MLN Connects for Thursday, January 21, 2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Quick Guide – DSP & Supervisor Increases Effective January 1, 2021
NJ Department of Human Services Division of Developmental Disabilities Quick Guide – DSP & Supervisor Increases Effective January 1, 2021 Service Service Procedure FY20 FY21 FY21 Rate FY21 FY21 Rate Description / Tier Code Rate Rate Total Rate DSP Supervisor Increase Increase Increase Career Planning Career Planning H2014HI 13.83 14.25 0.42 0.31 0.11 Community Tier A H2015HIU1 2.54 2.63 0.09 0.07 0.02 Inclusion Services Tier B H2015HIU2 3.23 3.35 0.12 0.09 0.03 Tier C H2015HIU3 4.00 4.14 0.14 0.10 0.04 Tier D H2015HIU4 5.93 6.14 0.21 0.16 0.05 Tier E H2015HIU5 7.87 8.15 0.28 0.21 0.07 Tier F H2015HIU7 11.80 12.22 0.42 0.31 0.11 Community-Based CBS H2021HI 7.41 7.83 0.42 0.31 0.11 Supports CBS (Acuity) H2021HI22 12.43 12.85 0.42 0.31 0.11 Day Habilitation Tier A T2021HIUS 2.54 2.63 0.09 0.07 0.02 Tier A/Acuity T2021HIU1 3.67 3.75 0.08 0.06 0.02 Differentiated Tier B T2021HIUR 3.23 3.35 0.12 0.09 0.03 Tier B /Acuity T2021HIU2 4.67 4.78 0.11 0.08 0.03 Differentiated Tier C T2021HIUQ 4.00 4.14 0.14 0.10 0.04 Tier C/Acuity T2021HIU3 5.78 5.92 0.14 0.10 0.04 Differentiated Tier D T2021HIUP 5.93 6.14 0.21 0.16 0.05 Tier D/Acuity T2021HIU4 8.56 8.77 0.21 0.16 0.05 Differentiated Tier E T2021HIUN 7.87 8.15 0.28 0.21 0.07 Tier E/Acuity T2021HIU5 11.36 11.64 0.28 0.21 0.07 Differentiated Tier F T2021HI22 11.80 12.22 0.42 0.31 0.11 Tier F/Acuity T2021HIU7 17.04 17.46 0.42 0.31 0.11 Differentiated Individual Supports Individual H2016HI 7.41 7.83 0.42 0.31 0.11 Supports Individual H2016HI22 12.43 12.87 0.44 0.33 0.11 Supports Acuity Tier A H2016HI52 -

New Measures for Border Enforcement (7) January 13, 2021
(Provisional translation) New measures for border enforcement (7) January 13, 2021 Based on “Phased Measures toward Resuming Cross-Border Travel” (referred in the document 2 of the 38th meeting of Novel Coronavirus Response Headquarters on June 18, 2020) and “Resumption of Cross-Border Travel and other measures” (referred in the document 3 of the 41st meeting of Novel Coronavirus Response Headquarters on July 22, 2020), the Government of Japan (GOJ) has permitted a new entry to Japan on an exceptional basis (“Residence Track”) and has partially relaxed restrictions on movement by limiting a range of activities during the period of 14-day quarantine at home or other designated locations (“Business Track”) under the condition that the person is sponsored by a company/entity that is able to ensure observance of the quarantine measures. However, the operation of “Business Track” and “Residence Track” with all the countries/regions covered under the framework will be suspended. The new entry of foreign nationals into Japan under these two tracks will not be permitted and the relaxation of restrictions on movement during the period of 14-day quarantine through “Business Track” will no longer be permitted for Japanese nationals and foreign nationals with the status of residence until the state of emergency declaration is lifted. Note 1: The quarantine measures mentioned above will be implemented at 0:00 am (JST) on January 14, 2021. Note 2: Holders of valid visas already issued under “Business Track” or “Residence Track” are in principle permitted to enter Japan until 0:00 am (JST) on January 21, 2021, except for those who have stayed in the United Kingdom or the Republic of South Africa within 14 days prior to the entry into Japan. -

BOARD of COUNTY COMMISSIONERS January 26, 2021 OPEN SESSION AGENDA
Jeffrey A. Cline, President Wayne K. Keefer Terry L. Baker, Vice President Cort F. Meinelschmidt Krista L. Hart, Clerk Randall E. Wagner 100 West Washington Street, Suite 1101 | Hagerstown, MD 21740-4735 | P: 240.313.2200 | F: 240.313.2201 WWW.WASHCO-MD.NET BOARD OF COUNTY COMMISSIONERS January 26, 2021 OPEN SESSION AGENDA In response to the existing State of Emergency, this meeting of the Board of County Commissioners will be conducted with a virtual component allowing for Commissioner and Staff participation via remote video conference. The meeting will be live streamed on the County’s YouTube and Facebook sites. 10:00 AM MOMENT OF SILENCE AND PLEDGE OF ALLEGIANCE CALL TO ORDER, President Jeffrey A. Cline APPROVAL OF MINUTES: January 12, 2021 10:05 AM COMMISSIONERS’ REPORTS AND COMMENTS 10:15 AM STAFF COMMENTS 10:20 AM REQUEST FOR INCREASE IN RATE OF PAY FOR CIRCUIT COURT BAILIFFS – Honorable Judge Daniel P. Dwyer, Administrative Judge; Kristin Grossnickle, Court Administrator, Circuit Court for Washington County 10:30 AM CONTRACT RENEWAL (PUR1403) LANDFILL INSPECTION SERVICES – Rick Curry, Director, Purchasing; Dave Mason, Deputy Director, Solid Waste 10:35 AM FISCAL YEAR 2022 RURAL LEGACY PROGRAM GRANT – Chris Boggs, Land Preservation Planner, Planning & Zoning; Allison Hartshorn, Grant Manager, Grant Management 10:40 AM HOOD CONSERVATION RESERVE ENHANCEMENT PROGRAM EASEMENT – Chris Boggs, Land Preservation Planner, Planning & Zoning 10:45 AM JOINT RESOLUTION AND AMENDMENT TO CONSOLIDATED GENERAL SERVICES AGREEMENT – Mark Bradshaw, -

Federal Register/Vol. 86, No. 12/Thursday, January 21, 2021/Notices
Federal Register / Vol. 86, No. 12 / Thursday, January 21, 2021 / Notices 6363 was enlarged in 1938 by Presidential and associated pull-outs, and all paved minimum path width of ten feet with a Proclamation to include protection of parking areas. Additionally, the GMP two-foot shoulder, a five percent prehistoric structures of historic and outlines five interpretive themes, one of maximum running slope grade, and a scientific interest. The Monument was which includes safety. When the Park safety railing adjacent to steep slopes. enlarged two more times in 1960 by entrance road was expanded in 2017, it Signage will be installed to warn trail Presidential Proclamation 3360 and in did not include a shoulder lane nor a users of safety hazards. The trail would 1969 by Presidential Proclamation 3887 separate lane for bicyclists or provide a much safer alternative for stating that it would be ‘‘in the public pedestrians. Bicyclists accessing the bicyclists who now must enter the Park interest to add to Arches certain Park from the nearby town of Moab, on the narrow shoulder of the entrance contiguous lands on which outstanding Utah ride on a shared use path for two road. The NPS will monitor activities on geological features of great scientific miles from the trail hub in town and the trail and make safety-related interest are situated and certain other then exit the path and enter the Park adjustments, as needed. lands adjacent to the monument which along the narrow and unsafe shoulder of are essential to the proper care, the 0.625-mile-long entrance road. -
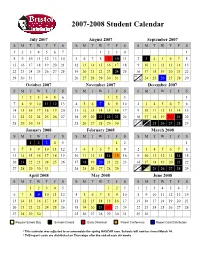
Approved Student Calendar
2007-2008 Student Calendar July 2007 August 2007 September 2007 SMTWT F S SMTWT F S SMTWT F S 1234567 1234 1 8910111213145678910 11 2 3 45678 15 16 17 18 19 20 21 12 13 14 15 16 17 18 9 10 11 12 13 14 15 22 23 24 25 26 27 28 19 20 21 22 23 24 25 16 17 18 19 20 21 22 23 29 30 31 26 27 28 29 30 31 30 24 25 26 27 28 29 October 2007 November 2007 December 2007 SMTWT F S SMTWT F S SMTWT F S 123456 123 1 7891011 12 134567 89102345678 14 15 16 17 18 19 20 11 12 13 14 15 16 17 9 10 11 12 13 14 15 21 22 23 24 25 26 27 18 19 20 21 22 23 24 16 17 18 19 20 21 22 23 24 28 29 30 31 25 26 27 28 29 30 30 31 25 26 27 28 29 January 2008 February 2008 March 2008 SMTWT F S SMTWT F S SMTWT F S 12345 12 1 67891011123456789 2345678 13 14 15 16 17 18 19 10 11 12 13 14 1516 9 1011121314 15 20 21 22 23 24 25 26 17 18 19 20 21 22 23 16 17 18 19 20 21 22 23 24 27 28 29 30 31 24 25 26 27 28 29 30 31 25 26 27 28 29 April 2008 May 2008 June 2008 SMTWT F S SMTWT F S SMTWT F S 12345 123 1234567 6789 10111245678910891011121314 13 14 15 16 17 18 19 11 12 13 14 15 16 17 15 16 17 18 19 20 21 20 21 22 23 24 25 26 18 19 20 21 22 23 24 22 23 24 25 26 27 28 27 28 29 30 25 26 27 28 29 30 31 29 30 Regular School Day Schools Closed Early Dismissal Parent Conference Report Card Distribution * This calendar was adjusted to accommodate the spring NASCAR race. -

Advisory Committee Minutes January 21, 2021
TOWN OF SCITUATE 600 Chief Justice Cushing Highway Scituate, Massachusetts 02066 Phone: 781-545-8716 FAX: 781-545-8704 Advisory Committee Meeting Minutes Thursday, January 21, 2021 Zoom Video/Audio Conference -- 7:00 pm Meeting conducted pursuant to the March 12, 2020 modifications to the Open Meeting Law made by Governor Baker pursuant to the state of emergency due to COVID-19. Committee Members Present: Jerry Kelly; Chair, Elise Russo, Mike Westort, Jamie Gilmore, Dan McGuiggin, Lynda Ferguson, Missy Seidel, Lincoln Heineman, Patrice Metro Also in Attendance: Finance Director; Nancy Holt, Town Administrator; Jim Boudreau, Recording Secretary; Alicia Anthony, SCTV Director; Seth Pfeiffer, SCTV Staff; Briana Trifiro, Town Planner; Karen Joseph, Director of Information Technology; Michael Minchello, Veteran Services Director; Don Knapp, Beautification Committee Chair People; Sytske Humphrey and Leslie Dienel, Historical Chair Person; Robert Chessia Committee Members Not In Attendance: none Jerry Kelly called the meeting to order at 7:02 p.m. which was seconded by Jamie and voted all in favor (9-0) by roll call vote; UNANIMOUS. Jerry Kelly made a motion to accept the minutes from the January 7, 2021 and the minutes from the January 14, 2021 meetings, that was seconded by (????) and voted all in favor (9- 0) by roll call vote; UNANIMOUS. FY22 Budget Presentation: Community Planning & Development o Planning (175) Karen Joseph, Town Planner Ms. Joseph said that they are working on their master plan and The Master Plan Advisory Committee is working with them. She stated that they are working on zoning before town meeting, saying that North Scituate Village Zoning Code Public Hearing is scheduled for 2/11 @ 7 p.m. -
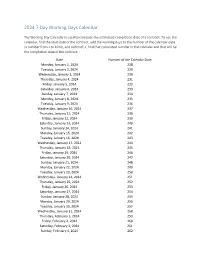
2024 7 Day Working Days Calendar
2024 7 Day Working Days Calendar The Working Day Calendar is used to compute the estimated completion date of a contract. To use the calendar, find the start date of the contract, add the working days to the number of the calendar date (a number from 1 to 1000), and subtract 1, find that calculated number in the calendar and that will be the completion date of the contract Date Number of the Calendar Date Monday, January 1, 2024 228 Tuesday, January 2, 2024 229 Wednesday, January 3, 2024 230 Thursday, January 4, 2024 231 Friday, January 5, 2024 232 Saturday, January 6, 2024 233 Sunday, January 7, 2024 234 Monday, January 8, 2024 235 Tuesday, January 9, 2024 236 Wednesday, January 10, 2024 237 Thursday, January 11, 2024 238 Friday, January 12, 2024 239 Saturday, January 13, 2024 240 Sunday, January 14, 2024 241 Monday, January 15, 2024 242 Tuesday, January 16, 2024 243 Wednesday, January 17, 2024 244 Thursday, January 18, 2024 245 Friday, January 19, 2024 246 Saturday, January 20, 2024 247 Sunday, January 21, 2024 248 Monday, January 22, 2024 249 Tuesday, January 23, 2024 250 Wednesday, January 24, 2024 251 Thursday, January 25, 2024 252 Friday, January 26, 2024 253 Saturday, January 27, 2024 254 Sunday, January 28, 2024 255 Monday, January 29, 2024 256 Tuesday, January 30, 2024 257 Wednesday, January 31, 2024 258 Thursday, February 1, 2024 259 Friday, February 2, 2024 260 Saturday, February 3, 2024 261 Sunday, February 4, 2024 262 Date Number of the Calendar Date Monday, February 5, 2024 263 Tuesday, February 6, 2024 264 Wednesday, February -

Smith Branch Monitoring Sites Monitoring Data Summary for February 15Th, 2018 – March 27Th, 2018
Smith Branch Monitoring Sites Monitoring Data Summary for February 15th, 2018 – March 27th, 2018 Data Gaps • During this monitoring period, there were periods of fouling turbidity data observed at both SMIA and SMIB that was removed from the dataset. • At the SMIB station, the specific conductivity sensor and temperature sensor became unsubmerged. During periods where the specific conductivity and temperature sensors were unsubmerged, DO and pH values, which are temperature dependent, were removed from the dataset. SCDHEC Standards • The SMIA station recorded a minimum pH value of 5.6. These low pH values occurred during the storm event on March 20th. • The SMIB station did not record any pH readings outside of the acceptable SCDHEC range of 6 to 8.5. • The SMIA and SMIB stations recorded average DO concentrations of 7.9 mg/L and 9.2 mg/L, respectively, which are well above the SCDHEC daily average standard of 5 mg/L. • The minimum DO concentrations were 5.0 mg/L and 6.8 mg/L at the SMIA and SMIB stations, respectively, which are both above the SCDHEC minimum level of 4 mg/L. Storm Events • Both Smith Branch stations recorded seven storms (at least 0.1 inches) in this monitoring period that resulted in 3.4 inches of precipitation at SMIA and 3.2 inches of precipitation at SMIB. • The Smith Branch monitoring stations both recorded typical water quality responses to the storm events observed during this monitoring period. • The maximum antecedent dry time since the last significant precipitation event (at least 0.1 inch) was approximately 17.7 days prior to the February 25th storm event at SMIA and 20.8 days prior to the February 28th storm event at SMIB. -

Pricing*, Pool and Payment** Due Dates January - December 2021 Mideast Marketing Area Federal Order No
Pricing*, Pool and Payment** Due Dates January - December 2021 Mideast Marketing Area Federal Order No. 33 Class & Market Administrator Payment Dates for Producer Milk Component Final Pool Producer Advance Prices Payment Dates Final Payment Due Partial Payment Due Pool Month Prices Release Date Payrolls Due & Pricing Factors PSF, Admin., MS Cooperative Nonmember Cooperative Nonmember January February 3 * February 13 February 22 December 23, 2020 February 16 ** February 16 February 17 Janaury 25 January 26 February March 3 * March 13 March 22 January 21 * March 15 March 16 March 17 February 25 February 26 March March 31 * April 13 April 22 February 18 * April 15 April 16 April 19 ** March 25 March 26 April May 5 May 13 May 22 March 17 * May 17 ** May 17 ** May 17 April 26 ** April 26 May June 3 * June 13 June 22 April 21 * June 15 June 16 June 17 May 25 May 26 June June 30 * July 13 July 22 May 19 * July 15 July 16 July 19 ** June 25 June 28 ** July August 4 * August 13 August 22 June 23 August 16 ** August 16 August 17 July 26 ** July 26 August September 1 * September 13 September 22 July 21 * September 15 September 16 September 17 August 25 August 26 September September 29 * October 13 October 22 August 18 * October 15 October 18 ** October 18 ** September 27 ** September 27 ** October November 3 * November 13 November 22 September 22 * November 15 November 16 November 17 October 25 October 26 November December 1 * December 13 December 22 October 20 * December 15 December 16 December 17 November 26 ** November 26 December January 5, 2022 January 13, 2022 January 22, 2022 November 17 * January 18, 2022 ** January 18, 2022 ** January 18, 2022 ** December 27 ** December 27 ** * If the release date does not fall on the 5th (Class & Component Prices) or 23rd (Advance Prices & Pricing Factors), the most current release preceding will be used in the price calculation. -

January 21, 2021 Finance Committee Meeting Agenda
NOTICE OF FINANCE COMMITTEE MEETING Thursday, January 21, 2021 4:00 pm Park District of Highland Park Board of Park Commissioners West Ridge Center 636 Ridge Road Highland Park, IL 60035 FINANCE COMMITTEE MEETING AGENDA The Governor has issued a disaster declaration related to public health concerns because of COVID-19, and all or part of the jurisdiction the Park District of Highland Park is covered by the disaster area. The President of the Board of Park Commissioners has determined that an in-person meeting conducted under this Act is not practical or prudent because of said disaster. Likewise, in compliance with the capacity limitations caused by the disaster, public attendance at the meeting is not feasible. Therefore, the Board of Park Commissioners have made alternative arrangements in the manner described below to allow any interested member of the public access to contemporaneously hear all discussion, testimony, and roll call votes. Members of the public may view a live stream of the Finance Committee Meeting by clicking the Thursday, January 21 Finance Committee Meeting Video link found at https://www.pdhp.org/park-board/meetings/ I. CALL TO ORDER II. ROLL CALL III. PUBLIC COMMENT FOR ITEMS ON AGENDA For public comment, members of the public should email Brian Romes, Executive Director, at [email protected]. Emails should be sent between Tuesday, January 19 at 4:00 p.m. until 3:45 p.m. on Thursday, January 21 and should have “Public Comment for January 21 Finance Committee Meeting” in the subject line of the email. Comments will be read aloud during the meeting. -

February 15, 2021
This newsletter will be posted each Monday during the Bowling season (1/04/21 – 3/08/21) + 11/30 and 12/14 #8 –February 15, 2021 REGIONAL HOSTS/ASSIGNMENTS (REPEAT) https://www.kshsaa.org/Public/Bowling/pdf/ASSIGNMENTS.pdf SCHEDULE FOR REGIONAL BOWLING TOURNAMENTS Tuesday, 2/23 - 6A @ Olathe Lanes East - Olathe East HS Tuesday, 2/23 - 5-1A @ Walnut Bowl, Great Bend - Great Bend HS Wednesday, 2/24 - 5-1A @ The Alley, Wichita - Andover HS Wednesday, 2/24 - 5-1A @ Crown Lanes, Leavenworth - Basehor Linwood HS Wednesday, 2/24 - 6A @ Mission Bowl, Olathe - Shawnee Mission-East HS Thursday, 2/25 - 6A @ West Acres, Wichita - Wichita-Northwest HS Thursday, 2/25 - 5-1A @ Olathe-Lanes East (PM) - OP-St. Thomas Aquinas HS Friday, 2/26 - 5-1A @ Olathe Lanes East (AM) - OP-St. Thomas Aquinas HS Friday, 2/26 - 5-1A @ Gage Bowl, Topeka - Tecumseh-Shawnee Heights HS Friday, 2/26 - 6A @ West Ridge Lanes, Topeka - Topeka-Washburn Rural HS Friday, 2/26 - 5-1A @ West Acres, Wichita - Wichita-Bishop Carroll Friday, 2/26 - 5-1A @ The Alley, Wichita - Wichita-Collegiate HS TIME SCHEDULE FOR REGIONAL TOUNAMENTS (REPEAT) NOTE: Please do not arrive at your tournament site until the printed time below. MORNING TIME SCHEDULE 7:45 AM- Teams Arrive at Center 8:05 - Morning Session Coaches Mtg. 8:25 - Welcome, National Anthem, Team Introductions, etc. 8:40 - Warm-up 8:50 - Competition Begins (3 American Tenpin games followed by 4 Baker games) 11:30 - Competition completed; Coaches check bowlers scores; Bowlers & coaches leave center BOWLING CENTER CLEARED, CLEANED & LANES RE-OILED FOR NEXT SESSION AFTERNOON TIME SCHEDULE 12:45 PM- Teams Arrive at Center 1:05 - Afternoon Session Coaches Mtg. -

State Daily Infections Per 100K Effective Dates
Chicago Emergency Travel Order State by State List The list is updated every other Tuesday and goes into effect the following Friday at 12:01 a.m. Daily Infections Effective Dates – Effective Dates – State Per 100k Red List Orange List December 14 – January January 11 – 10 Arizona November 13 – December 95.6 13 January 1 – January 10 January 11 – South Carolina November 13 – December 83.6 31 December 4 – January January 11 – 10 Rhode Island November 13 – December 71.4 3 January 1 – January 10 January 11 – Georgia November 13 – December 68.5 31 January 1 – January 10 January 11 – New York November 13 – December 67.9 31 December 14 – January January 11 – 10 Kentucky November 13 – December 63.7 13 December 4 – January January 11 – 10 Oklahoma November 13 – December 63.4 3 December 14 – January January 11 – 10 Delaware November 13 – December 62.8 13 January 1 – January 10 January 11 – North Carolina November 13 – December 62.4 31 December 14 – January January 11 – Arkansas 61.3 10 November 13 – December 13 December 14 – January January 11 – 10 California November 13 – December 60.3 13 January 1 – January 10 January 11 – Texas November 20 – December 60.2 31 December 14 – January 11 – December 31 Connecticut November 13 – December 57.7 13 December 14 – January January 11 – 10 New Hampshire November 20 – December 57.5 13 December 14 – January January 11 – 10 Massachusetts November 13 – December 57.2 13 January 1 – January 10 January 11 – New Jersey November 13 – December 57.2 31 November 13 – January January 11 – Utah 56 10 December 14 –January