For Answer April 27Th
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Sinn-Fein-NA-EES.Pdf
Candidate Name Constituency Amount Assigned Total Expenditure on the candidate by the national agent € € 1. Micheal MacDonncha Dublin Bay North 5000 2.Denise Mitchell Dublin Bay North 5000 3.Chris Andrews Dublin Bay South 5000 450.33 4.Mary Lou McDonald Dublin Central 4000 5.Louise O’Reilly Dublin Fingal 8000 2449.33 6. Eoin O’Broin Dublin Mid West 3000 7. Dessie Ellis Dublin North West 3000 8.Cathleen Carney Boud Dublin North West 5000 9.Sorcha Nic Cormaic Dublin Rathdown 5000 10.Aengus Ó Snodaigh Dublin South 3000 Central 11.Màire Devine Dublin South 3000 Central 12. Sean Crowe Dublin South West 3000 13.Sarah Holland Dublin South West 5000 14.Paul Donnelly Dublin West 3000 69.50 15.Shane O’Brien Dun Laoghaire 5000 73.30 16.Caoimhghìn Ó Caoláin Cavan Monaghan 3000 129.45 17.Kathryn Reilly Cavan Monaghan 3000 192.20 18.Pearse Doherty Donegal 3000 19.Pádraig MacLochlainn Donegal 3000 20.Garry Doherty Donegal 3000 21.Annemarie Roche Galway East 5000 22.Trevor O’Clochartaigh Galway West 5000 73.30 23.Réada Cronin Kildare North 5000 24.Patricia Ryan Kildare South 5000 13.75 25.Brian Stanley Laois 3000 255.55 26.Paul Hogan Longford 5000 Westmeath 27.Gerry Adams Louth 3000 28.Imelda Munster Louth 10000 29.Rose Conway Walsh Mayo 10000 560.57 30.Darren O’Rourke Meath East 6000 31.Peadar Tòibìn Meath West 3000 247.57 32.Carol Nolan Offaly 4000 33.Claire Kerrane Roscommon Galway 5000 34.Martin Kenny Sligo Leitrim 3000 193.36 35.Chris MacManus Sligo Leitrim 5000 36.Kathleen Funchion Carlow Kilkenny 5000 37.Noeleen Moran Clare 5000 794.51 38.Pat Buckley Cork East 6000 202.75 39.Jonathan O’Brien Cork North Central 3000 109.95 40.Thomas Gould Cork North Central 5000 109.95 41.Nigel Dennehy Cork North West 5000 42.Donnchadh Cork South Central 3000 O’Laoghaire 43.Rachel McCarthy Cork south West 5000 101.64 44.Martin Ferris Kerry County 3000 188.62 45.Maurice Quinlivan Limerick City 3000 46.Seamus Browne Limerick City 5000 187.11 47.Seamus Morris Tipperary 6000 1428.49 48.David Cullinane Waterford 3000 565.94 49.Johnny Mythen Wexford 10000 50.John Brady Wicklow 5000 . -
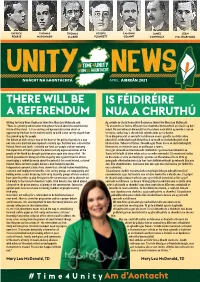
April Unity News
PATRICK THOMAS THOMAS JOSEPH ÉAMONN JAMES SEÁN PEARSE McDONAGH CLARKE PLUNKETT CEANNT CONNOLLY Mac DIARMADA #Time4Unity UNITY# AM LE hAONTACHT NEWS NUACHT NA hAONTACHTA APRIL AIBREÁN 2021 THERE WILL BE IS FÉIDIRÉIRE AWriting forREFERENDUM Unity News Úachtaran Shinn Féin Mary Lou McDonald said: AgNUA scríobh do Unity News A dúirt ÚachtaranCHRUTHÚ Shinn Féin Mary Lou McDonald: “There is a growing conversation throughout Ireland about the constitutional “Tá an comhrá ar fud na hÉireann faoi thodhchaí bunreachtúil an oileáin ag dul i future of the island. It is an exciting and dynamic discussion about an méad. Plé corraitheach dinimiciúil atá faoi dheis nach bhfuil ag mórán i saol an opportunity few have in the modern world; to build a new society shaped from lae inniu; sochaí nua a chruthú ón talamh aníos ag na daoine. the ground up by the people. Tá an díospóireacht ar aontacht na hÉireann anois i gcroílár an chláir oibre The debate on Irish unity is now at the heart of the political agenda in a way pholaitiúil ar bhealach nach bhfacthas ó cuireadh an chríochdheighilt céad not seen since partition was imposed a century ago. Partition was a disaster for bliain ó shin. Tubaiste d’Éirinn, Thuaidh agus Theas ba ea an chríochdheighilt. Ireland, North and South. It divided our land, our people and our economy. Rinnean tír, an mhuintir agus an geilleagar a roinnt. The imposition of Brexit against the democratically expressed wishes of the Toisc gur cuireadh an Breatimeacht i bhfeidhm i gcoinne thoil mhuintir an people of the North has brought partition once again into sharp relief. -

74 Dáil Éireann
(Second Supplementary Order Paper) 74 DÁIL ÉIREANN Dé Máirt, 1 Nollaig, 2020 Tuesday, 1st December, 2020 2 p.m. GNÓ COMHALTAÍ PRÍOBHÁIDEACHA PRIVATE MEMBERS' BUSINESS Fógra i dtaobh Leasú ar Thairiscint: Notice of Amendment to Motion [Please note: there is a change to the text of the Sinn Féin motion highlighted in bold on today’s Second Supplementary Order Paper.] 109. “That Dáil Éireann: notes that: — in five weeks’ time the pension age is due to increase to 67 years of age on 1st January, 2021; — legislation needed to stop the pension age increasing to 67 in January has not passed through the House; — every worker in the State makes a considerable tax contribution throughout their working life and should have the right to retire at 65; — some workers want to retire at 65, while others want to remain at work, where they are able and willing to do so; — numerous employment contracts stipulate an end of employment date in line with when an employee turns 65; — since the abolition of the State Pension Transition payment, thousands of 65-year olds have had to sign on for a Jobseeker’s payment; — there are now over 4,000 65-year olds in receipt of either Jobseeker’s Allowance or Jobseeker’s Benefit; — there is a difference of €45.30 between the Jobseeker payments and the State Pension leading to an annual loss of €2,355.60; and — the pension age is scheduled in legislation to increase to 67 years in 2021, and 68 years in 2028; and calls on the Government to: — restore the State Pension Transition payment for those retiring at 65 years of age; — abolish mandatory retirement (with exceptions for security-related employment) to give workers the choice to work or retire so long as they are fit to do so; P.T.O. -

Dáil Éireann
DÁIL ÉIREANN AN BILLE SLÁINTE (LEASÚ), 2020 HEALTH (AMENDMENT) BILL 2020 LEASUITHE COISTE COMMITTEE AMENDMENTS [No. 42 of 2020] [22 October, 2020] DÁIL ÉIREANN AN BILLE SLÁINTE (LEASÚ), 2020 —AN COISTE HEALTH (AMENDMENT) BILL 2020 —COMMITTEE STAGE Leasuithe Amendments SECTION 3 1. In page 4, line 36, after “Equality” to insert “and Dáil Éireann”. —Bríd Smith, Richard Boyd Barrett, Gino Kenny. 2. In page 4, between lines 36 and 37, to insert the following: “(e) The Minister shall, before prescribing a fixed penalty provision in regulations under this section, recognising the emergency nature of these regulations, consult with and seek approval of a majority of the members of both Houses of the Oireachtas.”. —David Cullinane, Chris Andrews, John Brady, Martin Browne, Pat Buckley, Matt Carthy, Sorca Clarke, Rose Conway-Walsh, Réada Cronin, Seán Crowe, Pa Daly, Pearse Doherty, Paul Donnelly, Dessie Ellis, Mairéad Farrell, Kathleen Funchion, Thomas Gould, Johnny Guirke, Martin Kenny, Claire Kerrane, Pádraig Mac Lochlainn, Mary Lou McDonald, Denise Mitchell, Imelda Munster, Johnny Mythen, Eoin Ó Broin, Donnchadh Ó Laoghaire, Ruairí Ó Murchú, Louise O'Reilly, Darren O'Rourke, Aengus Ó Snodaigh, Maurice Quinlivan, Patricia Ryan, Brian Stanley, Pauline Tully, Mark Ward, Violet-Anne Wynne. 3. In page 5, line 21, after “Equality” to insert “and Dáil Éireann”. —Bríd Smith, Richard Boyd Barrett, Gino Kenny. [No. 42 of 2020] [22 October, 2020] [SECTION 3] 4. In page 5, between lines 21 and 22, to insert the following: “(d) The Minister shall, before prescribing a fixed penalty provision in regulations under this section, recognising the emergency nature of these regulations, consult with and seek approval of a majority of the members of both Houses of the Oireachtas.”. -

Sinn Fein
Received by NSD/FARA Registration Unit 12/06/2019 1:00 PM From: Friends of Sinn Fein <[email protected]> Sent: Friday, December 6, 2019 1:00 PM To: Subject: Friday Newsletter Friends of Sinn US Congressional Resolution to protect the Good Friday Agreement Received by NSD/FARA Registration Unit 12/06/2019 1:00 PM Received by NSD/FARA Registration Unit 12/06/2019 1:00 PM The United States House of Representatives has passed Resolution 585 calling for the full implementation of the Good Friday and subsequent Agreements. The resolution insists that any future trade deal between the US and Britain must protect the Good Friday Agreement. Speaking following the passing of the resolution Sinn Fein President Mary Lou McDonald TD said: “Over the past twenty-five years, United States Presidents and political leaders have been central to the Irish Peace process and the Good Friday Agreement. "That special relationship endures and crosses party political lines. "A future trade deal between the US and Britain post Brexit is the responsibility of the US Congress. "Today the congress passed a resolution to oppose a hard border on the island of Ireland and supported the right to national self-determination in line with provisions of the Good Friday Agreement. "The Congress also insisted that any new trade deal with Britain must be contingent on meeting the obligations of the Good Friday Agreement including the continued incorporation into law of the European Convention on Human Rights. “I would like to thank Rep. Tom Suozzi for introducing this resolution and Rep. Peter King for his bipartisan sponsorship. -

WORSHAM-DOCUMENT-2019.Pdf
Democracy and the Fallacy of the Post-Conflict Era in Northern Ireland The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Worsham, Nicole A. 2019. Democracy and the Fallacy of the Post- Conflict Era in Northern Ireland. Master's thesis, Harvard Extension School. Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:42004239 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Democracy and the Fallacy of the Post -Conflict Era in Northern Ireland Nicole A. Worsham A Thesis in the Field of International Relations for the Degree of Master of Liberal Arts in Extension Studies Harvard University May 2019 © 2019 Nicole A. Worsham Abstract While Northern Ireland has experienced a period of relative peace since the signing of the Good Friday Agreement in 1998, entrenched, age-old tensions persist between those of opposing political persuasions, and between those of different religions. Those tensions continue to manifest themselves in ways which disprove the notion that Northern Ireland is in a post-conflict era. Further, demographic shifts, social changes, and external pressures make the status quo in Northern Ireland untenable. Profound uncertainty over Brexit now threatens the structure and foundation of government, and, perhaps of more immediate concern, the devolved local Executive and Assembly of Northern Ireland have collapsed, with little evidence that local government may be restored in the near term. -

1. Debbie Abrahams, Labour Party, United Kingdom 2
1. Debbie Abrahams, Labour Party, United Kingdom 2. Malik Ben Achour, PS, Belgium 3. Tina Acketoft, Liberal Party, Sweden 4. Senator Fatima Ahallouch, PS, Belgium 5. Lord Nazir Ahmed, Non-affiliated, United Kingdom 6. Senator Alberto Airola, M5S, Italy 7. Hussein al-Taee, Social Democratic Party, Finland 8. Éric Alauzet, La République en Marche, France 9. Patricia Blanquer Alcaraz, Socialist Party, Spain 10. Lord John Alderdice, Liberal Democrats, United Kingdom 11. Felipe Jesús Sicilia Alférez, Socialist Party, Spain 12. Senator Alessandro Alfieri, PD, Italy 13. François Alfonsi, Greens/EFA, European Parliament (France) 14. Amira Mohamed Ali, Chairperson of the Parliamentary Group, Die Linke, Germany 15. Rushanara Ali, Labour Party, United Kingdom 16. Tahir Ali, Labour Party, United Kingdom 17. Mahir Alkaya, Spokesperson for Foreign Trade and Development Cooperation, Socialist Party, the Netherlands 18. Senator Josefina Bueno Alonso, Socialist Party, Spain 19. Lord David Alton of Liverpool, Crossbench, United Kingdom 20. Patxi López Álvarez, Socialist Party, Spain 21. Nacho Sánchez Amor, S&D, European Parliament (Spain) 22. Luise Amtsberg, Green Party, Germany 23. Senator Bert Anciaux, sp.a, Belgium 24. Rt Hon Michael Ancram, the Marquess of Lothian, Former Chairman of the Conservative Party, Conservative Party, United Kingdom 25. Karin Andersen, Socialist Left Party, Norway 26. Kirsten Normann Andersen, Socialist People’s Party (SF), Denmark 27. Theresa Berg Andersen, Socialist People’s Party (SF), Denmark 28. Rasmus Andresen, Greens/EFA, European Parliament (Germany) 29. Lord David Anderson of Ipswich QC, Crossbench, United Kingdom 30. Barry Andrews, Renew Europe, European Parliament (Ireland) 31. Chris Andrews, Sinn Féin, Ireland 32. Eric Andrieu, S&D, European Parliament (France) 33. -

Dáil Éireann
DÁIL ÉIREANN AN COMHCHOISTE UM NA MEÁIN, TURASÓIREACHT, EALAÍONA, CULTÚR, SPÓRT AGUS GAELTACHT JOINT COMMITTEE ON MEDIA, TOURISM, ARTS, CULTURE, SPORT AND THE GAELTACHT Dé Céadaoin, 18 Samhain 2020 Wednesday, 18 November 2020 Tháinig an Comhchoiste le chéile ag 2 p.m. The Joint Committee met at 2 p.m. Comhaltaí a bhí i láthair/Members present: Teachtaí Dála/Deputies Seanadóirí/Senators Chris Andrews,* Malcolm Byrne, Ciarán Cannon, Shane Cassells, Alan Dillon, Annie Hoey. Peter Fitzpatrick, Brendan Griffin, Marc MacSharry,+ Mattie McGrath, Imelda Munster, Christopher O’Sullivan. * In éagmais/In the absence of Deputy Johnny Mythen + In éagmais le haghaidh cuid den choiste / In the absence for part of the meeting of Deputy Christopher O’Sullivan I láthair/In attendance: Senator Seán Kyne. Teachta/Deputy Niamh Smyth sa Chathaoir/in the Chair. 1 JMTACSG The joint committee met in private session until 2.04 p.m. Key Priorities for Sport Ireland and Impact of Covid-19 on Sports Sector: Sport Ireland Chairman: All members have the speaking slot rota. Deputy Brendan Griffin will be first, followed by Deputy Imelda Munster, Senator Malcolm Byrne and Senator Annie Hoey. We will then move down the list. Deputy Chris Andrews need not worry. He has been included as speaker number 11. Does he have the rota with the list of speakers? Deputy Chris Andrews: Yes, I have it here. Does the committee have to conclude by 4 p.m.? Chairman: Yes. Deputy Griffin is getting five minutes. Deputy Brendan Griffin: Yes. Chairman: Deputy Mattie McGrath is very welcome. I am glad he could join us as I know he was busy in the convention centre this morning. -

Annual Activity Report 2020 European Parliament Liaison Office in Ireland Europe House 12-14 Lower Mount Street Dublin D02 W710 Tel
The European Parliament Liaison Office in Ireland Annual activity report 2020 European Parliament Liaison Office in Ireland Europe House 12-14 Lower Mount Street Dublin D02 W710 Tel. +353 (0)1 6057900 Website: www.europarl.ie Facebook: @EPinIreland Twitter: @EPinIreland and @EPIreland_Edu Instagram: @ep_ireland © European Union/EP, 2021 Reproduction is authorised provided the source is acknowledged. Contents Contents 3 Top Posts and Tweets in 2020 34 Top Content Highlighting MEPs’ Work 36 Introduction 5 Top Content on Cooperation with other Members of the Organisations and MEPs 39 European Parliament for Ireland 6 Top Content Produced by EPLO Dublin 40 Remote Plenary Sessions 7 Strategy 41 Social Media Data Overview 41 Outreach Activities 10 Cross-border activities 13 Activities for young people 42 Regular newsletter 17 European Parliament Ambassador School Campaigns 18 Programme (EPAS) 42 International Women’s Day 18 Euroscola 44 Charlemagne Youth Prize 19 Information visits to Europe House Europeans Against COVID-19 19 in Dublin 45 European Citizen’s Prize 21 Blue Star Programme 45 Lux Audience Award 21 Other youth activities 46 Sakharov Prize 21 Back to school 47 Bridge the Pond initiative 48 Other information activities 22 Annexes 43 EP grant programme Annex I - Ambassador Schools for information activities 24 Academic Year 2019-2020 49 Media 25 Annex II - Ambassador Schools Journalism students and the EP 25 Academic Year 2020-2021 50 Europeans Against COVID-19 26 Annex III - Schools representing Ireland at Commission hearings and -

Dáil Éireann
DÁIL ÉIREANN AN BILLE UM BARRACHAS NÁISIÚNTA (CÚLCHISTE LE hAGHAIDH TEAGMHAIS EISCEACHTÚLA), 2018 NATIONAL SURPLUS (RESERVE FUND FOR EXCEPTIONAL CONTINGENCIES) BILL 2018 LEASUITHE TUARASCÁLA REPORT AMENDMENTS [No. 116a of 2018] [15 April, 2019] DÁIL ÉIREANN AN BILLE UM BARRACHAS NÁISIÚNTA (CÚLCHISTE LE hAGHAIDH TEAGMHAIS EISCEACHTÚLA), 2018 —AN TUARASCÁIL NATIONAL SURPLUS (RESERVE FUND FOR EXCEPTIONAL CONTINGENCIES) BILL 2018 —REPORT Leasuithe Amendments 1. In page 4, to delete lines 27 to 31. —Jonathan O'Brien, Pearse Doherty, Gerry Adams, Mary Lou McDonald, Caoimhghín Ó Caoláin, Martin J. Ferris, Aengus Ó Snodaigh, Dessie Ellis, Seán Crowe, Brian Stanley, Imelda Munster, Louise O'Reilly, Denise Mitchell, Eoin Ó Broin, John Brady, David Cullinane, Kathleen Funchion, Pat Buckley, Donnchadh Ó Laoghaire, Maurice Quinlivan, Martin Kenny. 2. In page 4, lines 34 and 35, to delete “, in addition to any assets referred to in subsection (1) and, as the case may be, sums referred to in subsection (2),”. —Jonathan O'Brien, Pearse Doherty, Gerry Adams, Mary Lou McDonald, Caoimhghín Ó Caoláin, Martin J. Ferris, Aengus Ó Snodaigh, Dessie Ellis, Seán Crowe, Brian Stanley, Imelda Munster, Louise O'Reilly, Denise Mitchell, Eoin Ó Broin, John Brady, David Cullinane, Kathleen Funchion, Pat Buckley, Donnchadh Ó Laoghaire, Maurice Quinlivan, Martin Kenny. 3. In page 4, to delete lines 37 to 40, and in page 5, to delete lines 1 to 9. —Jonathan O'Brien, Pearse Doherty, Gerry Adams, Mary Lou McDonald, Caoimhghín Ó Caoláin, Martin J. Ferris, Aengus Ó Snodaigh, Dessie Ellis, Seán Crowe, Brian Stanley, Imelda Munster, Louise O'Reilly, Denise Mitchell, Eoin Ó Broin, John Brady, David Cullinane, Kathleen Funchion, Pat Buckley, Donnchadh Ó Laoghaire, Maurice Quinlivan, Martin Kenny. -

Notice-Of-Poll-Midla
IARRTHÓRA/CANDIDATE Moltóra/Proposer (if any) BRENNAN - SOLIDARITY PEOPLE BEFORE PROFIT (CYRIL BRENNAN of Rose Cottage, Lissacholly, Self Ballyshannon, Co. Donegal. Multi Task Attendant.) Liosta Ionaid SPBP Replacement List. CARTHY - SINN FÉIN Pearse Doherty (MATT CARTHY of 52 Foxfield, Carraig Mhachaire Rois, Magheraclogher, Derrybeg, Co. Mhuineacháin. Member of the European Parliament.) Letterkenny, Co. Donegal. Liosta Ionaid SF Replacement List. CASEY - NON PARTY (PETER CASEY of Edgewater House, Carrowhugh, Self Greencastle, Co. Donegal, F93 A2P3. Businessman) Liosta Ionaid PC Replacement List. FLANAGAN - NON-PARTY (LUKE 'MING' FLANAGAN of 5 Knockroe Park, Castlerea, Co. Roscommon. Full Time Public Self Representative.) Liosta Ionaid LMF Replacement List. GREENE - DIRECT DEMOCRACY IRELAND (D.D.I.) (PATRICK GREENE of Harestown Road, Brownstown, Self Monasterboice, Co. Louth. Timber Worker.) Liosta Ionaid DDI Replacement List. HANNIGAN - THE LABOUR PARTY (Group of the Progressive Alliance of Socialists and Democrats) (DOMINIC HANNIGAN of 14B Glenview Self Drive, Galway, H91 Y5NA. Civil Engineer.) Liosta Ionaid LAB Replacement List. HEALY EAMES - NON-PARTY (FIDELMA HEALY EAMES of Maree, Oranmore, Self Co. Galway. Primary School Teacher.) Liosta Ionaid FHE Replacement List. MAHAPATRA - NON PARTY (DILIP MAHAPATRA of Elora, Stokeshill, Dromiskin, Self Dundalk, Co. Louth, A91 VW99. Medical Doctor.) McGUINNESS - FINE GAEL (Group of the European People's Party (Christian Democrats)) (MAIREAD McGUINNESS of Mentrim, Self Drumconrath, Navan, Co. Meath, C15 YE3H. Member of the European Parliament.) Liosta Ionaid FG Replacement List. McHUGH - GREEN PARTY/COMHAONTAS GLAS (SAOIRSE McHUGH of Dooagh, Achill, Co. Mayo. Self Sustainable Farming Advocate.) Liosta Ionaid GP Replacement List. MILLER - NON-PARTY (JAMES MILLER of Toorlisnamore, Kilbeggan, Self Co. Westmeath. -

Critical Engagement: Irish Republicanism, Memory Politics
Critical Engagement Critical Engagement Irish republicanism, memory politics and policing Kevin Hearty LIVERPOOL UNIVERSITY PRESS First published 2017 by Liverpool University Press 4 Cambridge Street Liverpool L69 7ZU Copyright © 2017 Kevin Hearty The right of Kevin Hearty to be identified as the author of this book has been asserted by him in accordance with the Copyright, Designs and Patents Act 1988. All rights reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the publisher. British Library Cataloguing-in-Publication data A British Library CIP record is available print ISBN 978-1-78694-047-6 epdf ISBN 978-1-78694-828-1 Typeset by Carnegie Book Production, Lancaster Contents Acknowledgements vii List of Figures and Tables x List of Abbreviations xi Introduction 1 1 Understanding a Fraught Historical Relationship 25 2 Irish Republican Memory as Counter-Memory 55 3 Ideology and Policing 87 4 The Patriot Dead 121 5 Transition, ‘Never Again’ and ‘Moving On’ 149 6 The PSNI and ‘Community Policing’ 183 7 The PSNI and ‘Political Policing’ 217 Conclusion 249 References 263 Index 303 Acknowledgements Acknowledgements This book has evolved from my PhD thesis that was undertaken at the Transitional Justice Institute, University of Ulster (TJI). When I moved to the University of Warwick in early 2015 as a post-doc, my plans to develop the book came with me too. It represents the culmination of approximately five years of research, reading and (re)writing, during which I often found the mere thought of re-reading some of my work again nauseating; yet, with the encour- agement of many others, I persevered.