Pediatric Respirology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Newsletter Editor: Yoichi Nakanishi Associate Editors: Yoshinosuke Fukuchi, David CL Lam, Suga Konno
Vol.30, No.1 (January 2021) Newsletter Editor: Yoichi Nakanishi Associate Editors: Yoshinosuke Fukuchi, David CL Lam, Suga Konno Message from the President A Happy New Year to all APSR members. Last year was a year of COVID-19. The APSR was also influenced by the disease, and the APSR 2020 Congress in Kyoto was postponed to 2021. I would express sincere appreciation to the Japanese Local Congress Committee team for their tremendous efforts to re-arrange the Congress, and also to the Korean Local Congress Committee team for their kind acceptance of postponement of the APSR Congress in Seoul to 2022. Under this difficult situation, we should not stagnate scientific progress and educational activities. We have held two COVID-19 webinars, three APSR virtual meetings, an ATS-APSR joint webinar, joint symposia with the Philippine College of Chest Physicians (PCCP), the Malaysian Thoracic Society (MTS) and the Taiwan Society of Pulmonary and Critical Care Medicine (TSPCCM). It is a great pleasure that many APSR members joined these web meetings and all of them were so successful. I am profoundly grateful to the Central Congress Committee members, Assembly members, presenters, facilitators, audiences, en bloc members, sponsors and the APSR secretariat office. The Asia-Pacific region has the biggest population in the world and is accomplishing rapid development, though it still has many health problems such as air pollution, tobacco smoking, respiratory infection including tuberculosis, and poor medical infrastructure. We are happy to have lots of projects to solve these problems. This year, we are going to further enhance our activities in order to achieve our objectives, i.e., “The advancement and promotion of knowledge of the respiratory system in health and disease, which strives to encourage research, improve clinical practice through teaching, increase awareness of health problems in the area and promote the exchange of knowledge among respirologists in the Asia-Pacific region”. -

Welcome to the Central Bank of China
399 INSURED FINANCIAL INSTITUTIONS 2020/5/31 37 Insured Domestic Banks 5 Sanchong City Farmers' Association of New Taipei City 62 Hengshan District Farmers' Association of Hsinchu County 1 Bank of Taiwan 13 BNP Paribas 6 Banciao City Farmers' Association of New Taipei City 63 Sinfong Township Farmers' Association of Hsinchu County 2 Land Bank of Taiwan 14 Standard Chartered Bank 7 Danshuei Township Farmers' Association of New Taipei City 64 Miaoli City Farmers' Association of Miaoli County 3 Taiwan Cooperative Bank 15 Oversea-Chinese Banking Corporation 8 Shulin City Farmers' Association of New Taipei City 65 Jhunan Township Farmers' Association of Miaoli County 4 First Commercial Bank 16 Credit Agricole Corporate and Investment Bank 9 Yingge Township Farmers' Association of New Taipei City 66 Tongsiao Township Farmers' Association of Miaoli County 5 Hua Nan Commercial Bank 17 UBS AG 10 Sansia Township Farmers' Association of New Taipei City 67 Yuanli Township Farmers' Association of Miaoli County 6 Chang Hwa Commercial Bank 18 ING BANK, N. V. 11 Sinjhuang City Farmers' Association of New Taipei City 68 Houlong Township Farmers' Association of Miaoli County 7 Citibank Taiwan 19 Australia and New Zealand Bank 12 Sijhih City Farmers' Association of New Taipei City 69 Jhuolan Township Farmers' Association of Miaoli County 8 The Shanghai Commercial & Savings Bank 20 Wells Fargo Bank 13 Tucheng City Farmers' Association of New Taipei City 70 Sihu Township Farmers' Association of Miaoli County 9 Taipei Fubon Commercial Bank 21 MUFG Bank 14 -

2020 MEC SUPPLIER DISCLOSURE LIST in 2008, MEC Made a Commitment to Its Members to Disclose the Names and Addresses of Factories That Manufacture MEC Label Products
2020 MEC SUPPLIER DISCLOSURE LIST In 2008, MEC made a commitment to its members to disclose the names and addresses of factories that manufacture MEC Label products. We rely on our supply chain partners to commit and adopt MEC's social compliance policy and supplier code of conduct. To drive meaningful change, we understand that we need to work with our supply chain partners to meet the requirements set out in our policies. Listed product manufacturers (tier 1) represent 100% of our finished good supply chain. In an effort to continue MEC’s journey into supply chain transparency, MEC has added our Tier 1 subcontractor supply chain and our material supply-chain partners to the supplier disclosure list in September 2017. It is our commitment to our members that we will continue to disclose our supply chain partners; working to expand this list to include trims, component and subcomponent manufacturers. This list was last updated in January 2020. MEC updates its supplier list twice a year. This list fluctuates over time to reflect changes in product seasonality and our supplier base. PRODUCT MANUFACTURERS (Tier 1): FACTORY NAME | VENDOR NAME FACTORY ADDRESS CITY PROVINCE/STATE Komperdell Sportartikel Gesmbh Wagnermuhle 30 Mondsee Upper Austria CPCG International Co., Ltd. | Palace Group Phum Chhok, Khum Kok Rovieng, Sruk Chhoeung Brey Kampong Cham Kampong Cham Sun Grace Glove Cambodia Co., Ltd. Phum Prek Treng, Khum Samraong Thom Kean Svay District Kandal All Card 765 Boxwood Drive Cambridge Ontario BBS Pro Services Inc. No. 270 19358 96th Avenue Surrey British Columbia AK TECH CO.,LTD Vellage Po Sin, Town Lilin, New Zone ZhongKai Huizhou Guangdong Bellmart Kingtai Industrial Xiamen | Great King Group 4th and 5th Floor, No. -

Website : the Bank Website
Website : http://newmaps.twse.com.tw The Bank Website : http://www.landbank.com.tw Time of Publication : July 2018 Spokesman Name: He,Ying-Ming Title: Executive Vice President Tel: (02)2348-3366 E-Mail: [email protected] First Substitute Spokesman Name: Chu,Yu-Feng Title: Executive Vice President Tel: (02) 2348-3686 E-Mail: [email protected] Second Substitute Spokesman Name: Huang,Cheng-Ching Title: Executive Vice President Tel: (02) 2348-3555 E-Mail: [email protected] Address &Tel of the bank’s head office and Branches(please refer to’’ Directory of Head Office and Branches’’) Credit rating agencies Name: Moody’s Investors Service Address: 24/F One Pacific Place 88 Queensway Admiralty, Hong Kong. Tel: (852)3758-1330 Fax: (852)3758-1631 Web Site: http://www.moodys.com Name: Standard & Poor’s Corp. Address: Unit 6901, level 69, International Commerce Centre 1 Austin Road West Kowloon, Hong Kong Tel: (852)2841-1030 Fax: (852)2537-6005 Web Site: http://www.standardandpoors.com Name: Taiwan Ratings Corporation Address: 49F., No7, Sec.5, Xinyi Rd., Xinyi Dist., Taipei City 11049, Taiwan (R.O.C) Tel: (886)2-8722-5800 Fax: (886)2-8722-5879 Web Site: http://www.taiwanratings.com Stock transfer agency Name: Secretariat land bank of Taiwan Co., Ltd. Address: 3F, No.53, Huaining St. Zhongzheng Dist., Taipei City 10046, Taiwan(R,O,C) Tel: (886)2-2348-3456 Fax: (886)2-2375-7023 Web Site: http://www.landbank.com.tw Certified Publick Accountants of financial statements for the past year Name of attesting CPAs: Gau,Wey-Chuan, Mei,Ynan-Chen Name of Accounting Firm: KPMG Addres: 68F., No.7, Sec.5 ,Xinyi Rd., Xinyi Dist., Taipei City 11049, Taiwan (R.O.C) Tel: (886)2-8101-6666 Fax: (886)2-8101-6667 Web Site: http://www.kpmg.com.tw The Bank’s Website: http://www.landbank.com.tw Website: http://newmaps.twse.com.tw The Bank Website: http://www.landbank.com.tw Time of Publication: July 2018 Land Bank of Taiwan Annual Report 2017 Publisher: Land Bank of Taiwan Co., Ltd. -

Scientific Publications in Respiratory Journals from Chinese
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2013-004201 on 28 February 2014. Downloaded from Scientific publications in respiratory journals from Chinese authors in various parts of North Asia: a 10-year survey of literature Bo Ye,1 Ting-Ting Du,1 Ting Xie,2 Jun-Tao Ji,1 Zhao-Hong Zheng,1 Zhuan Liao,1 Liang-Hao Hu,1 Zhao-Shen Li1 To cite: Ye B, Du T-T, Xie T, ABSTRACT et al Strengths and limitations of this study . Scientific publications in Objectives: Respiratory disease remains one of the respiratory journals from leading causes of morbidity and mortality in China. Chinese authors in various A few journals covered resources beyond respiratory However, little is known about the research status of parts of North Asia: a 10-year even selected from the respiratory system of Science — survey of literature. BMJ Open respirology in three major regions of China Mainland Citation Index Expanded (SCIE). Besides, some 2014;4:e004201. doi:10.1136/ (ML), Hong Kong (HK) and Taiwan (TW). A 10-year related journals not shown in SCIE were not col- bmjopen-2013-004201 survey of literature was conducted to compare the lected. Some respiratory medicine research articles three regions’ outputs in the research of respirology. were published in general journals, rather than in the ▸ Prepublication history for Design: A bibliometric study. specialized ones. Searching by the author’s address this paper is available online. Setting: China. (China, HK or TW) led to another problem that the To view these files please Participants and outcome measures: A literature articles which addressed other cities or provinces visit the journal online search in PubMed database, updated as of September were not included. -
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total Journals: 8631
SCIENCE CITATION INDEX EXPANDED - JOURNAL LIST Total journals: 8631 1. 4OR-A QUARTERLY JOURNAL OF OPERATIONS RESEARCH 2. AAPG BULLETIN 3. AAPS JOURNAL 4. AAPS PHARMSCITECH 5. AATCC REVIEW 6. ABDOMINAL IMAGING 7. ABHANDLUNGEN AUS DEM MATHEMATISCHEN SEMINAR DER UNIVERSITAT HAMBURG 8. ABSTRACT AND APPLIED ANALYSIS 9. ABSTRACTS OF PAPERS OF THE AMERICAN CHEMICAL SOCIETY 10. ACADEMIC EMERGENCY MEDICINE 11. ACADEMIC MEDICINE 12. ACADEMIC PEDIATRICS 13. ACADEMIC RADIOLOGY 14. ACCOUNTABILITY IN RESEARCH-POLICIES AND QUALITY ASSURANCE 15. ACCOUNTS OF CHEMICAL RESEARCH 16. ACCREDITATION AND QUALITY ASSURANCE 17. ACI MATERIALS JOURNAL 18. ACI STRUCTURAL JOURNAL 19. ACM COMPUTING SURVEYS 20. ACM JOURNAL ON EMERGING TECHNOLOGIES IN COMPUTING SYSTEMS 21. ACM SIGCOMM COMPUTER COMMUNICATION REVIEW 22. ACM SIGPLAN NOTICES 23. ACM TRANSACTIONS ON ALGORITHMS 24. ACM TRANSACTIONS ON APPLIED PERCEPTION 25. ACM TRANSACTIONS ON ARCHITECTURE AND CODE OPTIMIZATION 26. ACM TRANSACTIONS ON AUTONOMOUS AND ADAPTIVE SYSTEMS 27. ACM TRANSACTIONS ON COMPUTATIONAL LOGIC 28. ACM TRANSACTIONS ON COMPUTER SYSTEMS 29. ACM TRANSACTIONS ON COMPUTER-HUMAN INTERACTION 30. ACM TRANSACTIONS ON DATABASE SYSTEMS 31. ACM TRANSACTIONS ON DESIGN AUTOMATION OF ELECTRONIC SYSTEMS 32. ACM TRANSACTIONS ON EMBEDDED COMPUTING SYSTEMS 33. ACM TRANSACTIONS ON GRAPHICS 34. ACM TRANSACTIONS ON INFORMATION AND SYSTEM SECURITY 35. ACM TRANSACTIONS ON INFORMATION SYSTEMS 36. ACM TRANSACTIONS ON INTELLIGENT SYSTEMS AND TECHNOLOGY 37. ACM TRANSACTIONS ON INTERNET TECHNOLOGY 38. ACM TRANSACTIONS ON KNOWLEDGE DISCOVERY FROM DATA 39. ACM TRANSACTIONS ON MATHEMATICAL SOFTWARE 40. ACM TRANSACTIONS ON MODELING AND COMPUTER SIMULATION 41. ACM TRANSACTIONS ON MULTIMEDIA COMPUTING COMMUNICATIONS AND APPLICATIONS 42. ACM TRANSACTIONS ON PROGRAMMING LANGUAGES AND SYSTEMS 43. ACM TRANSACTIONS ON RECONFIGURABLE TECHNOLOGY AND SYSTEMS 44. -

List of Insured Financial Institutions (PDF)
401 INSURED FINANCIAL INSTITUTIONS 2021/5/31 39 Insured Domestic Banks 5 Sanchong City Farmers' Association of New Taipei City 62 Hengshan District Farmers' Association of Hsinchu County 1 Bank of Taiwan 13 BNP Paribas 6 Banciao City Farmers' Association of New Taipei City 63 Sinfong Township Farmers' Association of Hsinchu County 2 Land Bank of Taiwan 14 Standard Chartered Bank 7 Danshuei Township Farmers' Association of New Taipei City 64 Miaoli City Farmers' Association of Miaoli County 3 Taiwan Cooperative Bank 15 Oversea-Chinese Banking Corporation 8 Shulin City Farmers' Association of New Taipei City 65 Jhunan Township Farmers' Association of Miaoli County 4 First Commercial Bank 16 Credit Agricole Corporate and Investment Bank 9 Yingge Township Farmers' Association of New Taipei City 66 Tongsiao Township Farmers' Association of Miaoli County 5 Hua Nan Commercial Bank 17 UBS AG 10 Sansia Township Farmers' Association of New Taipei City 67 Yuanli Township Farmers' Association of Miaoli County 6 Chang Hwa Commercial Bank 18 ING BANK, N. V. 11 Sinjhuang City Farmers' Association of New Taipei City 68 Houlong Township Farmers' Association of Miaoli County 7 Citibank Taiwan 19 Australia and New Zealand Bank 12 Sijhih City Farmers' Association of New Taipei City 69 Jhuolan Township Farmers' Association of Miaoli County 8 The Shanghai Commercial & Savings Bank 20 Wells Fargo Bank 13 Tucheng City Farmers' Association of New Taipei City 70 Sihu Township Farmers' Association of Miaoli County 9 Taipei Fubon Commercial Bank 21 MUFG Bank 14 -
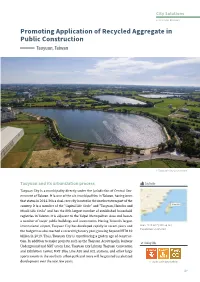
Promoting Application of Recycled Aggregate in Public Construction Taoyuan, Taiwan
City Solutions 2-3 Circular Economy Promoting Application of Recycled Aggregate in Public Construction Taoyuan, Taiwan © Taoyuan City Government City Profile Taoyuan and its urbanization process Taoyuan City is a municipality directly under the jurisdiction of Central Gov- ernment of Taiwan. It is one of the six municipalities in Taiwan, having been country. It is a member of the "Capital Life Circle" and "Taoyuan, Hsinchu and Taoyuan City that status in 2014. It is a dual-core city located in the northwestern part of the registries in Taiwan. It is adjacent to the Taipei Metropolitan Area and boasts Miaoli Life Circle" and has the fifth-largest number of established household a number of major public buildings and investments. Having Taiwan's largest international airport, Taoyuan City has developed rapidly in recent years and Area: 1,140 km² (440 sq mi) Population: 2,245,059 the budget has also reached a record high every year, growing beyond NTD110 - tion. In addition to major projects such as the Taoyuan Aerotropolis, Railway billion in 2019. Thus, Taoyuan City is experiencing a golden age of construc Linking SDGs Underground and MRT Green Line, Taoyuan City Library, Taoyuan Convention and Exhibition Center, MRT Blue Line A20 and A21 stations, and other large sports events in the southern urban park and more will be granted accelerated development over the next few years. © sdg knowledge platform 119 City Solutions 2-3 Circular Economy Engineering organizations and environmental protection agencies often Project Duration: From July -

Welcome to the Central Bank of China
400 INSURED FINANCIAL INSTITUTIONS 2020/12/31 38 Insured Domestic Banks 5 Sanchong City Farmers' Association of New Taipei City 62 Hengshan District Farmers' Association of Hsinchu County 1 Bank of Taiwan 13 BNP Paribas 6 Banciao City Farmers' Association of New Taipei City 63 Sinfong Township Farmers' Association of Hsinchu County 2 Land Bank of Taiwan 14 Standard Chartered Bank 7 Danshuei Township Farmers' Association of New Taipei City 64 Miaoli City Farmers' Association of Miaoli County 3 Taiwan Cooperative Bank 15 Oversea-Chinese Banking Corporation 8 Shulin City Farmers' Association of New Taipei City 65 Jhunan Township Farmers' Association of Miaoli County 4 First Commercial Bank 16 Credit Agricole Corporate and Investment Bank 9 Yingge Township Farmers' Association of New Taipei City 66 Tongsiao Township Farmers' Association of Miaoli County 5 Hua Nan Commercial Bank 17 UBS AG 10 Sansia Township Farmers' Association of New Taipei City 67 Yuanli Township Farmers' Association of Miaoli County 6 Chang Hwa Commercial Bank 18 ING BANK, N. V. 11 Sinjhuang City Farmers' Association of New Taipei City 68 Houlong Township Farmers' Association of Miaoli County 7 Citibank Taiwan 19 Australia and New Zealand Bank 12 Sijhih City Farmers' Association of New Taipei City 69 Jhuolan Township Farmers' Association of Miaoli County 8 The Shanghai Commercial & Savings Bank 20 Wells Fargo Bank 13 Tucheng City Farmers' Association of New Taipei City 70 Sihu Township Farmers' Association of Miaoli County 9 Taipei Fubon Commercial Bank 21 MUFG Bank 14 -

Interstitial Pneumonia with Autoimmune Features: Why Rheumatologist-Pulmonologist Collaboration Is Essential
biomedicines Review Interstitial Pneumonia with Autoimmune Features: Why Rheumatologist-Pulmonologist Collaboration Is Essential Marco Sebastiani 1 , Paola Faverio 2, Andreina Manfredi 1, Giulia Cassone 1 , Caterina Vacchi 1, Anna Stainer 2, Maria Rosa Pozzi 3, Carlo Salvarani 1,4, Alberto Pesci 2 and Fabrizio Luppi 2,* 1 Rheumatology Unit, University of Modena and Reggio Emilia, Azienda Ospedaliero-Universitaria Policlinico di Modena, 41124 Modena, Italy; [email protected] (M.S.); [email protected] (A.M.); [email protected] (G.C.); [email protected] (C.V.); [email protected] (C.S.) 2 Respiratory Unit, San Gerardo Hospital, Department of Medicine and Surgery, University of Milan-Bicocca, 20900 Monza, Italy; [email protected] (P.F.); [email protected] (A.S.); [email protected] (A.P.) 3 Rheumatology Unit, San Gerardo Hospital, 20900 Monza, Italy; [email protected] 4 Rheumatology Unit, Dipartimento Medicina Interna e Specialità Mediche, Azienda Unità Sanitaria Locale di Reggio Emilia—Istituto di Ricerca e Cura a Carattere Scientifico, 42123 Reggio Emilia, Italy * Correspondence: [email protected]; Tel.: +39-0392339373; Fax: +39-0392336660 Abstract: In 2015 the European Respiratory Society (ERS) and the American Thoracic Society (ATS) “Task Force on Undifferentiated Forms of Connective Tissue Disease-associated Interstitial Lung Disease” proposed classification criteria for a new research category defined as “Interstitial Pneumo- nia with Autoimmune Features” (IPAF), to uniformly define patients with interstitial lung disease (ILD) and features of autoimmunity, without a definite connective tissue disease. These classification criteria were based on a variable combination of features obtained from three domains: a clinical domain consisting of extra-thoracic features, a serologic domain with specific autoantibodies, and a Citation: Sebastiani, M.; Faverio, P.; morphologic domain with imaging patterns, histopathological findings, or multicompartment in- Manfredi, A.; Cassone, G.; Vacchi, C.; volvement. -

(A2LA Cert. No. 3100.01) 03/19/2020 Page 1 of 4 SCOPE OF
SCOPE OF ACCREDITATION TO ISO/IEC 17025:2017 DEKRA TESTING AND CERTIFICATION CO., LTD 1 No.159, Sec. 2, Wenhua 1st Road, Linkou District New Taipei City 24457, TAIWAN (R.O.C.) Murphy Wang: [email protected] Phone: +886 2 2602 7968 ELECTRICAL Valid To: November 30, 2022 Certificate Number: 3100.01 In recognition of the successful completion of the A2LA evaluation process, accreditation is granted to this laboratory at the location listed above, as well as the four satellite laboratory locations listed below, to perform the following Electrical tests: Test: Test Method(s): Mobile Devices GSM/GPRS/EDGE ETSI EN 300 607-1; Protocol/Conformance/SIM/SAT/ EN 301 511; ETSI EN 301 511; A-GPS/IoT Connection Efficiency 3GPP TS 51.010-1; (excluding Radiated Spurious Emissions) ETSI TS 151.010-1; 3GPP TS 51.010-2; ETSI TS 151 010-2; 3GPP TS 51.010-4; ETSI TS 151 010-4; ETSI TS 102 230-1; GSMA PRD TS.35; NAPRD.03; GCF-CC WCDMA/UMTS/HSPA 3GPP TS 31.121; 3GPP TS 34.121-1; Protocol/Conformance/USIM/USAT/ 3GPP TS 31.124; A-GPS/IMS/IoT Connection Efficiency ETSI TS 134 121; (excluding Radiated Spurious Emissions) ETSI EN 301 908-2; EN 301 908-2; 3GPP TS 34.123-1; 3GPP TS 34.171; 3GPP TS 34.229-1; 3GPP TR 37.901; ETSI TS 102 230-1; GSMA PRD TS.35; NAPRD.03; GCF-CC (A2LA Cert. No. 3100.01) 03/19/2020 Page 1 of 4 Test: Test Method(s): Mobile Devices (cont.) LTE/FDD/TDD 3GPP TS 31.121; Protocol/Conformance/UE positioning/ 3GPP TS 31.124; IMS/IoT Connection Efficiency/ 3GPP TS 34.229-1; USIM/USAT 3GPP TS 36.521-1; (excluding Radiated Spurious Emissions) ETSI -

National Level Public Officials Election-Taiwan, 2020)
Election Result By Party Votes For The 7th Direct Presidential Election (National Level Public Officials Election-Taiwan, 2020) James C.Y.Soong、Yu Xiang (PFP) Daniel K.Y.Han、Chang Shan-Zheng (KMT) TSAI,ING-WEN、Lai Qing-De (DPP) Locality Valid Votes Votes % Votes % Votes % Grand Total 14300940 608590 4.26 5522119 38.61 8170231 57.13 Taiwan Province 4207385 179061 4.26 1709221 40.62 2319103 55.12 Ilan County 274406 10739 3.91 90010 32.80 173657 63.28 Hsinchu County 325039 18435 5.67 154224 47.45 152380 46.88 Miaoli County 326601 15222 4.66 164345 50.32 147034 45.02 Changhua County 763231 35060 4.59 291835 38.24 436336 57.17 Nantou County 299152 13315 4.45 133791 44.72 152046 50.83 Yunlin County 399788 15331 3.83 138341 34.60 246116 61.56 Chia-I County 307290 11138 3.62 98810 32.16 197342 64.22 Pingtung County 511050 14021 2.74 179353 35.10 317676 62.16 Taitung County 115668 4163 3.60 67413 58.28 44092 38.12 Hualien County 185212 6869 3.71 111834 60.38 66509 35.91 Penghu County 50904 2583 5.07 20911 41.08 27410 53.85 Keelung City 226204 11878 5.25 99360 43.93 114966 50.82 Hsinchu City 261102 14103 5.40 102725 39.34 144274 55.26 Chia-I City 161738 6204 3.84 56269 34.79 99265 61.37 Taipei City 1632453 70769 4.34 685830 42.01 875854 53.65 Kaohsiung City 1763826 55309 3.14 610896 34.63 1097621 62.23 New Taipei City 2466187 112620 4.57 959631 38.91 1393936 56.52 Taichung City 1698470 84800 4.99 646366 38.06 967304 56.95 Tainan City 1167248 41075 3.52 339702 29.10 786471 67.38 Taoyuan City 1311141 63132 4.82 529749 40.40 718260 54.78 Fuchien Province