Metrics to Drive Improvements in Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Profiles of State All-Payer Claims Databases
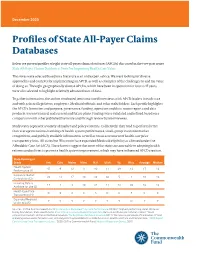
December 2020 Profiles of State All-Payer Claims Databases Below we present profiles of eight state all-payer claims databases (APCDs) discussed in the two-part series State All-Payer Claims Databases: Tools for Improving Health Care Value. The states were selected based on a literature scan and expert advice. We were looking for diverse approaches and contexts for implementing an APCD, as well as examples of the challenges to and the value of doing so. The eight geographically diverse APCDs, which have been in operation for four to 17 years, were also selected to highlight relatively advanced uses of data. To gather information, the author conducted semistructured interviews with APCD leaders in each state and with selected legislators, employers, Medicaid officials, and other stakeholders. Each profile highlights the APCD’s formation and purpose, governance, funding, operation and data, recent reports and data products, lessons learned, and current and future plans. Findings were validated and refined based on a comparison with other published literature and through review by interviewees. Study states represent a variety of market and policy contexts. Collectively, they tend to perform better than average on national rankings of health system performance, small-group insurance market competition, and publicly available information, as well as on an assessment of health care price transparency laws. All states but Wisconsin have expanded Medicaid eligibility as allowed under the Affordable Care Act (ACA). These factors suggest that most of the states are amenable to adopting health reforms and policies to promote health system improvement, which may have influenced APCD creation. State Ranking or Grade Ark. -
A Sustainable Business Model for Health Information Exchange Platforms: the Solution to Interoperability in Healthcare IT1 Niam Yaraghi
JANUARY 2015 A Sustainable Business Model for Health Information Exchange Platforms: The Solution to Interoperability in Healthcare IT1 Niam Yaraghi INTRODUCTION Timely access to patients’ medical records helps physicians to make better decisions. They can provide their patients with higher quality of care and avoid many redundant and often harmful medical procedures. Fewer redundancies and medical errors will naturally lead to the much needed savings in the health care system. A nationwide network in which all of the medical providers can access the medical records of their patients is estimated to save up to $81 billion in annual costs (Hillestad et al., 2005). Niam Yaraghi is a The most recent efforts to promote health care IT started in 2004 by the executive order of fellow in the Brookings Institution’s Center for President George W. Bush to establish the Office of National Coordinator for Health IT (ONC). Five Technology Innovation. He is an expert on years later, this position was legislatively mandated as a part of Health Information Technology economics of healthcare for Economic and Clinical Health (HITECH) Act. President Obama’s administration knew very well information technology with a focus on Health that reforming the health care system starts with building the nation’s infrastructure of health Information Exchange (HIE) systems. care IT. To achieve this goal, the federal government has already spent over $27 billion as financial incentives to promote the adoption and use of modern IT systems among health care professionals (Galbraith, 2013). Although the generous federal incentives have led the majority of health care providers to adopt basic Electronic Health Record (EHR) systems, they rarely exchange their medical information with each other (Furukawa et al., 2014). -

Decision Support in the Emerging Pay-For-Value World
Title Decision Support In The Emerging Pay-For-Value World: An Essential Element Of Market Place Success Decision Support In The Emerging Pay-For-Value World 1 What Is Driving The Need For Decision Support? The Increasingly Pay-For-Value World Of Health & Human Service Organizations The Patient Protection and Affordable Care Act (PPACA) has sparked a revolution: health care is shifting from a fee-for-service (“pay-for-volume”) model to one in which services are reimbursed based upon the health value they bring to the consumer (“pay-for-value”). In this new market, payers and consumers are evaluated for value against the yardstick of “The Triple Aim:” better care, reduced costs, and improved patient satisfaction.i Transition From A Fee-for-Service to Pay-for-Performance Reimbursement Case Rates & Capitation & Pay-For- Fee-For-Service Bundled Population Performance Payments Payments (P4P) While the U.S. health and human services system has seen change before, a perfect storm of four market factors resulting from this revolution drives change in the competitive market positioning of every stakeholder organization in the field: ii • PPACA’s limitations on health plan profitability • Consumer and payer search for “value” in health purchases • The shift to value-based reimbursement • The merging roles of care management and service delivery organizationsiii Each of these factors alone presents strategic challenges. Combined, these factors have created a new market environment that demands new management team skills and organizational infrastructure -

Health Sector Advisory Council & Collaborative on Healthcare for Aging Populations and Advanced Illnesses (HSAC/CHAPI)
MEETING SUMMARY May 1-2, 2013 Health Sector Advisory Council & Collaborative on Healthcare for Aging Populations and Advanced Illnesses (HSAC/CHAPI) Health Sector Management, Fuqua School of Business, Duke University “Care Coordination: Data, Dynamics, Dilemmas” was an important update since our April 2011 HSAC meeting in which we discussed the CMS-proposed models/incentives for “accountable care organizations.” Our May 2013 meeting examined several trends we observed since 2011 following several questions: As we have move toward “value-based” payments and greater care coordination, are we appropriately rewarding physician activities that are associated with “quality” from a patient perspective? How are local health care markets being influenced by the convergence of “care coordination” structures, payment reform, and increasing access to clinical and financial data? How are providers and payers positioning themselves in anticipation of the health insurance exchanges? As communities engage in care of the most vulnerable populations, what strategies are being used to control rising Medicaid and Medicare costs? Is greater care coordination inadvertently undermining competitive pressures on prices and quality? Following the agenda from the May meeting are brief summaries of the presentations by our speakers. Biographical sketches and photos of each speaker follows the agenda and summaries. Wednesday, May 1, 2013 Collaborative on Healthcare for Aging Populations and Advanced Illnesses (CHAPI) The World Is Changing Panel Discussion and Presentations David Cannady – Vice President, Strategic Resource Group, HCA Samira Beckwith – CEO Hope Healthcare Services, FL John Barkley – Chief Medical Officer, Post Acute Care Services, Carolinas Healthcare System Tim Clontz -- Executive Vice President, Cone Health System/President, NC PACE Assoc. -

Population Health Management: Meeting the Demand for Value-Based Care POPULATION HEALTH MANAGEMENT: Meeting the Demand for Value-Based Care
National Committee for Quality Assurance in Collaboration with Health Management Associates Population Health Management: Meeting the Demand for Value-Based Care POPULATION HEALTH MANAGEMENT: Meeting the Demand for Value-Based Care OVERVIEW Over the last decade, federal, state and private sector activities have driven population health management and value-based care to the forefront of health care. Public purchasers, such as Medicare and state Medicaid programs, and employers have created incentives for health plans—and increasingly, provider organizations—to contain costs, improve health care quality and meet or exceed population health goals. Other factors, such as changing demographics and the increasing prevalence of chronic disease, are also driving adoption of population health management. Development of a comprehensive population health management strategy is critical to an organization’s ability to drive outcome improvements and succeed under value-based payment models. Organizations must be able to identify the needs of their populations through assessment, risk stratification and development of programs and services that are tailored to those needs. The National Committee for Quality Assurance (NCQA) engaged Health Management Associates (HMA) to summarize the key factors driving population health management adoption among health care organizations, as well as recent population health management trends that are helping organizations succeed under value-based care arrangements. Although this paper is written for leaders of health -

Aligning Health Plans and Providers: Working Together to Control Costs US Health Care Costs Continue to Rise More Rapidly Than Is Sustainable
Aligning health plans and providers: Working together to control costs US health care costs continue to rise more rapidly than is sustainable. Health care spending was $3.2 trillion in 2015, a 5.3% Higher premiums can deter healthy people from voluntarily increase from 2014, and is expected to continue to grow purchasing insurance products, resulting in a higher 5.8% annually for the next decade1. Health care as a average level of “risk” or illness burden in the group that percentage of the US gross domestic product (GDP) has does buy coverage. This creates a “vicious cycle” of even steadily risen from 13.8% in 20002 to 17.8% in 20153, and is higher premiums as the risk deteriorates. The industry predicted to be 20.1% by 20254. should consider focusing on identifying and implementing strategies to bend the medical cost curve while improving While the Affordable Care Act (ACA) improved access to health outcomes. coverage for many Americans5, the recent Presidential election has created uncertainty about the future of Concerns over the cost of care aren’t new. Rapid, but this law. Whether access comes through subsidies on expensive, improvements in technology, the shift from ACA exchanges, expanded Medicaid, or other legislative commercial to government payers while care systems solutions or we return to higher levels of uninsured, health have negative margins on government paid patients care spending per covered person will continue to be a and unaffordability of premium rates, give payers and challenge. How will continued health care cost increases be providers greater incentives to collaborate on population paid for, and how can these increases be dampened? health approaches.