Cranial Nerves
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MR Imaging of the Orbital Apex
J Korean Radiol Soc 2000;4 :26 9-0 6 1 6 MR Imaging of the Orbital Apex: An a to m y and Pat h o l o g y 1 Ho Kyu Lee, M.D., Chang Jin Kim, M.D.2, Hyosook Ahn, M.D.3, Ji Hoon Shin, M.D., Choong Gon Choi, M.D., Dae Chul Suh, M.D. The apex of the orbit is basically formed by the optic canal, the superior orbital fis- su r e , and their contents. Space-occupying lesions in this area can result in clinical d- eficits caused by compression of the optic nerve or extraocular muscles. Even vas c u l a r changes in the cavernous sinus can produce a direct mass effect and affect the orbit ap e x. When pathologic changes in this region is suspected, contrast-enhanced MR imaging with fat saturation is very useful. According to the anatomic regions from which the lesions arise, they can be classi- fied as belonging to one of five groups; lesions of the optic nerve-sheath complex, of the conal and intraconal spaces, of the extraconal space and bony orbit, of the cav- ernous sinus or diffuse. The characteristic MR findings of various orbital lesions will be described in this paper. Index words : Orbit, diseases Orbit, MR The apex of the orbit is a complex region which con- tains many nerves, vessels, soft tissues, and bony struc- Anatomy of the orbital apex tures such as the superior orbital fissure and the optic canal (1-3), and is likely to be involved in various dis- The orbital apex region consists of the optic nerve- eases (3). -

Gluteal Region-II
Gluteal Region-II Dr Garima Sehgal Associate Professor King George’s Medical University UP, Lucknow Structures in the Gluteal region • Bones & joints • Ligaments Thickest muscle • Muscles • Vessels • Nerves Thickest nerve • Bursae Learning Objectives By the end of this teaching session Gluteal region –II all the MBBS 1st year students must be able to: • Enumerate the nerves of gluteal region • Write a short note on nerves of gluteal region • Describe the location & relations of sciatic nerve in gluteal region • Enumerate the arteries of gluteal region • Write a short note on arteries of gluteal region • Enumerate the arteries taking part in trochanteric and cruciate anastomosis • Write a short note on trochanteric and cruciate anastomosis • Enumerate the structures passing through greater sciatic foramen • Enumerate the structures passing through lesser sciatic foramen • Enumerate the bursae in relation to gluteus maximus • Enumerate the structures deep to gluteus maximus • Discuss applied anatomy Nerves of Gluteal region (all nerves in gluteal region are branches of sacral plexus) Superior gluteal nerve (L4,L5, S1) Inferior gluteal nerve (L5, S1, S2) FROM DORSAL DIVISIONS Perforating cutaneous nerve (S2,S3) Nerve to quadratus femoris (L4,L5, S1) Nerve to obturator internus (L5, S1, S2) FROM VENTRAL DIVISIONS Pudendal nerve (S2,S3,S4) Sciatic nerve (L4,L5,S1,S2,S3) Posterior cutaneous nerve of thigh FROM BOTH DORSAL &VENTRAL (S1,S2) & (S2,S3) DIVISIONS 1. Superior Gluteal nerve (L4,L5,S1- dorsal division) 1 • Enters through the greater 3 sciatic foramen • Above piriformis 2 • Runs forwards between gluteus medius & gluteus minimus • SUPPLIES: 1. Gluteus medius 2. Gluteus minimus 3. Tensor fasciae latae 2. -

Cranial Nerve Palsy
Cranial Nerve Palsy What is a cranial nerve? Cranial nerves are nerves that lead directly from the brain to parts of our head, face, and trunk. There are 12 pairs of cranial nerves and some are involved in special senses (sight, smell, hearing, taste, feeling) while others control muscles and glands. Which cranial nerves pertain to the eyes? The second cranial nerve is called the optic nerve. It sends visual information from the eye to the brain. The third cranial nerve is called the oculomotor nerve. It is involved with eye movement, eyelid movement, and the function of the pupil and lens inside the eye. The fourth cranial nerve is called the trochlear nerve and the sixth cranial nerve is called the abducens nerve. They each innervate an eye muscle involved in eye movement. The fifth cranial nerve is called the trigeminal nerve. It provides facial touch sensation (including sensation on the eye). What is a cranial nerve palsy? A palsy is a lack of function of a nerve. A cranial nerve palsy may cause a complete or partial weakness or paralysis of the areas served by the affected nerve. In the case of a cranial nerve that has multiple functions (such as the oculomotor nerve), it is possible for a palsy to affect all of the various functions or only some of the functions of that nerve. What are some causes of a cranial nerve palsy? A cranial nerve palsy can occur due to a variety of causes. It can be congenital (present at birth), traumatic, or due to blood vessel disease (hypertension, diabetes, strokes, aneurysms, etc). -

Septation of the Sphenoid Sinus and Its Clinical Significance
1793 International Journal of Collaborative Research on Internal Medicine & Public Health Septation of the Sphenoid Sinus and its Clinical Significance Eldan Kapur 1* , Adnan Kapidžić 2, Amela Kulenović 1, Lana Sarajlić 2, Adis Šahinović 2, Maida Šahinović 3 1 Department of anatomy, Medical faculty, University of Sarajevo, Čekaluša 90, 71000 Sarajevo, Bosnia and Herzegovina 2 Clinic for otorhinolaryngology, Clinical centre University of Sarajevo, Bolnička 25, 71000 Sarajevo, Bosnia and Herzegovina 3 Department of histology and embriology, Medical faculty, University of Sarajevo, Čekaluša 90, 71000 Sarajevo, Bosnia and Herzegovina * Corresponding Author: Eldan Kapur, MD, PhD Department of anatomy, Medical faculty, University of Sarajevo, Bosnia and Herzegovina Email: [email protected] Phone: 033 66 55 49; 033 22 64 78 (ext. 136) Abstract Introduction: Sphenoid sinus is located in the body of sphenoid, closed with a thin plate of bone tissue that separates it from the important structures such as the optic nerve, optic chiasm, cavernous sinus, pituitary gland, and internal carotid artery. It is divided by one or more vertical septa that are often asymmetric. Because of its location and the relationships with important neurovascular and glandular structures, sphenoid sinus represents a great diagnostic and therapeutic challenge. Aim: The aim of this study was to assess the septation of the sphenoid sinus and relationship between the number and position of septa and internal carotid artery in the adult BH population. Participants and Methods: A retrospective study of the CT analysis of the paranasal sinuses in 200 patients (104 male, 96 female) were performed using Siemens Somatom Art with the following parameters: 130 mAs: 120 kV, Slice: 3 mm. -

Lab #23 Anal Triangle
THE BONY PELVIS AND ANAL TRIANGLE (Grant's Dissector [16th Ed.] pp. 141-145) TODAY’S GOALS: 1. Identify relevant bony features/landmarks on skeletal materials or pelvic models. 2. Identify the sacrotuberous and sacrospinous ligaments. 3. Describe the organization and divisions of the perineum into two triangles: anal triangle and urogenital triangle 4. Dissect the ischiorectal (ischioanal) fossa and define its boundaries. 5. Identify the inferior rectal nerve and artery, the pudendal (Alcock’s) canal and the external anal sphincter. DISSECTION NOTES: The perineum is the diamond-shaped area between the upper thighs and below the inferior pelvic aperture and pelvic diaphragm. It is divided anatomically into 2 triangles: the anal triangle and the urogenital (UG) triangle (Dissector p. 142, Fig. 5.2). The anal triangle is bounded by the tip of the coccyx, sacrotuberous ligaments, and a line connecting the right and left ischial tuberosities. It contains the anal canal, which pierced the levator ani muscle portion of the pelvic diaphragm. The urogenital triangle is bounded by the ischiopubic rami to the inferior surface of the pubic symphysis and a line connecting the right and left ischial tuberosities. This triangular space contains the urogenital (UG) diaphragm that transmits the urethra (in male) and urethra and vagina (in female). A. Anal Triangle Turn the cadaver into the prone position. Make skin incisions as on page 144, Fig. 5.4 of the Dissector. Reflect skin and superficial fascia of the gluteal region in one flap to expose the large gluteus maximus muscle. This muscle has proximal attachments to the posteromedial surface of the ilium, posterior surfaces of the sacrum and coccyx, and the sacrotuberous ligament. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

98796-Anatomy of the Orbit
Anatomy of the orbit Prof. Pia C Sundgren MD, PhD Department of Diagnostic Radiology, Clinical Sciences, Lund University, Sweden Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lay-out • brief overview of the basic anatomy of the orbit and its structures • the orbit is a complicated structure due to its embryological composition • high number of entities, and diseases due to its composition of ectoderm, surface ectoderm and mesoderm Recommend you to read for more details Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 3 x 3 Imaging technique 3 layers: - neuroectoderm (retina, iris, optic nerve) - surface ectoderm (lens) • CT and / or MR - mesoderm (vascular structures, sclera, choroid) •IOM plane 3 spaces: - pre-septal •thin slices extraconal - post-septal • axial and coronal projections intraconal • CT: soft tissue and bone windows 3 motor nerves: - occulomotor (III) • MR: T1 pre and post, T2, STIR, fat suppression, DWI (?) - trochlear (IV) - abducens (VI) Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Superior orbital fissure • cranial nerves (CN) III, IV, and VI • lacrimal nerve • frontal nerve • nasociliary nerve • orbital branch of middle meningeal artery • recurrent branch of lacrimal artery • superior orbital vein • superior ophthalmic vein Lund University / Faculty of Medicine / Inst. Clinical Sciences / Radiology / ECNR Dubrovnik / Oct 2018 Lund University / Faculty of Medicine / Inst. -
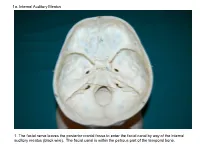
1A. Internal Auditory Meatus
1a. Internal Auditory Meatus 1. The facial nerve leaves the posterior cranial fossa to enter the facial canal by way of the internal auditory meatus (black wire). The facial canal is within the petrous part of the temporal bone. 1b. Internal Auditory Meatus The facial nerve leaves the posterior cranial fossa to enter the facial canal by way of the internal auditory meatus (black wire). 2. Hiatus of the Canal and Groove for the Greater Superficial Petrosal Nerve The greater superficial petrosal nerve leaves the facial canal to enter the middle cranial fossa by way of the hiatus of the canal for the greater superficial petrosal nerve (black wire). 3. Pterygoid Canal at Anterior Lip of the Lacerate Foramen The greater superficial petrosal nerve is joined by the deep petrosal nerve to form the nerve of the pterygoid canal (black and red wire). This nerve leaves the middle cranial fossa to enter the pterygopalatine fossa by way of the pterygoid canal. The posterior opening of the pterygoid canal is at the anterior lip of the lacerate foramen. The greater superficial nerve and the deep petrosal nerve travel within the cavernous sinus. 4. Pterygopalatine Fossa Seen Through the Pterygomaxillary Fissure The anterior opening of the pterygoid canal is into the pterygopalatine fossa (black wire). The pterygopalatine fossa is located medial to the pterygomaxillary fissure and contains the pterygopalatine ganglion. 5. External Auditory Meatus The chorda tympani nerve leaves the facial canal and crosses the middle ear (black wire). It then leaves the middle ear to arrive in the infratemporal fossa by way of the petrotympanic fissure. -

Morphometric Study of Hypoglossal Canal of Occipital Bone in Dry Skulls of Two States in Southern Nigeria Enaohwo, Taniyohwo.MAMERHI1, Okoro
Bangladesh Journal of Medical Science Vol. 19 No. 04 October’20 Original article: Morphometric study of hypoglossal canal of occipital bone in dry skulls of two states in southern nigeria Enaohwo, Taniyohwo.MAMERHI1, Okoro. Ogheneyebrorue. GODSWILL Abstract: Background: It is observed that the morphologic and morphometric variability of the occipital bone structures may coexist in the same individual or among different subjects of the same or different populations and thus, a sound knowledge of the morphometry of this area can provide important benefits in determining safe surgical zones during surgical procedures. Aim: The present study was aimed at measuring the length (right and left) and width (right and left) of the hypoglossal canal among adult dry skulls of two states in southern Nigeria. Materials and Method: This study adopted the cross sectional study design. A total of eighty (80) hypoglossal canal; right and left were selected by simple random sampling and their length and width were measured with the aid of the digital vernier caliper. Results: The hypoglossal canal length on the right side was seen to be higher compared to the left length of the hypoglossal canal while the right hypoglossal canal width was seen to be higher compared to the left hypoglossal canal width and also observed differences between the right and left sides were statistically significant (P=0.01). Conclusion: There was a statistical significant difference with regard to hypoglossal canal length (right and left) and width (right and left) among the studied population. Keywords: Occipital bone, hypoglossal canal, morphology, variation Bangladesh Journal of Medical Science Vol. -

Lab Manual Axial Skeleton Atla
1 PRE-LAB EXERCISES When studying the skeletal system, the bones are often sorted into two broad categories: the axial skeleton and the appendicular skeleton. This lab focuses on the axial skeleton, which consists of the bones that form the axis of the body. The axial skeleton includes bones in the skull, vertebrae, and thoracic cage, as well as the auditory ossicles and hyoid bone. In addition to learning about all the bones of the axial skeleton, it is also important to identify some significant bone markings. Bone markings can have many shapes, including holes, round or sharp projections, and shallow or deep valleys, among others. These markings on the bones serve many purposes, including forming attachments to other bones or muscles and allowing passage of a blood vessel or nerve. It is helpful to understand the meanings of some of the more common bone marking terms. Before we get started, look up the definitions of these common bone marking terms: Canal: Condyle: Facet: Fissure: Foramen: (see Module 10.18 Foramina of Skull) Fossa: Margin: Process: Throughout this exercise, you will notice bold terms. This is meant to focus your attention on these important words. Make sure you pay attention to any bold words and know how to explain their definitions and/or where they are located. Use the following modules to guide your exploration of the axial skeleton. As you explore these bones in Visible Body’s app, also locate the bones and bone markings on any available charts, models, or specimens. You may also find it helpful to palpate bones on yourself or make drawings of the bones with the bone markings labeled. -

Vertebral Column
Vertebral Column • Backbone consists of Cervical 26 vertebrae. • Five vertebral regions – Cervical vertebrae (7) Thoracic in the neck. – Thoracic vertebrae (12) in the thorax. – Lumbar vertebrae (5) in the lower back. Lumbar – Sacrum (5, fused). – Coccyx (4, fused). Sacrum Coccyx Scoliosis Lordosis Kyphosis Atlas (C1) Posterior tubercle Vertebral foramen Tubercle for transverse ligament Superior articular facet Transverse Transverse process foramen Facet for dens Anterior tubercle • Atlas- ring of bone, superior facets for occipital condyles. – Nodding movement signifies “yes”. Axis (C2) Spinous process Lamina Vertebral foramen Transverse foramen Transverse process Superior articular facet Odontoid process (dens) •Axis- dens or odontoid process is body of atlas. – Pivotal movement signifies “no”. Typical Cervical Vertebra (C3-C7) • Smaller bodies • Larger spinal canal • Transverse processes –Shorter – Transverse foramen for vertebral artery • Spinous processes of C2 to C6 often bifid • 1st and 2nd cervical vertebrae are unique – Atlas & axis Typical Cervical Vertebra Spinous process (bifid) Lamina Vertebral foramen Inferior articular process Superior articular process Transverse foramen Pedicle Transverse process Body Thoracic Vertebrae (T1-T12) • Larger and stronger bodies • Longer transverse & spinous processes • Demifacets on body for head of rib • Facets on transverse processes (T1-T10) for tubercle of rib Thoracic Vertebra- superior view Spinous process Transverse process Facet for tubercle of rib Lamina Superior articular process -

Cranial Nerve VIII
Cranial Nerve VIII Color Code Important (The Vestibulo-Cochlear Nerve) Doctors Notes Notes/Extra explanation Please view our Editing File before studying this lecture to check for any changes. Objectives At the end of the lecture, the students should be able to: ✓ List the nuclei related to vestibular and cochlear nerves in the brain stem. ✓ Describe the type and site of each nucleus. ✓ Describe the vestibular pathways and its main connections. ✓ Describe the auditory pathway and its main connections. Due to the difference of arrangement of the lecture between the girls and boys slides we will stick to the girls slides then summarize the pathway according to the boys slides. Ponto-medullary Sulcus (cerebello- pontine angle) Recall: both cranial nerves 8 and 7 emerge from the ventral surface of the brainstem at the ponto- medullary sulcus (cerebello-pontine angle) Brain – Ventral Surface Vestibulo-Cochlear (VIII) 8th Cranial Nerve o Type: Special sensory (SSA) o Conveys impulses from inner ear to nervous system. o Components: • Vestibular part: conveys impulses associated with body posture ,balance and coordination of head & eye movements. • Cochlear part: conveys impulses associated with hearing. o Vestibular & cochlear parts leave the ventral surface* of brain stem through the pontomedullary sulcus ‘at cerebellopontine angle*’ (lateral to facial nerve), run laterally in posterior cranial fossa and enter the internal acoustic meatus along with 7th (facial) nerve. *see the previous slide Auditory Pathway Only on the girls’ slides 04:14 Characteristics: o It is a multisynaptic pathway o There are several locations between medulla and the thalamus where axons may synapse and not all the fibers behave in the same manner.