Part 11 Business Regulation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Annual Review of Performance 2016/17
Annual review of performance 2016/17 General Dental Council About the Professional Standards Authority The Professional Standards Authority for Health and Social Care1 promotes the health, safety and wellbeing of patients, service users and the public by raising standards of regulation and voluntary registration of people working in health and care. We are an independent body, accountable to the UK Parliament. We oversee the work of nine statutory bodies that regulate health professionals in the UK and social workers in England. We review the regulators’ performance and audit and scrutinise their decisions about whether people on their registers are fit to practise. We also set standards for organisations holding voluntary registers for people in unregulated health and care occupations and accredit those organisations that meet our standards. To encourage improvement we share good practice and knowledge, conduct research and introduce new ideas including our concept of right-touch regulation.2 We monitor policy developments in the UK and internationally and provide advice to governments and others on matters relating to people working in health and care. We also undertake some international commissions to extend our understanding of regulation and to promote safety in the mobility of the health and care workforce. We are committed to being independent, impartial, fair, accessible and consistent. More information about our work and the approach we take is available at www.professionalstandards.org.uk. 1 The Professional Standards Authority for Health and Social Care was previously known as the Council for Healthcare Regulatory Excellence 2 Right-touch regulation revised (October 2015). Available at www.professionalstandards.org.uk/policy-and-research/right-touch-regulation Contents 1. -

Check Your Optician Is Registered Gocpatientsbooklet1qx 5/8/10 11:30 Page 2
GOCPatientsBooklet1QX 5/8/10 11:30 Page 1 Check your optician is registered GOCPatientsBooklet1QX 5/8/10 11:30 Page 2 This booklet tells you who we, the General Optical Council (GOC), are. It also tells you what we do and how our services can help you. About us We regulate opticians, students training to be opticians and optical businesses in the UK. There are currently around 23,500 optometrists, dispensing opticians, student opticians and optical businesses on our registers. Our powers come from the Opticians Act 1989. What do the different words mean? An optometrist is the person who tests your sight. They can also fit and supply glasses or contact lenses. A dispensing optician is the person who fits and supplies your glasses or contact lenses. Ophthalmologists and ophthalmic medical practitioners (OMPs) are medically-qualified doctors who specialise in eye conditions. They are also allowed to test your sight and fit and supply glasses and contact lenses. Ophthalmologists and OMPs are registered by the General Medical Council. In this booklet we describe optometrists and dispensing opticians as ‘opticians’. 2 We describe people who are registered with us as ‘registrants’. We use these terms to make it clearer for you. What is regulation? Regulators protect the public by: • restricting who can practise a profession; • making sure that their registrants are suitably qualified; and • making sure that their registrants are fit to practise safely. We are one of nine healthcare regulators in the UK. The other regulators are: • the General Chiropractic Council; • the General Dental Council; • the General Medical Council; • the General Osteopathic Council; • the Health Professions Council; • the Nursing and Midwifery Council; • the Pharmaceutical Society of Northern Ireland; and • the Royal Pharmaceutical Society of Great Britain. -

A Review of the Literature on Continuing Professional Development (CPD)
A Review of the Literature on Continuing Professional Development (CPD) Commissioned by the General Dental Council (GDC) to inform their policy proposals for CPD development 10 January 2019 Association for Dental Education in Europe (ADEE) 10 January 2019 Association for Dental Education in Europe International Office Dublin Dental School and Hospital Trinity College, Lincoln Place Dublin 2, Ireland T: +353 1 612 7287 / 7235 F: +353 1 612 7294 Project Team Professor Jonathan Cowpe, emeritus professor, Cardiff University, School of Dentistry (Project Lead) Dr Argyro Kavadella, Athens University, School of Dentistry (Lead Project Researcher) Professor Alison Bullock, Cardiff University, School of Social Sciences, (Expert Advisor & Researcher) Ms Emma Barnes, Cardiff University, School of Social Sciences (Search Advisor & Researcher) Dr Barry Quinn, King’s College London (Project Researcher) Mr Denis Murphy, Chief Administrative Officer of ADEE (Project Administrator) Contents GLOSSARY ................................................................................................................................................ Other abbreviations ............................................................................................................................. EXECUTIVE SUMMARY ............................................................................................................................ i INTRODUCTION ...................................................................................................................................... -

A Better, Fairer System of Dental Regulation 2
Shifting the balance: a better, fairer system of dental regulation 2 Good regulation starts ‘upstream’ with communications, engagement and learning; persuasion and influence; leadership, partnership and an expression of common goals 3 Contents Chair’s foreword 4 Introduction 6 1. Moving upstream 15 2. First tier complaints 34 3. Working with partners 45 4. Refocusing fitness to practise 51 Building on principles: news steps 59 Proposals for action 60 4 Chair’s foreword The GDC is seeking to open and stimulate a serious public debate on the future of dental regulation. In the development of the ideas contained here we have engaged extensively with many of the groups and individuals that have a stake in dental regulation: professionals and their representative bodies, patient groups, regulators, educators, policy makers and others. We will continue to build on this engagement over the coming months, ensuring that we reach patients and professionals across the United Kingdom (UK). We want to seek views from everyone with an interest in the regulation of dentistry. The public expects and depends on safe, effective dental care that puts patients first. We know that is what the overwhelming majority of the dentists and dental care professionals working across the UK aspire to, and succeed in, delivering. They are committed and hard-working professionals in whom the public rightly places its trust. However, there can be challenges to fulfilling those expectations, for a range of reasons. For example: • there may be tensions between what the patient -

Performance Review 2019/20 GENERAL DENTAL COUNCIL
for Health and Social Care performance review 2019/20 GENERAL DENTAL COUNCIL 21 ABOUT THE PERFORMANCE REVIEW PROCESS We aim to protect the public by improving the regulation of people who work in health and care. This includes our oversight of 10 organisations that regulate health and care professionals in the UK. As described in our legislation, we have a statutory duty to report annually to Parliament on the performance of each of these 10 regulators. Our performance reviews look at the regulators’ performance against our Standards of Good Regulation, which describe the outcomes we expect regulators to achieve. They cover the key areas of the regulators’ work, together with the more general expectations about the way in which we would expect the regulators to act. In carrying out our reviews, we aim to take a proportionate approach based on the information that is available about the regulator. In doing so, we look at concerns and information available to us from other stakeholders and members of the public. The process is overseen by a panel of the Authority’s senior staff. We initially assess the information that we have and which is publicly available about the regulator. We then identify matters on which we might require further information in order to determine whether a Standard is met. This further review might involve an audit of cases considered by the regulator or its processes for carrying out any of its activities. Once we have gathered this further information, we decide whether the individual Standards are met and set out any concerns or areas for improvement. -

Ddcn 1199/2010
Change Request NHS Connecting for Health NHS Data Model and Dictionary Service Reference: Change Request 1199 Version No: 1.0 Subject: General Pharmaceutical Council and Royal Pharmaceutical Society of Great Britain Update Effective Date: Immediate Reason for Change: Organisation Change Publication Date: 6 October 2010 Background: DDCN 1143/2010 "General Pharmaceutical Council" advised that the General Pharmaceutical Council aimed to become operational on 27 September 2010. The General Pharmaceutical Council is now operational and this Data Dictionary Change Notice updates the NHS Data Model and Dictionary as follows: z Changes the name of the Royal Pharmaceutical Society of Great Britain to Royal Pharmaceutical Society and updates the description z Updates the description for the General Pharmaceutical Council, as it is now a regulatory body z Updates other affected pages within the NHS Data Model and Dictionary to reflect these changes Note: Both updated NHS Business Definitions have been agreed by the appropriate organisation. Summary of changes: Supporting Information GENERAL PHARMACEUTICAL COUNCIL Changed Description ORGANISATIONS INTRODUCTION Changed Description ORGANISATIONS MENU Changed Description REGULATORY BODY Changed Description ROYAL PHARMACEUTICAL SOCIETY renamed from ROYAL PHARMACEUTICAL Changed Name, Aliases, Description SOCIETY OF GREAT BRITAIN Attribute Definitions PROFESSIONAL REGISTRATION BODY CODE Changed Description Date: 6 October 2010 Sponsor: Ken Lunn, Director of Data Standards and Products, NHS Connecting for Health Note: New text is shown with a blue background. Deleted text is crossed out. Retired text is shown in grey. Within the Diagrams deleted classes and relationships are red, changed items are blue and new items are green. GENERAL PHARMACEUTICAL COUNCIL Change to Supporting Information: Changed Description The General Pharmaceutical Council (GPhC) is a new, shadow ORGANISATION that became an independent legal entity on 12 March 2010.The General Pharmaceutical Council (GPhC) is a Regulatory Body. -
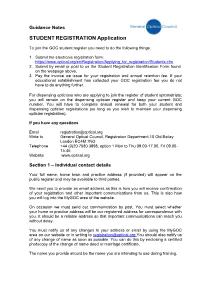
STUDENT REGISTRATION Application
Guidance Notes STUDENT REGISTRATION Application To join the GOC student register you need to do the following things: 1. Submit the electronic registration form: https://www.optical.org/en/Registration/Applying_for_registration/Students.cfm 2. Submit by email or post to us the Student Registration Identification Form found on the webpage above. 3. Pay the invoice we issue for your registration and annual retention fee. If your educational establishment has collected your GOC registration fee you do not have to do anything further. For dispensing opticians who are applying to join the register of student optometrists; you will remain on the dispensing optician register and keep your current GOC number. You will have to complete annual renewal for both your student and dispensing optician registrations (so long as you wish to maintain your dispensing optician registration). If you have any questions Email [email protected] Write to General Optical Council, Registration Department,10 Old Bailey London EC4M 7NG Telephone +44 (0)20 7580 3898, option 1 Mon to Thu 09.00-17.00, Fri 09.00- 16.45 Website www.optical.org Section 1 – Individual contact details Your full name, home town and practice address (if provided) will appear on the public register and may be available to third parties. We need you to provide an email address as this is how you will receive confirmation of your registration and other important communications from us. This is also how you will log into the MyGOC area of the website. On occasion we must send out communication by post. You must select whether your home or practice address will be our registered address for correspondence with you. -

Guidance Notes
Guidance Notes FULLY QUALIFIED REGISTRATION Application To join the GOC fully qualified register you need to do the following things: 1. Submit the electronic registration form: https://www.optical.org/en/Registration/Applying_for_registration/fully- qualified.cfm 2. Submit by email or post to us the Registration Identification Form found on the webpage above. 3. Pay the invoice we issue for your registration and annual retention fee. Please note that upon registration your name will be removed from the student register on successful application to the full register. If applicable, your entry in the register of dispensing opticians will be removed on successful application to the register of optometrists. If you have any questions Email [email protected] Write to General Optical Council, Registration Department,10 Old Bailey London EC4M 7NG Telephone +44 (0)20 7580 3898, option 1 Mon to Thu 09.00-17.00, Fri 09.00- 16.45 Website www.optical.org Section 1 – Individual contact details Your full name, home town and practice address (if provided) will appear on the public register and may be available to third parties. We need you to provide an email address as this is how you will receive confirmation of your registration and other important communications from us. This is also how you will log into the MyGOC area of the website. On occasion we must send out communication by post. You must select whether your home or practice address will be our registered address for correspondence with you. It should be a reliable address so that important communications can reach you without delay. -

GDC Additional Skills
CALL FOR IDEAS GDC Consultation What do patients need and want to know about dental professionals’ additional skills and qualifications? The deadline for responses is 5.00pm on Friday 9 May 2008 Please reply to: Moragh Loose Additional Skills Consultation General Dental Council 37 Wimpole Street London W1G 8DQ You can also reply by email to: [email protected]. This consultation pack contains: - an explanation of some terms you will find in the consultation; - some background information explaining what we are consulting on and why; - consultation questions; - Annex A - a “Frequently Asked Questions” document on current additional qualifications/skills policy; - Annex B - draft guidance on dental professionals‟ scope of practice to help you answer the questions in this consultation; - Annex C - guidance on what will happen to your response once the consultation has closed; - Annex D - a list of organisations we are sending this consultation to; - Annex E - a copy of the patient leaflet Who regulates health and social care professionals? which gives more information on what the GDC does. General Dental Council 37 Wimpole Street London W1G 8DQ Tel: 020 7887 3800 Fax: 020 7224 3294 Minicom: 18001 020 7887 3800 (via TypeTalk) Email: [email protected] Explanation of terms used in this consultation Continuing professional development (CPD) – by law, registered dentists have to be able to demonstrate that they are compliant with our CPD scheme. This requires them to keep their knowledge and skills up-to-date so that they provide high quality patient care. Dental care professionals will also have to do this from August 2008. -
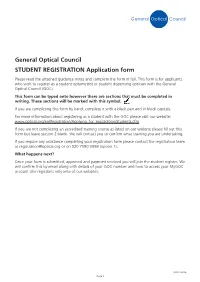
General Optical Council STUDENT REGISTRATION Application Form
General Optical Council STUDENT REGISTRATION Application form Please read the attached guidance notes and complete the form in full. This form is for applicants who wish to register as a student optometrist or student dispensing optician with the General Optical Council (GOC). This form can be typed onto however there are sections that must be completed in writing. These sections will be marked with this symbol. If you are completing this form by hand, complete it with a black pen and in block capitals. For more information about registering as a student with the GOC please visit our website: www.optical.org/en/Registration/Applying_for_registration/Students.cfm If you are not completing an accredited training course as listed on our website please fill out this form but leave section 2 blank. We will contact you to confirm what training you are undertaking. If you require any assistance completing your registration form please contact the registration team at [email protected] or on 020 7580 3898 (option 1). What happens next? Once your form is submitted, approved and payment received you will join the student register. We will confirm this by email along with details of your GOC number and how to access your MyGOC account (the registrant only area of our website). SR001 08/16 Page 1 Checklist Please complete all sections of the application form and read the guidance notes before completing the form. Have you selected an option from Student Optometrist or Student Dispensing Optician? Section 1 – Contact details Have you provided -

FULLY QUALIFIED REGISTRATION Application
Guidance Notes FULLY QUALIFIED REGISTRATION Application To join the GOC fully qualified register you need to do the following things: 1. Submit the electronic registration form: https://www.optical.org/en/Registration/Applying_for_registration/fully- qualified.cfm 2. Submit by email or post to us the Registration Identification Form found on the webpage above. 3. Pay the invoice we issue for your registration and annual retention fee. Please note that upon registration your name will be removed from the student register on successful application to the full register. If applicable, your entry in the register of dispensing opticians will be removed on successful application to the register of optometrists. If you have any questions Email [email protected] Write to General Optical Council, Registration Department,10 Old Bailey London EC4M 7NG Telephone +44 (0)20 7580 3898, option 1 Mon to Thu 09.00-17.00, Fri 09.00- 16.45 Website www.optical.org Section 1 – Individual contact details Your full name, home town and practice address (if provided) will appear on the public register and may be available to third parties. We need you to provide an email address as this is how you will receive confirmation of your registration and other important communications from us. This is also how you will log into the MyGOC area of the website. On occasion we must send out communication by post. You must select whether your home or practice address will be our registered address for correspondence with you. It should be a reliable address so that important communications can reach you without delay. -

Principles for Good Practice in Remote Consultations and Prescribing
High level principles for good practice in remote consultations and prescribing This information is for all healthcare professionals with prescribing responsibilities. It sets out the shared high level principles of good practice expected of everyone when consulting and or prescribing remotely from the patient. The principles are underpinned by existing standards and guidance from professional and system regulators. Healthcare professionals should continue to follow guidance from regulatory bodies and take clinical guidance into account in their decision making. This information is not clinical guidance or new guidance from regulatory bodies. These principles have been co-authored and agreed by a range of healthcare regulators and organisations (see Annex A). Safeguards for patients accessing healthcare remotely Remote consultations and prescribing provided online, over video-link or by phone can benefit patients1, save resources and help meet public demand for more convenient access to healthcare. However, there are potential patient safety risks, particularly where services aren’t linked to a patient’s NHS GP or regular healthcare provider, and where there may be limited access to a patient’s medical records. Issues include increased attempts to gain access to medicines which can cause serious harm and the need to ensure safe ongoing monitoring of those with long term conditions. Providers of remote services and the healthcare professionals they work with must be aware of these risks and be clear about their responsibilities for protecting patients. Patients can expect to have effective safeguards in place to protect them when they receive advice and treatment remotely. Safeguards are necessary whether the consultation happens in the context of a continuing treating relationship or is a one- off interaction between a patient and a healthcare professional.