A Toolkit for Pharmacy, Podiatry, Optometry, and Dentistry
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
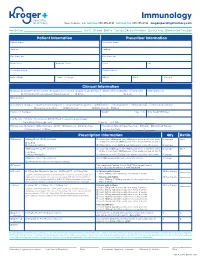
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -

PEILING CHEN EDUCATION Doctorate of Optometry May 2018
PEILING CHEN EDUCATION Doctorate of Optometry May 2018 Salus University, Pennsylvania College of Optometry, Elkins Park, PA Bachelors of Science in Biology May 2013 College of Chemical and Life Sciences, University of Maryland, College Park, MD EMPLOYMENT Assistant Faculty of Ophthalmology January 2019- present Wilmer Eye Institute, Johns Hopkins Medicine ◾ Provide comprehensive eye services specializing in the diagnosis and management of ocular diseases, conditions and post-operative surgical care in areas such as: dry eye, ocular allergy, macular degeneration, retinal pathologies, diabetic retinopathy, hypertensive retinopathy, glaucoma, LASIK care, and cataracts; as well as, eye examinations and contact lens fittings Optometrist August 2018- December 2018 National Vision, Inc. ◾ Provide comprehensive eye exams, contact lense fittings and assistance in the referral and management of glaucoma, diabetes and cataract patients ◾ Treat minor ocular service conditions like blepharitis, ocular allergy and dry eye Optical Principles and Ophthalmic Application Teaching Assistant August 2015-May 2016 Pennsylvania College of Optometry, Elkins Park, PA ◾ Assisted first year optometry students at the Pennsylvania College of Optometry with challenging course topics ◾ Mentored underclassmen on how to succeed in the course based on prior experience Vision Therapist September 2011-2014 Appelbaum Eye Care Associates, Bethesda, MD ◾ Provided assistance on vision therapy exercises to patients with binocular vision and ocular motor dysfunctions ◾ Performed -

STEM Disciplines
STEM Disciplines In order to be applicable to the many types of institutions that participate in the HERI Faculty Survey, this list is intentionally broad and comprehensive in its definition of STEM disciplines. It includes disciplines in the life sciences, physical sciences, engineering, mathematics, computer science, and the health sciences. Agriculture/Natural Resources Health Professions 0101 Agriculture and related sciences 1501 Alternative/complementary medicine/sys 0102 Natural resources and conservation 1503 Clinical/medical lab science/allied 0103 Agriculture/natural resources/related, other 1504 Dental support services/allied 1505 Dentistry Biological and Biomedical Sciences 1506 Health & medical administrative services 0501 Biochem/biophysics/molecular biology 1507 Allied health and medical assisting services 0502 Botany/plant biology 1508 Allied health diagnostic, intervention, 0503 Genetics treatment professions 0504 Microbiological sciences & immunology 1509 Medicine, including psychiatry 0505 Physiology, pathology & related sciences 1511 Nursing 0506 Zoology/animal biology 1512 Optometry 0507 Biological & biomedical sciences, other 1513 Osteopathic medicine/osteopathy 1514 Pharmacy/pharmaceutical sciences/admin Computer/Info Sciences/Support Tech 1515 Podiatric medicine/podiatry 0801 Computer/info tech administration/mgmt 1516 Public health 0802 Computer programming 1518 Veterinary medicine 0803 Computer science 1519 Health/related clinical services, other 0804 Computer software and media applications 0805 Computer systems -

Medical-Dental History Personal History All of the Information Which You Provided on This Form Will Be Held in the Strictest Confidence
Medical-Dental History Personal History All of the information which you provided on this form will be held in the strictest confidence. Although some questions may seem unimportant at the time, they may be vital in an emergency situation. Please answer each question and ask if you need assistance completing the form. Patients Name:________________________________________________ Sex: M F Parents / Guardian:___________________________________________________________________ Date of Birth: __________________________ BC Care Card: ____________________________ Mailing Address:_____________________________________________________________________ Home Phone: ______________________________ Cell Phone:________________________________ E-Mail:_____________________________________________________________________________ Purpose of Visit:______________________________________________________________________ Family Dentist:____________________________ Medical Doctor: ___________________________ Referred by:_________________________________________________________________________ I authorize the doctor to perform diagnostic procedures and treatment as may be necessary for proper dental care. I authorize the release of information concerning my child’s health care, advice, and treatment provided for the purpose of evaluating and administering claims for insurance benefits. I understand that my dental insurance carrier or payer of my dental benefits may pay less than the actual fee for services. I understand that I am financially responsible for payment -

Dental Medicine (DDS/DMD)
Pre-Health Information for Dental Medicine (DDS/DMD) Dentists who have a DMD or DDS have the similar education. Both degrees use the same curriculum requirements set by the American Dental Association and the type of degree awarded is determined by the university. Profession web site(s): www.ada.org , www.adea.org Application web site: www.adea.org/aadsas or for Texas schools: www.tmdsas.com Admission/Entrance exam:– DAT (Dental Admission Test) Transcripts: Official transcripts from ALL institutions attended, including Marquette University, must be sent directly from the institution to the central application service. If you completed study abroad courses at a U.S. sponsored program abroad, you must send transcripts. If you studied abroad and the courses and grades do not appear on a U.S. transcript, then you need to have transcripts sent to AADSAS from the foreign school or an evaluation service. Course prerequisites: Course prerequisites vary by program. Typical prerequisites include Biology 1001, 1002, a separate lab course such as Biology 2001, a biochemistry course, Chemistry 1001, 1002, 2111, 2112, Physics 1001 and 1002. Different course numbers for majors (e.g., Chemistry 1014 for Majors) will be accepted. Physics is required for dental school but not for the DAT. Many dental schools require courses such as Biochemistry, Anatomy, Physiology and/or Microbiology, Psychology, Sociology and other upper level biology or science courses. Students should research schools to which they will apply early enough to ensure they can complete all necessary pre-requisite courses. Observation hours/experience: Dental schools like to see well-rounded applications and look for quality and depth of experiences rather than requiring a specific number of hours. -

ADA.Org: Dental History Timeline
ARCHIVES OF THE AMERICAN DENTAL ASSOCIATION HISTORY OF DENTISTRY TIMELINE Compiled from various sources by ADA Library/Archives staff Ancient Origins • 5000 BC -A Sumerian text of this date describes “tooth worms” as the cause of dental decay. • 2600 BC -Death of Hesy-Re, an Egyptian scribe, often called the first “dentist.” An inscription on his tomb includes the title “the greatest of those who deal with teeth, and of physicians.” This is the earliest known reference to a person identified as a dental practitioner. • 1700-1550 BC -An Egyptian text, the Ebers Papyrus, refers to diseases of the teeth and various toothache remedies. • 500-300 BC -Hippocrates and Aristotle write about dentistry, including the eruption pattern of teeth, treating decayed teeth and gum disease, extracting teeth with forceps, and using wires to stabilize loose teeth and fractured jaws. • 100 BC -Celsus, a Roman medical writer, writes extensively in his important compendium of medicine on oral hygiene, stabilization of loose teeth, and treatments for toothache, teething pain, and jaw fractures. • 166-201 AD-The Etruscans practice dental prosthetics using gold crowns and fixed bridgework. The Beginnings of A Profession—Middle Ages • 500-1000 -During the Early Middle Ages in Europe medicine and surgery, including dentistry, is generally practiced by monks, the most educated people of the period. • 700 -A medical text in China mentions the use of “silver paste,” a type of amalgam. • 1130-1163 -A series of Papal edicts prohibit monks from performing any type of surgery, bloodletting or tooth extraction. Barbers often assisted monks in their surgical ministry because they visited monasteries to shave the heads of monks and the tools of the barber trade—sharp knives and razors—were useful for surgery. -

Pharmacy/Medical Drug Prior Authorization Form
High Cost Medical Drugs List High Cost Medical Drugs administered by Health Alliance™ providers within physician offices, infusion centers or hospital outpatient settings must be acquired from preferred specialty vendors. Health Alliance will not reimburse any drug listed as a “High Cost Medical Drug,” whether obtained from the provider’s own stock or via “buy-and-bill.” This drug list does not apply to members with Medicare coverage. Information on how to acquire these medications is located at the end of this document. Recent Updates Preferred Contact Drug Therapy Drug Name Code PA Effective Change Vendor Number Oncology – Injectable DARZALEX FASPRO J9144 YES 10/1/2021 CVS/Caremark® 800-237-2767 Added High Cost Medical Drug List Preferred Contact Drug Therapy Drug Name Code PA Effective Vendor Number Acromegaly SANDOSTATIN J2353 YES 7/1/2020 CVS/Caremark® 800-237-2767 Acromegaly SOMATULINE J1930 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products JETREA J7316 YES 7/1/2020 LDD Additional Products PROLASTIN J0256 YES 7/1/2020 LDD Additional Products QUTENZA J7336 NO 7/1/2020 LDD Additional Products REVCOVI J3590 YES 7/1/2020 LDD Additional Products RADICAVA J1301 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products SIGNIFOR J2502 YES 7/1/2020 Accredo® 866-759-1557 Additional Products SPRAVATO J3490 YES 7/1/2020 CVS/Caremark® 800-237-2767 Additional Products STRENSIQ J3590 YES 7/1/2020 LDD Additional Products THIOTEPA J9340 YES 7/1/2020 CVS/Caremark® 800-237-2767 Allergic Asthma CINQAIR J2786 YES 7/1/2020 CVS/Caremark® 800-237-2767 -
GUIDE to SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications
Journal of Oral and Maxillofacial Surgery Journal of Oral and Maxillofacial August 2015 • Volume 73 • Supplement 1 www.joms.org August 2015 • Volume 73 • Supplement 1 • pp 1-62 73 • Supplement 1 Volume August 2015 • GUIDE TO SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications INSERT ADVERT Elsevier YJOMS_v73_i8_sS_COVER.indd 1 23-07-2015 04:49:39 Journal of Oral and Maxillofacial Surgery Subscriptions: Yearly subscription rates: United States and possessions: individual, $330.00 student and resident, $221.00; single issue, $56.00. Outside USA: individual, $518.00; student and resident, $301.00; single issue, $56.00. To receive student/resident rate, orders must be accompanied by name of affiliated institution, date of term, and the signature of program/residency coordinator on institution letter- head. Orders will be billed at individual rate until proof of status is received. Prices are subject to change without notice. Current prices are in effect for back volumes and back issues. Single issues, both current and back, exist in limited quantities and are offered for sale subject to availability. Back issues sold in conjunction with a subscription are on a prorated basis. Correspondence regarding subscriptions or changes of address should be directed to JOURNAL OF ORAL AND MAXILLOFACIAL SURGERY, Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043. Telephone: 1-800-654-2452 (US and Canada); 314-447-8871 (outside US and Canada). Fax: 314-447-8029. E-mail: journalscustomerservice-usa@ elsevier.com (for print support); [email protected] (for online support). Changes of address should be sent preferably 60 days before the new address will become effective. -

Modernizing the Scope of Practice of Optometry Will Improve Access to Needed Eye and Vision Health Care for All Maryland Citizens
P.O. Box 350, Stevenson, MD 21153 ! T: (410) 486-9662 ! F: (443) 378-8845 ! www.marylandoptometry.org Modernizing the scope of practice of optometry will improve access to needed eye and vision health care for all Maryland citizens. It will ensure patients receive the best quality of care available, improve overall patient health outcomes and lower health care costs for both patients and insurers alike. SUMMARY OF SCOPE EXPANSION OBJECTIVES By removing outdated prohibitions in current statute, the bill seeks to better serve optometric patients by allowing Maryland optometrists to: • Prescribe all FDA Approved Therapeutic and Diagnostic Agents (e.g., oral and topical drugs, vitamins, and other therapies) • Independently Treat Glaucoma (development of patient treatment plan & delivery of pre/post operative care) • Perform In-office Diagnostic Testing (e.g., genetic testing via cheek swab and blood glucose testing for diabetes) • Order Diagnostic Tests (e.g., blood work, MRI, x-ray, sonogram, other lab work related to diseases of the eye and ocular system) • Remove Foreign Bodies “STATE OF THE STATE” SCOPE OF PRACTICE FACTS • Doctors of optometry order diagnostic tests in 45 states • Doctors of optometry prescribe controlled substances in 44 • Doctors of optometry to use oral drugs to treat Glaucoma in 42 states • Doctors of optometry prescribe anti-fungal oral medications in 41 states EDUCATION & TRAINING Optometrists receive a minimum of eight 8 years of education and training to obtain the required undergraduate and doctorate degrees necessary to practice optometry. All optometrists are required to pass a three part comprehensive national exam administered by the National Board of Examiners in Optometry prior to receiving their doctorate degree. -
Primary Care in Podiatric Medicine Certification and Foot and Ankle
MISSION STATEMENT We exist to protect and improve the podiatric health and welfare of the public. AMERICAN BOARD OF MULTIPLE SPECIALTIES IN PODIATRY The American Board of Multiple Specialties in Podiatry (the Board) was incorporated in 1986 to promote certification among podiatrists. In 2008, its certification programs were accredited by the American National Standards Institute (ANSI) for meeting the international standards for accreditation programs as set forth in ANSI/ISO/IEC/17024:2003. In 2012, the ABMSP was also accredited by URAC (Utilization Review Accreditation Commission). PURPOSE STATEMENT The specific and primary purpose of the American Board of Multiple Specialties in Podiatry is: (i) to develop and implement national and international standards for and to administer examinations for certification in (a) primary care in podiatric medicine and (b) foot and ankle surgery; (c) prevention and treatment of diabetic foot wounds and diabetic footwear; and (d) limb preservation and salvage; (ii) to grant recognition to individuals who meet the standards; (iii) to monitor the adherence to the standards by podiatrists certified by the corporation; and (iv) to maintain a registry of podiatrists certified by the corporation. American Board of Multiple Specialties in Podiatry Certification Examinations Primary Care in Podiatric Medicine Foot and Ankle Surgery Prevention and Treatment of Diabetic Foot Wounds and Diabetic Footwear Limb Preservation and Salvage STATEMENT OF IMPARTIALITY The ABMSP understands the importance of maintaining impartiality in all of its decision making and certification activities. The ABMSP Board of Directors is responsible for ensuring that the organization carries out its activities in an impartial manner, managing real or perceived conflicts of interest, and insuring objectivity in its decision making process. -
Optometry Career Guide
Optometry A Career Guide Acknowledgments This career guide was written and compiled by the Association of Schools and Colleges of Optometry (ASCO). The guide was written to provide a “core document” that could represent the most current, consistent, and reliable information on optometry as a career for use by prospective students, prehealth advisors, and optometrists who want to share infor- mation about their profession with others. The material is intended for use by ASCO and its member schools and colleges in any format that will make information about optometry accessible and available to those who express interest in the profession. Director, Student and Residency Affairs Association of Schools and Colleges of Optometry 6110 Executive Boulevard, Suite 420 Rockville, MD 20852 optometriceducation.org Updated August 2020 Table of Contents I. DEFINITION OF THE PROFESSION ...................................................................1 II. OUTLOOK FOR THE PROFESSION ..................................................................2 Population Changes and the Optometry Profession ...........................................2 Social and Legal Changes Affecting Optometry ..................................................3 Professional Satisfaction .............................................................................................4 III. NEW FRONTIERS IN EYE CARE ........................................................................5 Lasers .............................................................................................................................5 -

Current Status of Immunology Education in US Schools And
American Journal of Pharmaceutical Education 2019; 83 (7) Article 6994. RESEARCH Current Status of Immunology Education in US Schools and Colleges of Pharmacy Yuan Zhao, PhD,a Dana Ho, PharmD,a Benjamin Oldham, PharmD,a Bonnie Dong, PharmD,a Daniel Malcom, PharmDa,b a Sullivan University College of Pharmacy, Louisville, Kentucky b Associate Editor, American Journal of Pharmaceutical Education, Arlington, Virginia Submitted February 2, 2018; accepted June 17, 2018; published September 2019. Objective. To determine the extent of immunology education in US Doctor of Pharmacy (PharmD) programs. Methods. Curricular information on immunology education was collected from the web pages of US PharmD programs (N5142). The data were sorted, comparisons were made, and trends were identified. Results. Of 142 PharmD programs studied, 100% posted curriculum information on their websites. Among them, 73 programs (51.4%) had a dedicated immunology course in their curriculum, either as an independent course or a course combined with another subject. Most immunology education was offered in the first professional year (72.5%). Of the programs that offered immunology as an in- dependent course, the number of semester hours dedicated to the course varied from 1.5 to 3.5 (median53, mode53, mean52.7). More three-year programs offered immunology as a core compo- nent in the didactic curriculum than did four-year programs (64.7% vs 49.6%). Similarly, more private programs offered immunology than did public programs (64% vs 37.3%). Conclusion. Immunology education in US schools and colleges of pharmacy lacks consensus. Not all PharmD programs indicated they offered specific, focused immunology education in their curricula.