ 25 Settings directly or by inspiratory time Ti) Settings directly or via peak flow, Ti settings) Decreasing Ramp (potentially more physiologic) PIP: Total inspiratory work by vent; Reflects resistance & - Decreasing Ramp (potentially more physiologic) Card design by Respiratory care providers from: Square wave/constant vs Decreasing Ramp (potentially Flow Determined by: 1) PS level, 2) R, Rise Time ( rise time ® PPeak inspiratory compliance; Normal ~20 cmH20 (@8cc/kg and adult ETT); - Peak Flow determined by 1) Pinsp level, 2) R, 3)Ti (shorter Flow more physiologic) ¯ peak flow and 3.) pt effort Resp failure 30-40 (low VT use); Concern if >40. Flow = more flow), 4) pressure rise time (¯ Rise Time ® Peak v 0.9 Flow), 5) pt effort ( effort ® peak flow) Pplat-PEEP: tidal stress (lung injury & mortality risk). Target Determined by set RR, Vt, & Flow Pattern (i.e. for any set I:E Determined by patient effort & flow termination (“Esens” – PDriving peak flow, Square (¯ Ti) & Ramp ( Ti); Normal Ti: 1-1.5s; see below “Breath Termination”) < 15 cmH2O. -

Training Objectives for a Diving Medical Physician
The Diving Medical Advisory Committee Training Objectives for a Diving Medicine Physician This guidance includes all the training objectives agreed by the Diving Medical Advisory Committee, the European Diving Technology Committee and the European Committee for Hyperbaric Medicine in 2011. Rev 1 - 2013 INTRODUCTION The purpose of this document is to define more closely the training objectives in diving physiology and medicine that need to be met by doctors already fully accredited or board-certified in a clinical speciality to national standards. It is based on topic headings that were originally prepared for a working group of European Diving Technology Committee (EDTC) and the European Committee of Hyperbaric Medicine (ECHM) as a guide for diving medicine some 20 years ago by J.Desola (Spain), T.Nome (Norway) & D.H.Elliott (U.K.). The training now required for medical examiners of working divers and for specialist diving medicine physicians was based on a EDTC/ECHM standard 1999 and subsequently has been enhanced by the Diving Medical Advisory Committee (DMAC), revised and agreed in principle by DMAC, EDTC and ECHM in 2010 and then ratified by EDTC and ECHM in 2011. The requirements now relate to an assessment of competence, the need for some training in occupational medicine, the need for maintenance of those skills by individual ‘refresher training’. Formal recognition of all this includes the need to involve a national authority for medical education. These objectives have been applied internationally to doctors who provide medical support to working divers. (Most recreational instructors and dive guides are, by their employment, working divers and so the guidance includes the relevant aspects of recreational diving. -

A Review of the Use of Heliox in the Critically Ill
Special review A Review of the use of Heliox in the Critically Ill T. WIGMORE, E. STACHOWSKI Intensive Care Unit, Westmead Hospital, Westmead, NEW SOUTH WALES ABSTRACT Heliox, a mix of oxygen and helium, has a number of potential medical applications resulting from its relatively lower density. This paper reviews the physics underlying its utility and considers the evidence for its use. While there are studies that support its role, particularly in patients with exacerbations of asthma and chronic obstructive pulmonary disease (COPD), the data are inconclusive. (Critical Care and Resuscitation 2006; 8: 64-72) Key words: Heliox, helium, airway obstruction, asthma, chronic obstructive pulmonary disease Helium was discovered in 1868 by the French astro- a given pressure difference. Clinically this can be utilis- nomer Pierre-Jules-Cesar Janssen during a spectro- ed to assist patients who suffer from airway narrowing. scopic study of a total solar eclipse in India. It was named later the same year by the British astronomer Table 1. Physical properties of pure gases at RTP Joseph Norman Lockyer and chemist Sir Edward (298 degrees Kelvin and 1 atmosphere pressure) Frankland, the name derived from helios, the Greek for Density Viscosity Thermal sun. It is an inert gas present in the atmosphere (ρ) (η) conductivity (0.00052%) and was used initially in airships and Kg/m3 microPoise W/m K balloons. Today, most commercial helium is recovered from Air 1.184 184.33 0.025 natural gas using a cryogenic separation process, foll- owing which it is refined and liquefied. Liquid helium is Carbon 1.811 148.71 0.017 shipped from the production site to various storage Dioxide facilities worldwide before being distributed in the Helium 0.166 197.61 0.14 gaseous form into cylinders for on-site use. -

Wreck Diver Specialty Course Instructor Guide
Instructor Wreck Diver Guide Wreck Diver Specialty Course Instructor Guide Product No. 70232 (Rev. 4/07) Version 2.0 Instructor Guide Wreck Diver PADI Wreck Diver Specialty Course Instructor Guide © PADI 2007 Portions of the Appendix of this guide may be reproduced by PADI Members for use in PADI-sanctioned training, but not for resale or personal gain. No other reproduction is allowed without the express written permission of PADI. Published and distributed by PADI 30151 Tomas Rancho Santa Margarita, CA 92688-2125 USA Printed in U.S.A. Product No. 70232 (04/07) Version 2.0 2 Specialty Course Instructor Guide Instructor Wreck Diver Guide Table of Contents Introduction How to Use this Guide .......................................................................................5 Course Philosophy and Goals .............................................................................5 Course Flow Options .........................................................................................6 Program Options ................................................................................................7 Section One: Course Standards Standards at a Glance .........................................................................................8 Instructor Prerequisites .......................................................................................9 Student Diver Prerequisites ...............................................................................9 Supervision and Ratios .......................................................................................9 -

<P>The Texas Education Agency (TEA) Proposes the Repeal of <*>100
The State Board of Education (SBOE) adopts the repeal of §§130.13, 130.14, and 130.308-130.310 and new §§130.123-130.127, 130.315-130.318, 130.420-130.435, and 130.485-130.491, concerning Texas Essential Knowledge and Skills (TEKS) for career and technical education (CTE). The repeals and new sections are adopted without changes to the proposed text as published in the March 6, 2020 issue of the Texas Register (45 TexReg 1551) and will not be republished. The adopted repeals and new sections update the TEKS to align with recent legislation requiring the board to consolidate high school technology applications TEKS into CTE TEKS and eliminate TEKS for duplicative courses. The new sections also update the TEKS for CTE to add a new career cluster in energy to align with revised programs of study. REASONED JUSTIFICATION: The 86th Texas Legislature, 2019, passed House Bill 963, which required the SBOE, not later than March 1, 2020, to conduct a review of the TEKS for CTE and technology applications courses for Grades 9-12 and amend the board's rules to consolidate courses and eliminate duplicative courses. The SBOE is only required to implement this provision if the legislature appropriated money specifically for that purpose. If the legislature did not appropriate money specifically for that purpose, the SBOE may, but is not required to, implement a requirement using other appropriations available for that purpose. The legislature did not appropriate money specifically for the purpose of implementing this requirement. Texas is redesigning state-level programs of study to include coherent and rigorous content with challenging academic standards and relevant career and technical content. -

EMS DIVISION 23.1 Rev. 07/31/2020 PROTOCOL 23 WATER RELATED INCIDENTS
PROTOCOL 23 WATER RELATED INCIDENTS A. Introduction “Drowning is the process of experiencing respiratory impairment from submersion / immersion in liquid” The word Drowning, should be used to refer to a person who drowned (death) or to a person who was rescued (fatal drowning or non-fatal drowning.) Water Rescue is the process of removing someone from the water in which dangerous conditions are present but the victim shows no signs of respiratory impairment. General Care 1. Initial assessment/Care Protocol 1. 2. Administer 15 L/min Oxygen via NRB mask. 3. Maintain normal body temperature to protect against hypothermia. B. Drowning EMR/BLS 1. Consider concurrent trauma and manage accordingly Protocol 21. 2. Consider insertion of I-gel with NG Tube (Lifeguards only) Procedure 49 and Procedure 12. 3. Determine important history from the patient or bystanders which includes: a) Duration of submersion b) Water temperature c) Any possibility of seizure activity d) Any associated drug or alcohol use e) How the patient entered the water 4. All non-fatal drowning victims must be transported to the closest appropriate facility for evaluation, regardless of how well they may seem to have recovered. Delayed death or complications due to pulmonary edema or aspiration pneumonia are common. ALS 5. Consider insertion of an NG/OG Procedure 12. EMS DIVISION 23.1 Rev. 07/31/2020 PROTOCOL 23 WATER RELATED INCIDENTS 6. Treat dysrhythmias per specific protocols. Consider hypoxia as a primary cause of the dysrhythmias. C. Decompression Sickness/Air Embolism EMR/BLS 1. Evaluate for specific signs and symptoms: a) Pain (primarily joint pain) b) Altered level of consciousness c) Generalized numbness or confusion d) Weakness or paralysis e) External or diagnosed internal bleeding f) Extreme vertigo 2.