Guideline Documentation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

S Values in Accordance with Soczewiński-Wachtmeisters Equation
S values in accordance with Soczewiński-Wachtmeisters equation S value from Antiparasitic drugs: Soczewiński’s Metronidazole Ornidazole Secnidazole Tinidazole Equation* S(m) 1.614 2.161 1.921 1.911 S(a) 1.634 2.159 1.887 1.923 S value from Antihypertensive drugs: Soczewiński’s Nilvadipine Felodipine Isradipine Lacidipine equation 4.129 4.597 3.741 5.349 S(m) S(a) 5.330 4.841 4.715 5.690 S value from Non-steroidal anti-inflammatory drugs (NSAIDs): Soczewiński’s Mefenamic Indomethacin Nabumetone Phenylbutazone Carprofen Ketoprofen Flurbiprofen equation acid 2.879 2.773 3.456 2.682 2.854 2.139 2.568 S(m) 3.317 3.442 3.910 2.404 3.394 1.968 2.010 S(a) *where: S(m) – S is the slope of the regression curie in accordance with Soczewiński-Wachtmeisters equation using methanol-water mobile phase S(a) – S is the slope of the regression curie in accordance with Soczewiński-Wachtmeisters equation using acetone-water mobile phase First group of drugs (antiparasitic drugs) 1. Metronidazole (2-Methyl-5-nitroimidazole-1-ethanol) 2. Ornidazole (1-(3-Chloro-2-hydroxypropyl)-2-methyl-5-nitroimidazole) 3. Secnidazole (1-(2-methyl-5-nitro-1H-imidazol-1-yl) propan-2ol, 1-(2Hydroxypropyl)-2-methyl-5- nitroimidazole) 4. Tinidazole (1-[2-(Ethylsulfonyl)ethyl]-2-methyl-5-nitroimidazole) Second group of drugs (antihypertensive drugs) 1. Nilvadipine (2-Cyano-1,4-dihydro-6-methyl-4-(3-nitrophenyl)-3,5-pyridinedicarboxylic acid 3- methyl 5-(1-methylethyl) ester, 5-Isopropyl-3-methyl-2-cyano-1,4-dihydro-6-methyl-4-(m- nitrophenyl)-3,5-pyridinedicarboxylate, FK-235, FR-34235, Isopropyl 6-cyano-5-methoxycarbonyl-2- methyl-4-(3-nitrophenyl)-1,4-dihydropyridine-3-carboxylate) 2. -

Effect of Lacidipine and Nifedipine GITS on Platelet Function in Patients with Essential Hypertension
Journal of Human Hypertension (2000) 14, Suppl 1, S91–S95 2000 Macmillan Publishers Ltd All rights reserved 0950-9240/00 $15.00 www.nature.com/jhh Effect of lacidipine and nifedipine GITS on platelet function in patients with essential hypertension MC Armas-Padilla1, MJ Armas-Herna´ndez1, R Herna´ndez-Herna´ndez1, M Velasco2, B Pacheco1, AR Carvajal1 and A Castillo-Moreno1 1Clinical Pharmacology Unit, School of Medicine, Universidad Centroccidental Lisandro Alvarado, Barquisimeto, Venezuela; 2Clinical Pharmacology Unit, Vargas Medical School, Central University of Venezuela, Caracas, Venezuela With the aim of evaluating the effects on blood pressure, Both drugs reduced systolic and diastolic blood press- platelet function and insulin sensitivity of the dihydro- ure at the same level, however there were observable piridines lacidipine and nifedipine GITS, a parallel dou- differences in the rate of reduction. The nifedipine GITS ble-blind study was carried out in a group of 20 patients reduced supine systolic blood pressure by 25 mm Hg in with mild to moderate essential hypertension. They the first week, while the lacidipine did so by 11 mm Hg. received a placebo for 4 weeks; then were divided at At the end of the study period nifedipine reduced supine random into two groups of 10 patients each. Nifedipine systolic blood pressure by 28 mm Hg and lacidipine by GITS, 30 mg and lacidipine, 4 mg, were given during 16 20 mm Hg. Heart rate was increased slightly but signifi- weeks of active treatment. Blood pressure and heart cantly in the nifedipine GITS group only in the standing rate were measured at the clinic in supine, sitting and position. -

Dorset Medicines Advisory Group
DORSET CARDIOLOGY WORKING GROUP GUIDELINE FOR CALCIUM CHANNEL BLOCKERS IN HYPERTENSION SUMMARY The pan-Dorset cardiology working group continues to recommend the use of amlodipine (a third generation dihydropyridine calcium-channel blocker) as first choice calcium channel blocker on the pan-Dorset formulary for hypertension. Lercanidipine is second choice, lacidipine third choice and felodipine is fourth choice. This is due to preferable side effect profiles in terms of ankle oedema and relative costs of the preparations. Note: where angina is the primary indication or is a co-morbidity prescribers must check against the specific product characteristics (SPC) for an individual drug to confirm this is a licensed indication. N.B. Lacidipine and lercandipine are only licensed for use in hypertension. Chapter 02.06.02 CCBs section of the Formulary has undergone an evidence-based review. A comprehensive literature search was carried out on NHS Evidence, Medline, EMBASE, Cochrane Database, and UK Duets. This was for recent reviews or meta-analyses on calcium channel blockers from 2009 onwards (comparative efficacy and side effects) and randomised controlled trials (RCTs). REVIEW BACKGROUND Very little good quality evidence exists. No reviews, meta-analyses or RCTs were found covering all calcium channel blockers currently on the formulary. Another limitation was difficulty obtaining full text original papers for some of the references therefore having to use those from more obscure journals instead. Some discrepancies exist between classification of generations of dihydropyridine CCBs, depending upon the year of publication of the reference/authors’ interpretation. Dihydropyridine (DHP) CCBs tend to be more potent vasodilators than non-dihydropyridine (non-DHP) CCBs (diltiazem, verapamil), but the latter have greater inotropic effects. -

A Different Dihydropyridine Calcium Channel Blocker in Hypertensive Patients Who Developed Pedal Edema on Dihydropyridine Calcium Channel Blocker Therapy
Cumhuriyet Tıp Dergisi Cumhuriyet Tıp Derg 2014; 36: 19-24 Cumhuriyet Medical Journal Cumhuriyet Med J 2014; 36: 19-24 Original research-Orijinal araştırma http://dx.doi.org/10.7197/1305-0028.2102 A different dihydropyridine calcium channel blocker in hypertensive patients who developed pedal edema on dihydropyridine calcium channel blocker therapy Dihidropiridin grubu bir kalsiyum kanal blokeri tedavisi sırasında ayak bileği ödemi gelişen hipertansif hastalarda farklı bir dihidropiridin kalsiyum kanal blokerinin kullanımı Ayşe Yüksel, Ahmet Karagöz*, Özgül Uçar, Abdullah Çelik, Sinan Aydoğdu Department of Cardiology (A. Yüksel, MD), Abdurrahman Yurtaslan Oncology Education and Research Hospital, TR-06200 Ankara, Department of Cardiology (Assist Prof. A. Karagöz, MD), Giresun University, 28200, Giresun, Cardiovascular Surgery Clinic, (A. Çelik, MD), Giresun Professor Doctor Atilla İlhan Özdemir State Hospital, TR-28100 Giresun, Department of Cardiology (Assoc. Prof. Ö. Uçar, MD), Ankara Numune Education and Research Hospital, TR- 06230 Ankara, Department of Cardiology (Prof. S. Aydoğdu, MD), Yüksek İhtisas Education and Research Hospital, TR-06100 Ankara Abstract Aim. Dihydropyridine calcium channel blockers (CCB) are widely preferred for the treatment of hypertension for their efficacy, metabolic neutrality and low side effect profile. However pedal edema formation limits their usage. The aim of the present study is to evaluate the incidence of pedal edema formation with a different dihydropyridine CCB in hypertensive patients who developed pedal edema during a dihydropyridine CCB therapy. Method. Fifty-eight hypertensive patients (34 female, 24 male, mean age: 65.3±10.5) in whom pedal edema developed during treatment with a dihydropyridine CCB (amlodipine 10mg/day in 40 patients, amlodipine 5mg/day in 14 patients, nifedipine GITS 30mg/day in 4 patients) were enrolled. -

Lercanidipine Vs Lacidipine in Isolated Systolic Hypertension
Journal of Human Hypertension (2003) 17, 799–806 & 2003 Nature Publishing Group All rights reserved 0950-9240/03 $25.00 www.nature.com/jhh ORIGINAL ARTICLE Lercanidipine vs lacidipine in isolated systolic hypertension M Millar-Craig1, B Shaffu2, A Greenough3, L Mitchell3 and C McDonald3 1Department of Cardiology, Derbyshire Royal Infirmary, London Road, Derby, UK; 2Station Road Surgery, 152 Station Road, Wigston, Leicester, UK; 3Napp Pharmaceuticals Limited, Cambridge Science Park, Milton Road, Cambridge, UK This randomised, double-blind, double-dummy, parallel blood pressure was À0.81 (À4.45, 2.84) mmHg. These group, multicentre study compared the efficacy and confidence intervals were within the limits specified for tolerability of lercanidipine with lacidipine. Elderly equivalence, that is, (À5, 5) mmHg. Ambulatory blood patients with isolated systolic hypertension (supine pressure monitoring showed that the antihypertensive blood pressure X160/o95 mmHg) were enrolled and effects of both drugs lasted for the full 24-h dosing underwent a placebo run-in period of 14–27 days before period and followed a circadian pattern. Both treatments random allocation to lercanidipine tablets 10 mg once were well tolerated with a low incidence of adverse drug daily (n ¼ 111) or lacidipine tablets 2 mg once daily reactions and a low withdrawal rate. Significantly fewer (n ¼ 111) for the assessment period (112–160 days). patients withdrew from treatment with lercanidipine Titration to lercanidipine 20 mg once daily (two 10 mg (P ¼ 0.015). Neither treatment had any clinically signifi- tablets) or lacidipine 4 mg once daily (two 2 mg tablets) cant effect on pulse rate or cardiac conduction. -

List of Vital Essential and Necessary Drugs and Medical Sundries For
LIST OF VITAL ESSENTIAL AND NECESSARY DRUGS AND 2015 MEDICAL SUNDRIES FOR PUBLIC HEALTH INSTITUTIONS Sixth Edition STANDARDS & REGULATION DIVISION JAMAICA List of Vital Essential and Necessary List of Drugs and Medical Sundries for Public Institutions List of Vital Essential and Necessary List of Drugs and Medical Sundries for Public Institutions CONTENTS CONTENTS Contd. Page Preface 5-6 Page Information on Hospitals and Health Centres 7 Explanatory Notes 8 Medical Sundries 69-73 Prescription Writing 9-10 Dental Supplies 74 Algorithm for Treatment of Hypertension 11-12 Radiotherapy – Diagnostic Agents 75 Algorithm for Management of Type 2 Diabetes 13-14 Raw Materials 76 List of Drugs Designated for NHF 15-17 List of Drugs Designated for JADEP 18 VOLUME11 – SPECIALIST LIST 77 VOLUME 1 – GENERAL LIST 19 CLASSIFICATION OF DRUGS SECTION 1. Cardiovascular System 78 CLASSIFICATION OF DRUGS SECTION 2. Central Nervous System 79 SECTION 1. Cardiovascular System 20-24 SECTION 3. Dermatology 80 SECTION 2. Central Nervous System 25-30 SECTION 4. Endocrine System 80 SECTION 3. Dermatology 31-33 SECTION 5. Gastro-intestinal System 81 SECTION 4. Ear, Nose and Oropharynx 34-35 SECTION 6. Infections 81 SECTION 5. Endocrine System 36-38 SECTION 7. Malignant Disease and SECTION 6. Gastro-intestinal System 39-40 Immunosuppression 82 SECTION 7. Infections 41-46 SECTION 8. Musculoskeletal and Joint Diseases 83 SECTION 8. Malignant Disease and SECTION 9. Ophthalmology 83 Immunosuppression 47-49 SECTION 10. Genito-Urinary Tract Disorders 84 SECTION 9. Musculoskeletal and Joint Diseases 50-51 SECTION 11. Respiratory System 84 SECTION 10. Nutrition and Blood 52-54 SECTION 12. -

II~ R#I:C44kpu:Frt# PHILIPPINE HEALTH INSURANCE CORPORATION !I City State Centre Building # 709 Shaw Boulevard, Pasig City I Tel
II~ R#i:c44kPU:frt# PHILIPPINE HEALTH INSURANCE CORPORATION !I City State Centre Building # 709 Shaw Boulevard, Pasig City I Tel. 637-9999,637-6262 October 24, 2000 I PHILHEALTH CIRCULAR I No. 030, s-2000 '~ TO ALL MEMBERS OF THE NATIONAL HEJ;LTI-I INSURANCE PROGRAM, ACCREDITED INSTITUTIO:tjJAL AND I PROFESSIONAL HEALTH CARE PROVIIDERS, REGION},_L I HEALTH INSUM~CE OFFICES, CLAIM$ PROCESSING I DEPAKfMENTS IN THE CENTP.... AL OFdCE AND ALL OTHERS CONCERl~ED SUBJECT: List of additional rei11l.burseablc dtugs Ul.clud:ing over-the-counter I I drugs, found in the Philippine National Drug IFormularv I . II THE Philippme Health Insurance Corporation (Phill-lealth) has approved ~he following drugs for mclusion m Phili-Iealth's Positive List. These drugs can be found m the Clinical Practice Guidelines I (CPGs) for Hypertension, Urinary Tract Infection and Pneumonia. Claims ~or Medicare refund for I these drugs will be reimbursed only when used in the treatment of the disease1 indicated in the CPGs: I I DRUG CPG PREfARATION 1. Benazepril Hcl Hypertension Tablet 2. Bisoprolol Hypertension Tablet I 3. Cilazapril Hypertension Tablet 4. Doxazosin Hypertension Tablet 5.1sradipine Hypertension Tablet I 6. Lacidipine Hypertension i Tablet 7. Manidipine Hcl Hypertension Tablet 8. Perindopril Hypertension Tablet I 9. Quinapril Hypertension Tablet 10. Ramipril Hypertension Tablet 11. Delapril Hypertension Tablet I 12. Lisinopril Hypertension Tablet 13. Carteolol Hypertension Tablet 14. Oxprenolol Hypertension Tablet 15. Pindolol Hypertension Tablet ! I 16. Guanfacine Hypertension Tablet 17. Sodium Nitroprusside Hypertension Tablet 18. Nitrendipine Hypertension Tablet I Pneumonia O.!D-2.0g Vial 19. Cefamandole I 20. -

PACKAGE LEAFLET: INFORMATION for the USER Lacidipine 2 Mg Film-Coated Tablets Lacidipine 4 Mg Film-Coated Tablets Lacidipine
PACKAGE LEAFLET: INFORMATION FOR THE USER Lacidipine 2 mg film-coated tablets Lacidipine 4 mg film-coated tablets Lacidipine 6 mg film-coated tablets lacidipine Read all of this leaflet carefully before you start using this medicine. Keep this leaflet. You may need to read it again. If you have any further questions, ask your doctor or pharmacist. This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their symptoms are the same as yours. If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet (see Section 4) In this leaflet: 1. What Lacidipine tablets are and what they are used for 2. Before you take Lacidipine tablets 3. How to take Lacidipine tablets 4. Possible side effects 5. How to store Lacidipine tablets 6.Contents of the pack and other information 1. WHAT LACIDIPINE TABLETS ARE AND WHAT THEY ARE USED FOR Lacidipine tablets contains a medicine called lacidipine. This belongs to a group of medicines called ‘calcium channels blockers’. Lacidipine tablets helps to relax your blood vessels so that they get wider. This helps the blood to flow more easily and lowers the blood pressure. Lacidipine tablets taken regularly as prescribed by your doctor will help to lower your blood pressure (to treat hypertension). 2. WHAT YOU NEED TO KNOW BEFORE YOU TAKE LACIDIPINE TABLETS Do not take Lacidipine tablets: If you are allergic (hypersensitive) to lacidipine, other calcium channel blocker medicines or any of the other ingredients of lacidipine tablets (See section 6: Further information). -

Screening of 300 Drugs in Blood Utilizing Second Generation
Forensic Screening of 300 Drugs in Blood Utilizing Exactive Plus High-Resolution Accurate Mass Spectrometer and ExactFinder Software Kristine Van Natta, Marta Kozak, Xiang He Forensic Toxicology use Only Drugs analyzed Compound Compound Compound Atazanavir Efavirenz Pyrilamine Chlorpropamide Haloperidol Tolbutamide 1-(3-Chlorophenyl)piperazine Des(2-hydroxyethyl)opipramol Pentazocine Atenolol EMDP Quinidine Chlorprothixene Hydrocodone Tramadol 10-hydroxycarbazepine Desalkylflurazepam Perimetazine Atropine Ephedrine Quinine Cilazapril Hydromorphone Trazodone 5-(p-Methylphenyl)-5-phenylhydantoin Desipramine Phenacetin Benperidol Escitalopram Quinupramine Cinchonine Hydroquinine Triazolam 6-Acetylcodeine Desmethylcitalopram Phenazone Benzoylecgonine Esmolol Ranitidine Cinnarizine Hydroxychloroquine Trifluoperazine Bepridil Estazolam Reserpine 6-Monoacetylmorphine Desmethylcitalopram Phencyclidine Cisapride HydroxyItraconazole Trifluperidol Betaxolol Ethyl Loflazepate Risperidone 7(2,3dihydroxypropyl)Theophylline Desmethylclozapine Phenylbutazone Clenbuterol Hydroxyzine Triflupromazine Bezafibrate Ethylamphetamine Ritonavir 7-Aminoclonazepam Desmethyldoxepin Pholcodine Clobazam Ibogaine Trihexyphenidyl Biperiden Etifoxine Ropivacaine 7-Aminoflunitrazepam Desmethylmirtazapine Pimozide Clofibrate Imatinib Trimeprazine Bisoprolol Etodolac Rufinamide 9-hydroxy-risperidone Desmethylnefopam Pindolol Clomethiazole Imipramine Trimetazidine Bromazepam Felbamate Secobarbital Clomipramine Indalpine Trimethoprim Acepromazine Desmethyltramadol Pipamperone -

Drugs for Primary Prevention of Atherosclerotic Cardiovascular Disease: an Overview of Systematic Reviews
Supplementary Online Content Karmali KN, Lloyd-Jones DM, Berendsen MA, et al. Drugs for primary prevention of atherosclerotic cardiovascular disease: an overview of systematic reviews. JAMA Cardiol. Published online April 27, 2016. doi:10.1001/jamacardio.2016.0218. eAppendix 1. Search Documentation Details eAppendix 2. Background, Methods, and Results of Systematic Review of Combination Drug Therapy to Evaluate for Potential Interaction of Effects eAppendix 3. PRISMA Flow Charts for Each Drug Class and Detailed Systematic Review Characteristics and Summary of Included Systematic Reviews and Meta-analyses eAppendix 4. List of Excluded Studies and Reasons for Exclusion This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. 1 Downloaded From: https://jamanetwork.com/ on 09/28/2021 eAppendix 1. Search Documentation Details. Database Organizing body Purpose Pros Cons Cochrane Cochrane Library in Database of all available -Curated by the Cochrane -Content is limited to Database of the United Kingdom systematic reviews and Collaboration reviews completed Systematic (UK) protocols published by by the Cochrane Reviews the Cochrane -Only systematic reviews Collaboration Collaboration and systematic review protocols Database of National Health Collection of structured -Curated by Centre for -Only provides Abstracts of Services (NHS) abstracts and Reviews and Dissemination structured abstracts Reviews of Centre for Reviews bibliographic -

Package Leaflet: Information for the User Lacidipine Teva 2 Mg Film-Coated Tablets Lacidipine Teva 4 Mg Film-Coated Tablets Laci
Lacidipine, NL/H/2974/01-02/DC, 03.03.20 Package leaflet: Information for the user Lacidipine Teva 2 mg film-coated tablets Lacidipine Teva 4 mg film-coated tablets lacidipine Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor, pharmacist or nurse. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Lacidipine Teva is and what it is used for 2. What you need to know before you take Lacidipine Teva 3. How to take Lacidipine Teva 4. Possible side effects 5. How to store Lacidipine Teva 6. Contents of the pack and other information 1. What Lacidipine Teva is and what it is used for Lacidipine Teva contains a medicine called lacidipine. This belongs to a group of medicines called ‘calcium channel blockers’. Lacidipine Teva helps to relax your blood vessels so that they get wider. This helps the blood to flow more easily and lowers the blood pressure. Lacidipine Teva tablets taken regularly as prescribed by your doctor will help to lower your blood pressure (to treat hypertension). 2. What you need to know before you take Lacidipine Teva Do not take Lacidipine Teva - If you are allergic to lacidipine, other calcium channel blocker medicines or any of the other ingredients of this medicine(listed in section 6). -
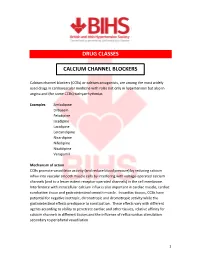
Calcium Channel Blockers (Ccbs)
DRUG CLASSES CALCIUM CHANNEL BLOCKERS Calcium channel blockers (CCBs) or calcium antagonists, are among the most widely used drugs in cardiovascular medicine with roles not only in hypertension but also in angina and (for some CCBs) tachyarrhythmias. Examples Amlodipine Diltiazem Felodipine Isradipine Lacidipine Lercanidipine Nicardipine Nifedipine Nisoldipine Verapamil Mechanism of action CCBs promote vasodilator activity (and reduce blood pressure) by reducing calcium influx into vascular smooth muscle cells by interfering with voltage-operated calcium channels (and to a lesser extent receptor-operated channels) in the cell membrane. Interference with intracellular calcium influx is also important in cardiac muscle, cardiac conduction tissue and gastrointestinal smooth muscle. In cardiac tissues, CCBs have potential for negative inotropic, chronotropic and dromotropic activity while the gastrointestinal effects predispose to constipation. These effects vary with different agents according to ability to penetrate cardiac and other tissues, relative affinity for calcium channels in different tissues and the influence of reflux cardiac stimulation secondary to peripheral vasodilation. 1 Although often considered as a single class, CCBs can be subdivided according to structural and functional distinctions. Dihydropyridine derivates : amlodipine, felodipine, isradipine, lacidipine, lercanidipine, nicardipine, nifedipine, nisoldipine Phenylalkylamine : verapamil Benzothiazepine derivative : diltiazem Dihydropyridine derivatives have pronounced