Myelography, Posterior Fossa, Radiological Supervision
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endoscopic Ultrasound for the Diagnosis of Disease and Staging of Cancers in Adult Patients with Gastroenterological Or Oncological Disease: Guidelines
TITLE: Endoscopic Ultrasound for the Diagnosis of Disease and Staging of Cancers in Adult Patients with Gastroenterological or Oncological Disease: Guidelines DATE: 26 February 2014 RESEARCH QUESTION What are the evidence-based guidelines for the use of endoscopic ultrasound in the diagnosis of disease and staging of cancers in adult patient with gastroenterological or oncological disease? KEY MESSAGE Thirteen evidence-based guidelines regarding the use of endoscopic ultrasound in the diagnosis of disease and staging of cancers in adult patient with gastroenterological or oncological disease were identified. METHODS A limited literature search was conducted on key resources including PubMed, The Cochrane Library (2014, Issue 2), University of York Centre for Reviews and Dissemination (CRD) databases, Canadian and major international health technology agencies, as well as a focused Internet search. Methodological filters were applied to limit retrieval to guidelines. The search was also limited to English language documents published between January 1, 2009 and February 11, 2014. Internet links were provided, where available. The summary of findings was prepared from the abstracts of the relevant information. Please note that data contained in abstracts may not always be an accurate reflection of the data contained within the full article. RESULTS Thirteen evidence-based guidelines regarding the staging and diagnosis of cancer and of gastrointestinal diseases were identified. Additional references of potential interest are provided in the appendix. Disclaimer: The Rapid Response Service is an information service for those involved in planning and providing health care in Canada. Rapid responses are based on a limited literature search and are not comprehensive, systematic reviews. -
Introduction to Neuroimaging
Introduction to Neuroimaging Aaron S. Field, MD, PhD Assistant Professor of Radiology Neuroradiology Section University of Wisconsin–Madison Updated 7/17/07 Neuroimaging Modalities Radiography (X-Ray) Magnetic Resonance (MR) Fluoroscopy (guided procedures) • MR Angiography/Venography (MRA/MRV) • Angiography • Diffusion and Diffusion Tensor • Diagnostic MR • Interventional • Perfusion MR • Myelography • MR Spectroscopy (MRS) Ultrasound (US) • Functional MR (fMRI) • Gray-Scale Nuclear Medicine ―Duplex‖ • Color Doppler • Single Photon Emission Computed Tomography (SPECT) Computed Tomography (CT) • Positron Emission Tomography • CT Angiography (CTA) (PET) • Perfusion CT • CT Myelography Radiography (X-Ray) Radiography (X-Ray) Primarily used for spine: • Trauma • Degenerative Dz • Post-op Fluoroscopy (Real-Time X-Ray) Fluoro-guided procedures: • Angiography • Myelography Fluoroscopy (Real-Time X-Ray) Fluoroscopy (Real-Time X-Ray) Digital Subtraction Angiography Fluoroscopy (Real-Time X-Ray) Digital Subtraction Angiography Digital Subtraction Angiography Indications: • Aneurysms, vascular malformations and fistulae • Vessel stenosis, thrombosis, dissection, pseudoaneurysm • Stenting, embolization, thrombolysis (mechanical and pharmacologic) Advantages: • Ability to intervene • Time-resolved blood flow dynamics (arterial, capillary, venous phases) • High spatial and temporal resolution Disadvantages: • Invasive, risk of vascular injury and stroke • Iodinated contrast and ionizing radiation Fluoroscopy (Real-Time X-Ray) Myelography Lumbar or -

Myelography in the Assessment of Degenerative Lumbar Scoliosis And
https://doi.org/10.14245/kjs.2017.14.4.133 KJS Print ISSN 1738-2262 On-line ISSN 2093-6729 CLINICAL ARTICLE Korean J Spine 14(4):133-138, 2017 www.e-kjs.org Myelography in the Assessment of Degenerative Lumbar Scoliosis and Its Influence on Surgical Management George McKay, Objective: Myelography has been shown to highlight foraminal and lateral recess stenosis more Peter Alexander Torrie, readily than computed tomography (CT) or magnetic resonance imaging (MRI). It also has the Wendy Bertram, advantage of providing dynamic assessment of stenosis in the loaded spine. The advent of weight-bearing MRI may go some way towards improving assessment of the loaded spine Priyan Landham, and is less invasive, however availability remains limited. This study evaluates the potential Stephen Morris, role of myelography and its impact upon surgical decision making. John Hutchinson, Methods: Of 270 patients undergoing myelography during 2006-2009, a period representing Roland Watura, peak utilisation of this imaging modality in our unit, we identified 21 patients with degenerative Ian Harding scoliosis who fulfilled our inclusion criteria. An operative plan was formulated by our senior author based initially on interpretation of an MRI scan. Subsequent myelogram and CT myelogram Department of Spinal Surgery, investigations were scrutinised, with any additional abnormalities noted and whether these im- Southmead Hospital, Bristol, United pacted upon the operative plan. Kingdom Results: From our 21 patients, 18 (85.7%) had myelographic findings not identified on MRI. Of Corresponding Author: note, in 4 patients, supine CT myelography yielded additional information when compared to George McKay supine MRI in the same patients. -

Research Article Magnetic Resonance Sialography Findings of Submandibular Ducts Imaging
Hindawi Publishing Corporation BioMed Research International Volume 2013, Article ID 417052, 6 pages http://dx.doi.org/10.1155/2013/417052 Research Article Magnetic Resonance Sialography Findings of Submandibular Ducts Imaging Nezahat Karaca ErdoLan,1 Canan Altay,2 Nesibe Özenler,3 TuLba Bozkurt,1 Engin Uluç,1 Berna Dirim Mete,1 and Esmail Özdemir4 1 Department of Radiology, Izmir Ataturk¨ Research and Training Hospital, Basın Sitesi, Karabaglar,˘ 35360 Izmir, Turkey 2 Department of Radiology, Medical School, Dokuz Eylul University, Inciralti, 35340 Izmir, Turkey 3 Department of Radiology, Balıkesir Ataturk¨ State Hospital, Yıldız Mahallesi Soma Caddesi No. 1, 10100 Balıkesir, Turkey 4 Universal Ege Health Hospital, 35220 Izmir, Turkey Correspondence should be addressed to Canan Altay; [email protected] Received 2 April 2013; Revised 29 May 2013; Accepted 12 June 2013 Academic Editor: Yoshito Tsushima Copyright © 2013 Nezahat Karaca Erdogan˘ et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Purpose. We aimed to assess the problem solving capability of magnetic resonance sialography (MR sialography), a noninvasive method for imaging submandibular gland ducts and determining duct-related pathologies, by comparing diseased and healthy cases. Materials and Methods. We conducted radiological assessment on a total of 60 submandibular glands (mean age 44.7) in 20 cases and 10 volunteers. MR sialography examinations were conducted with single-shot fast spin-echo sequence by using a surface coil placed on the submandibular gland. Each gland was evaluated in terms of the length, width and stricture of the main duct, as well as the difference between the intraparenchymal duct width, and the main duct width. -

Screening for Postmenopausal Osteoporosis
This report may be used, in whole or in part, as the basis for development of clinical practice guidelines and other quality enhancement tools, or a basis for reimbursement and coverage policies. AHRQ or U.S. Department of Health and Human Services endorsement of such derivative products may not be stated or implied. AHRQ is the lead Federal agency charged with supporting research designed to improve the quality of health care, reduce its cost, address patient safety and medical errors, and broaden access to essential services. AHRQ sponsors and conducts research that provides evidence-based information on health care outcomes; quality; and cost, use, and access. The information helps health care decisionmakers— patients and clinicians, health system leaders, and policymakers—make more informed decisions and improve the quality of health care services. Systematic Evidence Review Number 17 Screening for Postmenopausal Osteoporosis Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 2101 East Jefferson Street Rockville, MD 20852 http://www.ahrq.gov Contract No. 290-97-0018 Task Order No. 2 Technical Support of the U.S. Preventive Services Task Force Prepared by: Oregon Health Sciences University Evidence-based Practice Center, Portland, Oregon Heidi D. Nelson, MD, MPH Mark Helfand, MD, MS September 2002 Preface The Agency for Healthcare Research and Quality (AHRQ) sponsors the development of Systematic Evidence Reviews (SERs) through its Evidence-based Practice Program. With ∗ guidance from the third U.S. Preventive Services Task Force (USPSTF) and input from Federal partners and primary care specialty societies, two Evidence-based Practice Centers—one at the Oregon Health Sciences University and the other at Research Triangle Institute-University of North Carolina—systematically review the evidence of the effectiveness of a wide range of clinical preventive services, including screening, counseling, immunizations, and chemoprevention, in the primary care setting. -

Clinical Review Karen Bleich NDA 020351 Supplement 44 (CCTA) Visipaque (Iodixanol)
Clinical Review Karen Bleich NDA 020351 Supplement 44 (CCTA) Visipaque (iodixanol) CLINICAL REVIEW Application Type Supplemental New Drug Application Application Number(s) NDA 020351 s44 Priority or Standard Priority Submit Date(s) October 6th, 2016 Received Date(s) October 18th, 2016 PDUFA Goal Date April 5th, 2017 Division/Office Division of Medical Imaging Products/Office of Drug Evaluation IV Reviewer Name(s) Karen Bleich, MD Review Completion Date March 10th, 2017 Established Name Iodixanol (Proposed) Trade Name Visipaque Injection Applicant GE Healthcare Formulation(s) 320 mgI/mL Dosing Regimen 70-80 mL main bolus volume (does not include optional test bolus volume of 20 mL) at a flow rate of(b) (4) mL/s, followed by 20 mL saline flush Applicant Proposed For use in coronary computed tomography angiography (CCTA) to Indication(s)/Population(s) assist in the diagnostic evaluation of patients with suspected coronary artery disease. Recommendation on Approval Regulatory Action Recommended For use in coronary computed tomography angiography (CCTA) to Indication(s)/Population(s) assist in the diagnostic evaluation of patients with suspected (if applicable) coronary artery disease. CDER Clinical Review Template 2015 Edition 1 Reference ID: 4068412 Clinical Review Karen Bleich NDA 020351 Supplement 44 (CCTA) Visipaque (iodixanol) Table of Contents Glossary ........................................................................................................................................... 8 1 Executive Summary .............................................................................................................. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Three-Way Comparative Study of Endoscopic Ultrasound-Guided
Surgical Endoscopy (2019) 33:1260–1270 and Other Interventional Techniques https://doi.org/10.1007/s00464-018-6406-7 Three-way comparative study of endoscopic ultrasound-guided transmural gallbladder drainage using lumen-apposing metal stents versus endoscopic transpapillary drainage versus percutaneous cholecystostomy for gallbladder drainage in high-risk surgical patients with acute cholecystitis: clinical outcomes and success in an International, Multicenter Study Ali Siddiqui1 · Rastislav Kunda3 · Amy Tyberg2 · Mustafa A. Arain4 · Arish Noor1 · Tayebah Mumtaz1 · Usama Iqbal1 · David E. Loren1 · Thomas E. Kowalski1 · Douglas G. Adler5 · Monica Saumoy2 · Monica Gaidhane2 · Shawn Mallery4 · Eric M. Christiansen4 · Jose Nieto6 · Michel Kahaleh2 Received: 9 November 2017 / Accepted: 24 August 2018 / Published online: 12 September 2018 © Springer Science+Business Media, LLC, part of Springer Nature 2018 Abstract Background Percutaneous cholecystostomy tube (PTGBD), endoscopic retrograde cholangiopancreatography with trans- papillary gallbladder drainage (TP), and endoscopic ultrasound-guided transmural gallbladder drainage (EGBD) using lumen-apposing metal stents (LAMS) have been offered for gallbladder decompression for acute cholecystitis in high-risk surgical patients. Yet, there are limited data comparing these therapies. Our aim was to compare the safety and efficacy of EGBD to TP and PTGBD for gallbladder drainage. Methods We retrospectively collected high-risk surgical patients from six centers with acute cholecystitis who underwent gallbladder drainage by EGBD, TP, or PTGBD. Data included technical success (gallbladder drainage), clinical success (acute cholecystitis resolution), adverse events (AE), and follow-up. Results From 2010 to 2016, 372 patients underwent gallbladder drainage, with 146 by PTGBD, 124 by TP, and 102 drained by EGBD. Technical (98% vs. 88% vs. 94%; p = 0.004) and Clinical (97% vs. -

Impact of Preoperative Endoscopic Ultrasound in Surgical Oncology
REVIEW Impact of preoperative endoscopic ultrasound in surgical oncology Endoscopic ultrasound (EUS) has a strong impact on the imaging and staging of solid tumors within or in close proximity of the upper GI tract. Technological developments during the last two decades have increased the image quality and allowed very detailed visualization of local tumor spread and lymph node affection. Current indications for EUS of the upper GI tract encompass the differentiation between benign and malignant lesions, the staging of esophageal, gastric and pancreatic cancer, and the procurement of a biopsy specimen through fine-needle aspiration. Various technical innovations during the past two decades have increased the diagnostic quality and have simultaneously strengthened the role of EUS in the clinical setting. This article will give a compressed summary on the current state of EUS and possible further technical developments. 1 KEYWORDS: 3D imaging elastosonography endoscopic ultrasound miniprobes Sascha S Chopra & oncologic surgery Michael Hünerbein† 1Department of General & Transplantation Surgery, Charité Campus Virchow-Clinic, Berlin, Conventional endoscopic ultrasound the so-called ‘miniprobes’ into the biliary system Germany Linear versus radial systems or the pancreatic duct in order to obtain high-res- †Author for correspondence: Department of Surgery & Surgical Endoscopic ultrasound (EUS) with flex- olution radial ultrasound images locally. Present Oncology, Helios Hospital Berlin, ible endoscopes is an important diagnostic and mini probes show a diameter of 2–3 mm and oper- 13122 Berlin, Germany Tel.: +49 309 417 1480 therapeutic tool, especially for the local staging ate with frequencies between 12 and 30 MHz. Fax: +49 309 417 1404 of gastrointestinal (GI) cancers, the differen- The main drawbacks of these devices are the lim- michael.huenerbein@ tiation between benign and malignant tumors, ited durability and the decreased depth of penetra- helios-kliniken.de and interventional procedures, such as biopsies tion (~2 cm). -

Treatment of Spinal Cord Vascular Malformations by Surgical Excision
J. Neurosurg. / Volume 30 / April, 1969 Treatment of Spinal Cord Vascular Malformations by Surgical Excision H. KRAYENBOHL, M. G. YA~ARGIL, M.D., AND H. G. McCLINTOCK* Section v] Neurosurgery, Kantonsspital, The University o] Ziirich, Ziirich, Switzerland ECENT developments have now made called attention to an increase in symptoms direct surgical attack the treatment during pregnancy with subsidence after of choice for spinal cord vascular delivery, z~ Newman has stated that he be- malformations. We are reporting 17 cases lieves the increase in symptoms in such cases treated with surgical excision, the last 11 of may be due to "venous congestion" from the which were operated on under the operating distended uterus and interestingly suggests microscope. the possibility of some "hormonal factor act- There is much confusion in the literature ing on the vessel walls. ''22 Although none of concerning the histological nomenclature our cases was a child, several authors have used to describe varieties of spinal vascular reported the occurrence in children and even malformations. This confusion is partly the in infants?, ~, 10,22,23 result of the lack of opportunity for ade- quate microscopic study of the entire lesion. Clinical Picture We prefer to follow the classification of History. The clinical history is usually one Bergstrand, et al.2 who divided these malfor- of three types. There can be 1) a slow mations into: 1) angioma cavernosum, 2) progression of neurological symptoms and angioma racemosum, and 3) angioreticu- signs, 2) progression followed with regres- loma. Some vascular malformations will sion or a stationary period, or 3) a sudden show characteristics of more than one group, apoplectic onset. -
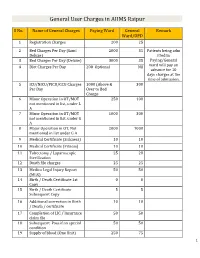
General User Charges in AIIMS Raipur
General User Charges in AIIMS Raipur S No. Name of General Charges Paying Ward General Remark Ward/OPD 1 Registration Charges 200 25 2 Bed Charges Per Day (Sami 2000 35 Patients being adm Deluxe) itted in 3 Bed Charges Per Day (Deluxe) 3000 35 Paying/General 4 Diet Charges Per Day 200 Optional Nil ward will pay an advance for 10 days charges at the time of admission. 5 ICU/NICU/PICU/CCU Charges 1000 (Above & 300 Per Day Over to Bed Charge 6 Minor Operation in OT/MOT 250 100 not mentioned in list, under L A 7 Minor Operation in OT/MOT 1000 300 not mentioned in list, under G A 8 Major Operation in OT, Not 2000 1000 mentioned in list under G A 9 Medical Certificate (Sickness) 10 10 10 Medical Certificate (Fitness) 10 10 11 Tubectomy / Laparoscopic 25 20 Sterilization 12 Death file charges 25 25 13 Medico Legal Injury Report 50 50 (MLR) 14 Birth / Death Certificate 1st 0 0 Copy 15 Birth / Death Certificate 5 5 Subsequent Copy 16 Additional correction in Birth 10 10 / Death / certificate 17 Completion of LIC / Insurance 50 50 claim file 18 Subsequent Pass if on special 50 50 condition 19 Supply of blood (One Unit) 250 75 1 20 Medical Board Certificate 500 500 On Special Case User Charges for Investigations in AIIMS Raipur S No. Name of Investigations Paying General Remark Ward Ward/OPD Anaesthsia 1 ABG 75 50 2 ABG ALONGWITH 150 100 ELECTROLYTES(NA+,K+)(Na,K) 3 ONLY ELECTROLYTES(Na+,K+,Cl,Ca+) 75 50 4 ONLY CALCIUM 50 25 5 GLUCOSE 25 20 6 LACTATE 25 20 7 UREA. -

A-Scan Echoencephalography in Measurement of the Cerebral Ventricles
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.31.3.245 on 1 June 1968. Downloaded from J. Neurol. Neurosurg. Psychiat., 1968, 31, 245-249 A-scan echoencephalography in measurement of the cerebral ventricles ANAND G. GARG AND ALEX. R. TAYLOR From the Department ofNeurological Surgery, Royal Victoria Hospital, Belfast, Northern Ireland The first attempts at ultrasonic visualization of the METHOD cerebral ventricles were made by Dussik (1948), The ventricular measurements obtained at echoen- Ballantine, Ludwig, Bolt, and Hueter (1950), and cephalography were compared with the x-ray measure- Hueter and Bolt (1951), using the transmission ments made at pneumoencephalography. method. The possible use of the pulse-echo method ANATOMICAL CONSIDERATIONS The third and lateral (echoencephalography) for the diagnosis of hy- ventricles are supratentorial structures. The third ventricle lies between the two thalmi, communicating drocephalus was suggested by Leksell (1956). Later in front with the lateral ventricles through the inter- Kikuchi, Uchida, Tanaka, and Wagai (1957) and de ventricular foramina and behind with the aqueduct of Vlieger and Ridder (1959) recorded echoes from the the midbrain. The septum lucidum and the third ventricle walls of the lateral ventricles. According to Gordon lie in the central plane of the brain. Protected by copyright. (1959), and de Vlieger and Ridder (1959), the width The lateral ventricle is a C-shaped cavity lying within of the third ventricle can also be measured. ter the cerebral hemisphere. It consists of a central body and Braak, Crezde, Grandia, and de Vleger (1961) used three horns-anterior, posterior, and temporal-running pneumoencephalography to study the origin of into the frontal, occipital, and temporal lobes respec- ventricular echoes.