FNB MOCK TEST 2 Answers & Explanations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Netter's Musculoskeletal Flash Cards, 1E
Netter’s Musculoskeletal Flash Cards Jennifer Hart, PA-C, ATC Mark D. Miller, MD University of Virginia This page intentionally left blank Preface In a world dominated by electronics and gadgetry, learning from fl ash cards remains a reassuringly “tried and true” method of building knowledge. They taught us subtraction and multiplication tables when we were young, and here we use them to navigate the basics of musculoskeletal medicine. Netter illustrations are supplemented with clinical, radiographic, and arthroscopic images to review the most common musculoskeletal diseases. These cards provide the user with a steadfast tool for the very best kind of learning—that which is self directed. “Learning is not attained by chance, it must be sought for with ardor and attended to with diligence.” —Abigail Adams (1744–1818) “It’s that moment of dawning comprehension I live for!” —Calvin (Calvin and Hobbes) Jennifer Hart, PA-C, ATC Mark D. Miller, MD Netter’s Musculoskeletal Flash Cards 1600 John F. Kennedy Blvd. Ste 1800 Philadelphia, PA 19103-2899 NETTER’S MUSCULOSKELETAL FLASH CARDS ISBN: 978-1-4160-4630-1 Copyright © 2008 by Saunders, an imprint of Elsevier Inc. All rights reserved. No part of this book may be produced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording or any information storage and retrieval system, without permission in writing from the publishers. Permissions for Netter Art figures may be sought directly from Elsevier’s Health Science Licensing Department in Philadelphia PA, USA: phone 1-800-523-1649, ext. 3276 or (215) 239-3276; or e-mail [email protected]. -

Physical Esxam
Pearls in the Musculoskeletal Exam Frank Caruso MPS, PA-C, EMT-P Skin, Bones, Hearts & Private Parts 2019 Examination Key Points • Area that needs to be examined, gown your patients - well exposed • Understand normal functional anatomy • Observe normal activity • Palpation • Range of Motion • Strength/neuro-vascular assessment • Special Tests General Exam Musculoskeletal Overview Physical Exam Preview Watch Your Patients Walk!! Inspection • Posture – Erectness – Symmetry – Alignment • Skin and subcutaneous tissues – Swelling – Redness – Masses Inspection • Extremities – Size – Deformities – Enlargement – Alignment – Contour – Symmetry Inspection • Muscles – Bilateral symmetry – Hypertrophy – Atrophy – Fasciculations – Spasms Palpation • Palpate bones, joints, and surrounding muscles for the following: – Heat – Tenderness – Swelling – Fluctuation – Crepitus – Resistance to pressure – Muscle tone Muscles • Size and strength affected by the following: – Genetics – Exercise – Nutrition • Muscles move joints through range of motion (ROM). Muscle Strength • Compare bilateral muscles – Strength – Symmetry – Equality – Resistance End Feel Think About It!! • The sensation the examiner feels in the joint as it reaches the end of the range of motion of each passive movement • Bone to bone: This is hard, unyielding – normal would be elbow extension. • Soft–tissue approximation: yielding compression that stops further movement – elbow and knee flexion. End Feel • Tissue stretch: hard – springy type of movement with a slight give – toward the end of range of motion – most common type of normal end feel : knee extension and metacarpophalangeal joint extension. Abnormal End Feel • Muscle spasm: invoked by movement with a sudden dramatic arrest of movement often accompanied by pain - sudden hard – “vibrant twang” • Capsular: Similar to tissue stretch but it does not occur where one would expect – range of motion usually reduced. -

MISSED? Metastatic Spinal Cord Compression NA Quraishi, C Esler ∗ BMJ 342 (7805), 1023-1025
PUBLICATIONS (ABSTRACTS EXCLUDED) 2014: Metastatic spinal cord compression as a result of the unknown primary tumour. Quraishi NA, Ramoutar D, Sureshkumar D, Manoharan SR, Spencer A, Arealis G, Edwards KL, Boszczyk BM. Eur Spine J. 2014 Apr 2. Trans-oral approach for the management of a C2 neuroblastoma. Salem KM, Visser J, Quraishi NA. Eur Spine J. 2014 Feb 19. Calcified giant thoracic disc herniations: considerations and treatment strategies. Quraishi NA, Khurana A, Tsegaye MM, Boszczyk BM, Mehdian SM. Eur Spine J. 2014 Apr;23 Surgical treatment of sacral chordoma: prognostic variables for local recurrence and overall survival. Varga PP, Szövérfi Z, Fisher CG, Boriani S, Gokaslan ZL, Dekutoski MB, Chou D, Qurais NA, Reynolds JJ, Luzzati A, Williams R, Fehlings MG, Germscheid NM, Lazary A, Rhines LD. Eur Spine J. 2014 Dec 23. Expert's comment concerning Grand Rounds case entitled: "trans-oral approach for the management of a C2 neuroblastoma. (K. M. I. Salem, J. Visser, and N. A. Quraishi).Choi D. Eur Spine J. 2015 Jan;24(1):177-9. Diagnosis and treatment of a rectal-cutaneous fistula: a rare complication of coccygectomy. Behrbalk E, Uri O, Maxwell-Armstrong C, Quraishi NA. Eur Spine J. 2014 Nov 1. A cohort study to evaluate cardiovascular risk of selective and nonselective cyclooxygenase inhibitors (COX-Is) in arthritic patients attending orthopedic department of a tertiary care hospital. Bhosale UA, Quraishi N, Yegnanarayan R, Devasthale D. Niger Med J. 2014 Sep;55(5):417-22. An evidence-based medicine model for rare and often neglected neoplastic conditions. Fisher CG, Goldschlager T, Boriani S, Varga PP, Rhines LD, Fehlings MG, Luzzati A, Dekutoski MB, Reynolds JJ, Chou D, Berven SH, Williams RP, Quraishi NA, Bettegowda C, Gokaslan ZL. -

Musculoskeletal Clinical Vignettes a Case Based Text
Leading the world to better health MUSCULOSKELETAL CLINICAL VIGNETTES A CASE BASED TEXT Department of Orthopaedic Surgery, RCSI Department of General Practice, RCSI Department of Rheumatology, Beaumont Hospital O’Byrne J, Downey R, Feeley R, Kelly M, Tiedt L, O’Byrne J, Murphy M, Stuart E, Kearns G. (2019) Musculoskeletal clinical vignettes: a case based text. Dublin, Ireland: RCSI. ISBN: 978-0-9926911-8-9 Image attribution: istock.com/mashuk CC Licence by NC-SA MUSCULOSKELETAL CLINICAL VIGNETTES Incorporating history, examination, investigations and management of commonly presenting musculoskeletal conditions 1131 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey Prof. John O'Byrne Mr. Iain Feeley Dr. Richie Downey Dr. Martin Kelly Mr. Iain Feeley Dr. Lauren Tiedt Dr. Martin Kelly Department of General Practice, RCSI Dr. Lauren Tiedt Dr. Mark Murphy Department of General Practice, RCSI Dr Ellen Stuart Dr. Mark Murphy Department of Rheumatology, Beaumont Hospital Dr Ellen Stuart Dr Grainne Kearns Department of Rheumatology, Beaumont Hospital Dr Grainne Kearns 2 2 Department of Orthopaedic Surgery, RCSI Prof. John O'Byrne Department of Orthopaedic Surgery, RCSI Dr. Richie Downey TABLE OF CONTENTS Prof. John O'Byrne Mr. Iain Feeley Introduction ............................................................. 5 Dr. Richie Downey Dr. Martin Kelly General guidelines for musculoskeletal physical Mr. Iain Feeley examination of all joints .................................................. 6 Dr. Lauren Tiedt Dr. Martin Kelly Upper limb ............................................................. 10 Department of General Practice, RCSI Example of an upper limb joint examination ................. 11 Dr. Lauren Tiedt Shoulder osteoarthritis ................................................. 13 Dr. Mark Murphy Adhesive capsulitis (frozen shoulder) ............................ 16 Department of General Practice, RCSI Dr Ellen Stuart Shoulder rotator cuff pathology ................................... -
CMM-314: Hip Surgery-Arthroscopic and Open Procedures Version 1.0.2019
CLINICAL GUIDELINES CMM-314: Hip Surgery-Arthroscopic and Open Procedures Version 1.0.2019 Clinical guidelines for medical necessity review of speech therapy services. © 2019 eviCore healthcare. All rights reserved. Comprehensive Musculoskeletal Management Guidelines V1.0.2019 CMM-314: Hip Surgery-Arthroscopic and Open Procedures CMM-314.1: Definitions 3 CMM-314.2: General Guidelines 4 CMM-314.3: Indications and Non-Indications 4 CMM-314.4 Experimental, Investigational, or Unproven 6 CMM-314.5: Procedure (CPT®) Codes 7 CMM-314.6: References 10 © 2019 eviCore healthcare. All rights reserved. Page 2 of 13 400 Buckwalter Place Boulevard, Bluffton, SC 29910 • (800) 918-8924 www.eviCore.com Comprehensive Musculoskeletal Management Guidelines V1.0.2019 CMM-314.1: Definitions Femoroacetabular Impingement (FAI) is an anatomical mismatch between the head of the femur and the acetabulum resulting in compression of the labrum or articular cartilage during flexion. The mismatch can arise from subtle morphologic alterations in the anatomy or orientation of the ball-and-socket components (for example, a bony prominence at the head-neck junction or acetabular over-coverage) with articular cartilage damage initially occurring from abutment of the femoral neck against the acetabular rim, typically at the anterosui per or aspect of the acetabulum. Although hip joints can possess the morphologic features of FAI without symptoms, FAI may become pathologic with repetitive movement and/or increased force on the hip joint. High-demand activities may also result in pathologic impingement in hips with normal morphology. s It ha been proposed that impingement with damage to the labrum and/or acetabulum is a causative factor in the development of hip osteoarthritis, and that as many as half of cases currently categorized as primary osteoarthritis may have an etiology of FAI. -

Physicians As Assistants at Surgery: 2016 Update
Physicians as Assistants at Surgery: 2016 Update Participating Organizations: American College of Surgeons American Academy of Ophthalmology American Academy of Orthopaedic Surgeons American Academy of Otolaryngology – Head and Neck Surgery American Association of Neurological Surgeons American Pediatric Surgical Association American Society of Colon and Rectal Surgeons American Society of Plastic Surgeons American Society of Transplant Surgeons American Urological Association Congress of Neurological Surgeons Society for Surgical Oncology Society for Vascular Surgery Society of American Gastrointestinal Endoscopic Surgeons The American College of Obstetricians and Gynecologists The Society of Thoracic Surgeons Physicians as Assistants at Surgery: 2016 Update INTRODUCTION This is the seventh edition of Physicians as Assistants at Surgery, a study first undertaken in 1994 by the American College of Surgeons and other surgical specialty organizations. The study reviews all procedures listed in the “Surgery” section of the 2016 American Medical Association’s Current Procedural Terminology (CPT TM). Each organization was asked to review new codes since 2013 that are applicable to their specialty and determine whether the operation requires the use of a physician as an assistant at surgery: (1) almost always; (2) almost never; or (3) some of the time. The results of this study are presented in the accompanying report, which is in a table format. This table presents information about the need for a physician as an assistant at surgery. Also, please note that an indication that a physician would “almost never” be needed to assist at surgery for some procedures does NOT imply that a physician is never needed. The decision to request that a physician assist at surgery remains the responsibility of the primary surgeon and, when necessary, should be a payable service. -

Orthopaedic Examination Spinal Cord / Nerves
9/6/18 OBJECTIVES: • Identify the gross anatomy of the upper extremities, spine, and lower extremities. • Perform a thorough and accurate orthopaedic ORTHOPAEDIC EXAMINATION examination of the upper extremities, spine, and lower extremities. • Review the presentation of common spine and Angela Pearce, MS, APRN, FNP-C, ONP-C extremity diagnoses. Robert Metzger, DNP, APRN, FNP - BC • Determine appropriate diagnostic tests for common upper extremity, spine, and lower extremity problems REMEMBER THE BASIC PRINCIPLES OF MUSCULOSKELETAL EXAMINATION Comprehensive History Comprehensive Physical Exam THE PRESENTERS • Chief Complaint • Inspection • HPI OLDCART • Palpation HAVE NO CONFLICTS OF INTEREST • PMH • Range of Motion TO REPORT • PSH • Basic principles use a goniometer to assess joint ROM until you can • PFSH safely eyeball it • ROS • Muscle grading • Physical exam one finger point • Sensation to maximum pain • Unusual findings winging and atrophy SPINAL COLUMN SPINAL CORD / NERVES • Spinal cord • Begins at Foramen Magnum and • Consists of the Cervical, Thoracic, continues w/ terminus at Conus Medullaris near L1 and Lumbar regions. • Cauda Equina • Collection of nerves which run from • Specific curves to the spinal column terminus to end of Filum Terminale • Lordosis: Cervical and Lumbar • Nerve Roots • Kyphosis: Thoracic and Sacral • Canal is broader in cervical/ lumbar regions due to large number of nerve roots • Vertebrae are the same throughout, • Branch off the spinal cord higher except for C1 & C2, therefore same than actual exit through -

Abductor Pollicis Brevis 5, 66, 68 Acetabular Dysplasia 199 Achilles
Cambridge University Press 978-0-521-86241-7 - Advanced Examination Techniques in Orthopaedics Edited by Nick Harris Index More information 13Harris(Ind)-cpp 25/9/02 11:34 am Page 219 Index abductor pollicis brevis 5, 66, 68 dislocation 156 acetabular dysplasia 199 paediatric patients 205 achilles tendinitis 165 shoulder instability 99, 101, 207 achilles tendon 167 apprentice’s spine (thoraco-lumbar Scheuermann’s disruption 182 disease) 214 acromegaly 4 arachnodactyly 207 acromioclavicular joint arcade of Frohse 73 impingement signs/tests 96–97 arcade of Struthers 71 inspection 85 arthrogryposis multiplex congenita 191, 206 palpation 85, 88 ataxic gait 197 acromioclavicular joint disorders 81 axillary nerve damage 88, 114, 118 impingement 96, 97 axonotmesis 66 adolescent acetabular dysplasia 193 adolescent disc syndrome 213, 217 back kneeing 197 adolescent idiopathic scoliosis 197 back pain 125, 126 Adson’s manoeuvre 131 paediatric patients 214 Allen’s test 5, 19 ballotment test (Reagan) 35, 36 anconeous epitrochlearis 71 Barlow’s test 203 ankle 165–187 belly press test (Napoleon’s sign) 91, 95 anatomy 170, 173 benign essential tremor 4 examination 167–182 biceps brachii 117 history 165 function testing 92 inspection 167 rupture instability 165, 182 insertion tendon 46, 47 movement 176–179 long head 47, 85 muscle strength grading 206 biceps reflex 88 neurovascular assessment 180 bicipital tendonitis 88, 92 paediatric examination 205–206 biro test see tactile adherence test cerebral palsy 209 block test 199, 200, 201 pain 165 Blount’s -

Physical Examination of Knee Ligament Injuries..Pdf
Review Article Physical Examination of Knee Ligament Injuries Abstract Robert D. Bronstein, MD The knee is one of the most commonly injured joints in the body. Joseph C. Schaffer, MD A thorough history and physical examination of the knee facilitates accurate diagnosis of ligament injury. Several examination techniques for the knee ligaments that were developed before advanced imaging remain as accurate or more accurate than these newer imaging modalities. Proper use of these examination techniques requires an understanding of the anatomy and pathophysiology of knee ligament injuries. Advanced imaging can be used to augment a history and examination when necessary, but should not replace a thorough history and physical examination. he knee joint is one of the most injuries because the current injury may Tcommonly injured joints in the be the sequela of a previous injury. body. Knee ligament injury and sub- Here, we present specific tech- sequent instability can cause consid- niques for the ligamentous exami- erable disability. Diagnosis of knee nation, including identifying injuries ligament injuries requires a thorough of the anterior cruciate ligament understanding of the anatomy and (ACL), the medial collateral liga- the biomechanics of the joint. Many ment (MCL), the lateral collateral specific examination techniques were ligament (LCL), the posterolateral cor- developed before advanced imaging, ner (PLC), and the posterior cruciate and several techniques remain as ligament (PCL), and describe the asso- accurate or more accurate than the ciated anatomy and biomechanics and From the Division of Sports Medicine, new imaging modalities. Advanced the methods that allow for increased Department of Orthopaedics, University of Rochester School of Medicine and imaging (eg, MRI) is appropriate to diagnostic sensitivity and accuracy. -

Elbow, Forearm, Wrist & Hand
Orthopedic Physical Assessment with Special Tests | Elbow, Forearm, Wrist & Hand COURSE DESCRIPTION Detailed video demonstrations of tests and procedures common in musculoskeletal assessment are supplemented by high-quality full-color clinical photographs and illustrations of each test and assessment for the Elbow, Forearm, Wrist & Hand. LEARNING OBJECTIVES Module 1 | Selected Movements- Elbow At the end of this module the learner will be able to: • Correctly instruct patients in performing active movements of the elbow including flexion,extension, pronation, and supination. • Identify positive indications of flexion, extension, pronation, and supination of the elbow. • Correctly perform and identify positive indications of passive movements of the elbow. • Correctly perform and identify positive indications of resisted isometric movements of the elbow including elbow flexion, elbow extension, pronation, supination, wrist flexion, and wrist extension. Module 2 | Special Tests for Ligamentous Instability At the end of this module the learner will be able to: • Define and describe ligamentous instability including suspected injury, epidemiology and demographics, relevant history, and relevant signs, symptoms and mechanism of injury for dislocation/subluxation and repetitive stress injuries. • Correctly perform and identify positive indications of a ligamentous valgus instability test. • Correctly perform and identify positive indications of a ligamentous varus instability test. • Correctly perform and identify positive indications of a milking maneuver. • Correctly perform and identify positive indications of a moving valgus stress test. • Correctly perform and identify positive indications of a lateral pivot-shift test. • Correctly perform and identify positive indications of a posterolateral rotary drawer test. • Correctly perform and identify positive indications of a posterolateral rotary apprehension test. Page 1 of 4 Accelerated Online Learning Orthopedic Phys. -
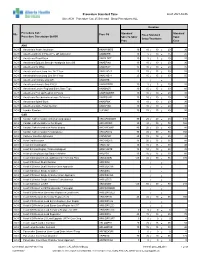
Standard Times Report
Procedure Standard Time as of: 2021-04-06 Site: ACH Procedure Cat: 25 Selected Show Procedures: ALL Duration Procedure Cat / Standard Standard Site Proc Cd Fixed Standard Procedure Description Std BK Skin To Skin/ Total Setup/Teardown Proc Case ANA ACH Anesthesia Awake Intubation ANAWKINTB 10 10 / 10 = 20 30 ACH Anesthesia Block in PACU Pre OR Admission ANABKRR 10 5 / 10 = 15 25 ACH Anesthesia Blood Patch ANABLDPT 10 5 / 5 = 10 20 ACH Anesthesia Epidural Steroid+/-Analgesia Inject SS ANAEPINJ 10 10 / 10 = 20 30 ACH Anesthesia for XRay ANAXRAY 15 10 / 10 = 20 35 ACH Anesthesia Insert Long Line IV<1 Year ANALINE<1 25 15 / 15 = 30 55 ACH Anesthesia Insert Long Line IV>1 Year ANALINE>1 25 15 / 15 = 30 55 ACH Anesthesia Intubate Only OR ANAINTB / = ACH Anesthesia Intubate Only PACU ANAINTBRR 10 5 / 5 = 10 20 ACH Anesthesia Local+/-Regional Block State Type ANABKOR 30 15 / 15 = 30 60 ACH Anesthesia Post Op Readmit to PACU ANARADMRR 10 10 / 10 = 20 30 ACH Anesthesia Pseudocholinesterase Deficiency ANAPSURR 10 10 / 10 = 20 30 ACH Anesthesia Spinal Block ANASPBK 10 10 / 10 = 20 30 ACH Anesthesia Spine Facet Injection ANASPINJ 10 10 / 10 = 20 30 ACH Lumbar Puncture LUPUNC 10 25 / 15 = 40 50 CAR ACH Cardiac Catheterization & Balloon Angioplasty HRCARCBANG 90 20 / 20 = 40 130 ACH Cardiac Catheterization w Full Biopsy HRCARCBX 90 40 / 30 = 70 160 ACH Cardiac Catheterization w Partial Biopsy HRCARCBXP 40 20 / 20 = 40 80 ACH Cardiac Catheterization+/-Valvoplasty HRCARCVL 90 40 / 30 = 70 160 ACH Catheter Insertion Aphoresis CAINAPHP 20 15 / 10 = 25 45 -

The Rules of Four: a Systematic Approach to Diagnosing Common Musculoskeletal Conditions of the Knee
Lerew S, Stoker S, Nallamothu S. The Rules of Four: A Systematic Approach to Diagnosing Common Musculoskeletal Conditions of the Knee. SMRJ. 2020;4(2). doi:10.51894/001c.11765 Clinical Practice The Rules of Four: A Systematic Approach to Diagnosing Common Musculoskeletal Conditions of the Knee a Shawn Lerew, DO 1 , Steven Stoker, DO 1, Shivajee Nallamothu, DO 1 1 Orthopedic Surgery, McLaren Oakland Hospital Keywords: knee, physical exam, musculoskeletal https://doi.org/10.51894/001c.11765 Spartan Medical Research Journal Vol. 4, Issue 2, 2020 Musculoskeletal symptoms are consistently one of the most commonly cited reasons for visits to ambulatory care centers every year, with knee pain accounting for approximately one-third of the reported complaints. Previous studies have demonstrated that many non-orthopedic physicians report a lack of confidence in performing clinical musculoskeletal knee examinations. “The Rules of Four” approach presented in this paper is designed to present a systematic and concise method to musculoskeletal examination of the knee within a memorable format. The approach allows for the timely diagnosis of common musculoskeletal injuries while aiding in directing further treatment and diagnostic testing. This method will ideally allow medical students and non-orthopedic physicians alike to confidently and effectively evaluate patients with complaints of knee pain in ambulatory care settings. INTRODUCTION With this approach, the knee is divided into three columns each with four corresponding examination points th Musculoskeletal symptoms are consistently one of the most and a 4 “column” comprised of the four main ligaments commonly cited reasons for visits to primary care providers of the knee.