Who Uses Nhs Direct? Factors That Impact on the Uptake of Telephone Based Healthcare
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

GWF Annual Report 2020
Annual Report Report and accounts of the Trustees · 2020 Nunc a mauris. Proin eget ligula. Nam cursus libero. Vestibulum velit orci, bibendum eget, molestie eu, sagittis non, leo. Nullam sed enim. Duis ac lorem. Lorem ipsum dolor sit amet, consectetuer adipiscingAnnual elit. Suspendisse Report potenti. Sed tincidunt varius arcu. Mauris vitae arcu sit amet quam condimentum pulvinar. Aenean Report and accounts of the Trustees Financial year to 5 April 2020 Reference and administrative information The Garfield Weston Foundation is a general grant-giving charity endowed by the late W Garfield Weston and members of his family, which is registered with the Central Register of Charities, registration number 230260. The Foundation is recognised by the Inland Revenue as an approved charity for tax purposes, the reference number being X96978. Principal Office Weston Centre 10 Grosvenor Street London W1K 4QY Trustees Guy H Weston, Chairman Anna Catrina Hobhouse Jana R Khayat Sophia M Weston Eliza L Mitchell Melissa Murdoch George G Weston Alannah Weston Geordie Dalglish Director Philippa Charles Secretary to the Trustees Janette Cattell Bankers Nunc a mauris.Coutts Proin & Co eget ligula. Nam cursus libero. 440 Strand Vestibulum velitLondon orci, WC2R bibendum 0QS eget, molestie eu, sagittis non, leo. Nullam sed enim. Duis ac lorem. Lorem ipsum dolor sit amet, Solicitors consectetuer adipiscingSlaughter and elit. May Suspendisse potenti. Sed tincidunt varius arcu. Mauris vitae1 Bunhill arcu Row sit amet quam condimentum pulvinar. Aenean London EC1Y -

A Geographical History of Hester's
AA GGEEOOGGRRAAPPHHIICCAALL HHIISSTTOORRYY OOFF HHEESSTTEERR’’SS WWAAYY Updated JULY 2015 COPYRIGHT INFORMATION: Produced by DAVID EDGAR. All of my researches here may be freely used or adapted by anybody else - no acknowledgements necessary - but please note that strictly speaking this does not apply to the late Mrs Hyett’s interviews, nor to newspaper quotes, nor to unacknowledged photographs. Readers, please send comments to [email protected]. Picture: aerial view of the new GCHQ under construction c.2001. OVERALL INTRODUCTION This is a history project that’s got a bit out of hand. My own interests are geographical, especially the interpretation of maps. And also to some extent archaeological, the things that left a mark. I find it hard to get excited about ancient things unless they have left a visible mark on the modern-day landscape. Apart from my own interpretation of maps, I have brought together the scraps of lore to be found in other peoples’ works. Douglas Trapp’s “History of Arle” produced for Dowty in 1971 was the last attempt to cover the early history. Phyllis White had set herself the task of updating that text, but her researches and those of Mrs Margery Hyett were barely touched in the five volumes Hester’s Way Neighbourhood Project finally produced commencing in March 1999, The History of Hester’s Way. I should here give credit to those two individuals - and also Sheila Forrest, Aylwin Sampson and others who attended our Local History Group – for some incidental facts that I jotted down then and have included here. It’s very easy to let one document lead to another, and there seems an infinity of material available for research. -

Your MCF Briefing November 2019
Your MCF briefing November 2019 Chief Executive and Chief Operating Officer • Following the results from the second staff survey, three sessions were held in early October to explore the feedback and identify ways of improving working practices and staff support. This process continued with a successful Staff Forum held in November and a number of proposals are now being implemented. • The remaining MCF summer holidays concluded with gala dinners in Eastbourne and Westcliffe-on-Sea. Once again, both were well attended and enjoyed by all. • The 2025 Dorset Festival Appeal was launched at Sherborne School in September. In the same month, West Kent held a pre-launch for their 2026 Festival at an event attended by over 100 charity stewards. The formal launch will be held at a black tie event on 7 February 2020. • At the end of October, Suffolk and Shropshire’s festivals both concluded with successful and enjoyable events. The 2019 Shropshire Festival Appeal returned the second-highest per capita total on record. • Also in October, the biannual Charity Stewards’ Conference was held in Nottingham. Almost all provinces were represented and the conference was one of the most successful held to date. • An impressive Vision Document outlining proposals for Compass Park was presented to Hertsmere Borough Council Planning Panel at the end of October. This appears to have been well received and further discussions are ongoing. • Arrangements for the 2020 MCF Ball have now been finalised and it will be held at the Chelsea Harbour Hotel on Saturday 20 June. Guest cabaret will be the legendary Status Quo. -

Annual Report and Financial Statements
Annual Report and Financial Statements For the year ending 31st March 2020 ANNUAL REPORT Registered Office And Official Address Bernard Sunley Foundation 20 Berkeley Square London W1J 6LH Board Of Trustees And Directors Mrs Anabel Knight (Chairman) Mrs Joan Tice DL, OBE (deceased 26th April 2019) Mrs Bella Sunley MBE Dr Brian W Martin Mr William Tice FRCS Mr Inigo Paternina Mrs Lucy Evans Director Ms Sue Davies Auditors Bankers Haysmacintyre LLP Clydesdale Bank 10 Queen Street Place 154-158 Kensington High Street London EC4R 1AG London W8 7RL Investment Managers Barwood Capital CCLA Investment Management FF&P Private Equity Limited 4 Waterside Way Limited 8 Sackville Street The Lakes Senator House London W1S 3EZ Bedford Road 85 Queen Victoria Street Northampton NN4 7XD London EC4V 4ET Fundsmith LLP 33 Cavendish Square Blackrock Advisors (UK) Limited Charles Stanley Pan Asset Capital Marylebone 12 Throgmorton Avenue Management Limited London W1G 0PW London EC2N 2DL Bishopsgate 55 Bishopsgate Mayfair Capital Investment London EC2N 3AS Management Limited 55 Wells Street London W1T 3PT 2 ANNUAL REPORT Contents Annual Report 4 Structure, Governance and Management 5 Objectives and Activities 6 Achievements and Performance 9 Investments and Financial Review 11 Statement of Trustees’ Responsibilities 12 Independent Auditor’s Report to the Trustees of the Bernard Sunley Foundation 15 Charities funded above £5,000 19 Charities funded at £5,000 and less 24 Grant payments made Financial Statements 28 Statement of Financial Activities 29 Balance Sheet 30 Cash Flow Statement 31 Accounting Policies 33 Notes to Financial Statements Bernard Sunley Foundation 3 ANNUAL REPORT Structure, Governance and Management The Bernard Sunley Foundation was founded on 28th July 1960 by the late Bernard Sunley (1910–1964) as a general grant making charity registered in England and Wales (number 1109099). -

Region Lieutenancy Group Name East Midlands Derbyshire Derbyshire Childrens Holiday Centre East Midlands Derbyshire PADLEY GROUP
Region Lieutenancy Group name East Midlands Derbyshire Derbyshire Childrens Holiday Centre East Midlands Derbyshire PADLEY GROUP East Midlands Leicestershire TwentyTwenty East Midlands Lincolnshire GRIMSBY, CLEETHORPES AND DISTRICT DIAL-A-RIDE East Midlands Nottinghamshire Age UK Nottingham & Nottinghamshire East Midlands Nottinghamshire DUKES WOOD OIL MUSEUM East Midlands Nottinghamshire Indigo Kids East Midlands Nottinghamshire Nottingham Child Contact Centre East of England Bedfordshire Bedford and District Handicapped Riders Association East of England Bedfordshire The Airfield Volunteer Fire Service The Forest of Marston Vale Volunteers (Forest East of England Bedfordshire Volunteers) East of England Cambridgeshire LadyBird Trsut East of England Cambridgeshire The Hometown Rock and Roll Band East of England Suffolk Hospice Neighbours Islands Guernsey Alderney Cancer Relief Trust Islands Guernsey The Priaulx Premature Baby Foundation Islands Jersey Age Concern Jersey North East County Durham Durham Pointers North East Northumberland Berwick Detachment, Northumbria Army Cadet Force North East Northumberland Phoenix Theatre North East Northumberland Tynedale Hospice at Home North East Tyne and Wear Cancer Connections North East Tyne and Wear Cornerstone North East Tyne and Wear Rape Crisis Tyneside and Northumberland (RCTN) North East Tyne and Wear Royalty Theatre Sunderland North West Cheshire Chelford Tenants and Residents Association North West Cheshire Cre8 North West Cheshire Northern Lights Children's Charity North West Greater -

Unlocked Book PDF Feb 2014
Hidden stories of the lives of Birmingham women 1900 to the present day Gudrun Limbrick BA Hons Oxon MA B’ham Contents Foreword by The Rt Hon Clare Short ....................................... 3 Action .............................................................................. 31 Introduction ...................................................................................... 4 Badrun Pasha: Working in the community ........................ 32 About the project ............................................................................. 5 Taslima Akbar: A political time .............................................. 34 Themes ............................................................................................... 6 Theresa Stewart: Our first female Council Leader .......... 36 Diversity .......................................................................... 38 Creativity .......................................................................... 7 Joycelyn Faulkner: Growing up in Handsworth ................ 39 Birmingham women in public art ................................................ 8 Emma Tucker: An upbringing that wasn’t the ‘norm’ .... 41 Doreen Goodall: Working at Cadbury’s ................................. 9 Anne Farag: A very Brummie trade ....................................... 11 Equality ........................................................................... 43 Women in Birmingham politics ................................................ 44 Independence ................................................................ -
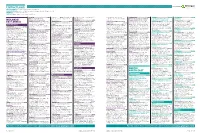
Contract Leads 270415
Contract Leads Powered by EARLY PLANNING Projects in planning up to detailed plans submitted. PLANS APPROVED Projects where the detailed plans have been approved but are still at pre-tender stage. TENDERS Projects that are at the tender stage CONTRACTS Approved projects at main contract awarded stage. IPSWICH £1M Developments Plc Agent: CMYK Planning & Drive, Sherwood Park, Nottingham, NG15 0DT Volker Fitzpatrick, Hertford Road, SHERINGHAM £1M GRIMSBY £1.515M CASTLEFORD £0.9M Hanson Concrete Products, Design, 6 Gavel Centre, St Albans,, AL3 6PQ Tel: 0115 906 1268 Hoddesdon, Hertfordshire, EN11 9BX Tel: 1 Blowlands Lane Upper Sheringham Rear Of Paragon House, Kiln Lane Savile Road MIDLANDS/ Sproughton Road Sproughton Tel: 01727 830123 NORWICH £6M 01992 305000 Planning authority: North Norfolk Job: Trading Estate Stallingborough Planning authority: Wakefield Job: Detail Planning authority: Babergh Job: Detailed PETERBOROUGH £1.9M Lotus Test Track, Potash Lane Hethel Clay Farm Development, Long Road Reserved Matters Granted for 8 residential Planning authority: North East Lincolnshire Plans Granted for 12 houses Client: EAST ANGLIA Plans Submitted for 12 industrial units Client: Prince William School, Herne Road Planning authority: South Norfolk Job: Trumpington £8.5m units Client: Broadland Housing Association Job: Detailed Plans Submitted for storage Greenhaven Homes Phase 1 Plc Developer: Brisko Metal Resources Agent: A I Oundle Detail Plans Granted for 3 wind turbines Planning authority: Cambridge Job: Detail Agent: Richard Pike Associates, -

Annual Report 2017
ALLCHURCHES TRUST LIMITED 2017 STRATEGIC REPORT WITH SUPPLEMENTARY MATERIAL As the owner of an ethical and successful financial services group, our vision is to deliver steadily growing support to churches and other charities, for the greater good of all. Allchurches Trust Limited Table of Contents Page Contents 3 About us 4 Explanation of terms 5 Reference and administrative details 6 Chairman’s Report 10 Strategic Report 40 Trustees’ Report 47 Charity statement of financial activities (including an income and expenditure account) 48 Charity balance sheet 49 Charity statement of cash flows 50 Consolidated statement of financial activities (including an income and expenditure account) 52 Consolidated balance sheet 53 Charitable giving (unaudited) This strategic report with supplementary information is only part of the Allchurches Trust Limited 2017 Annual Report, which is the charity’s full annual report and accounts. It does not contain sufficient information to allow for as full an understanding of the results of Allchurches Trust Limited and its trading subsidiaries and the state of affairs of the charity as would be provided by the full annual report and accounts. Notes to the charity and consolidated financial statements are not included in this statement but, where referred, are presented in the full annual report and accounts. The auditor’s report on the full annual report and accounts was unqualified. The auditor’s statement relating to the consistency of the trustees’ annual report and strategic report with the accounts was unqualified. For further information copies of the full annual accounts can be obtained, free of charge, from the company secretary at the registered office on page 5 of this statement. -

Agenda Papers
TRUST BOARD MEETING IN PUBLIC Wednesday 30 October 2019 At 09:30 VENUE: Oasis Centre, Queen Alexandra Hospital COSHAM Page 1 of 131 Page 2 of 131 TRUST BOARD MEETING IN PUBLIC Wednesday 30th October 2019 09:30 – 14.45 Oasis Centre, Queen Alexandra Hospital, Southwick Hill Road, Cosham, Portsmouth, PO6 3LY A G E N D A Item Time Item Enclosure Presented No. Y/N & by Number 228.19 09.30 Welcome, Apologies and Declaration of N Chair Interests (to ascertain whether any Board Member has any conflict of interest with any items on the Agenda) Divisional Presentation – Medicine and 229.19 09.35 N Urgent Care Minutes of the last meeting – 25th 230.19 10.00 1 Chair September 2019 231.19 10.05 Matters Arising/Summary of agreed actions 2 Chair 232.19 10.10 Notification of any other business N/A Chair 233.19 10.15 Chair’s opening remarks N/A Chair 234.19 10.25 Chief Executive’s Report 3 CEO STRATEGY 235.19 10.45 Winter Planning N COO 236.19 11.15 Compassionate Care 4 CN QUALITY AND SAFETY Quality and Performance Committee Committee 237.19 11.35 5 feedback Chair Safety, quality and operational performance MD / COO 238.19 11.45 N** report analysis / CN 239.19 12.45 Annual Complaints Report 6 DGR Emergency Preparedness, Response and 240.19 12.55 7 COO Resilience – Annual Report Page 3 of 131 WORKFORCE AND ORGANISATIONAL DEVELOPMENT Workforce and Organisational Development Committee feedback Committee 241.19 13.05 8 th Chair 19 September 2019 (for information) 23rd October 2019 (verbal) Workforce and Organisational Development 242.19 13.15 N** DWOD performance -

Annual Report and Financial Statements
OASIS COMMUNITY LEARNING (A Company Limited by Guarantee) ANNUAL REPORT AND FINANCIAL STATEMENTS YEAR ENDED 31 AUGUST 2020 Company Number: 05398529 ANNUAL REPORT AND FINANCIAL STATEMENTS YEAR ENDED 31 AUGUST 2020 ANNUAL REPORT AND FINANCIAL STATEMENTS YEAR ENDED 31 AUGUST 2020 REFERENCE AND ADMINISTRATIVE DETAILS MEMBERS Oasis Charitable Trust (Company number: 02818823) is the sole Member DIRECTORS Nick Bent Andy Blundell (3) Craig Dean Keith Dennis (1) (2) (3) Ann Holt Contents Page Alison Layne-Smith (appointed 13 February 2020) Tony Lowman (1) (2) Graham Mungeam (1) (2) Dave Rasmussen (1) (2) (appointed 6 January 2020) Reference and Administration Information 1 Nita Rogers (3) Andy Simmonds (1) (2) Report of the Directors 2 John Whiter (1) (2) (resigned 25 March 2020) (1) Members of the Audit & Risk Committee Governance Statement 23 (2) Members of the Finance Committee Statement on Regularity, Propriety and Compliance 29 (3) Members of the Performance Evaluation Committee Statement of Directors’ Responsibilities 30 The Directors are also the trustees of Oasis Community Learning under charity law. Independent Auditor’s Report on the Financial Statements 31 COMPANY SECRETARY John Barneby Reporting Accountant’s Report on Regularity 34 EXECUTIVE GROUP Chief Executive Officer John Murphy Statement of Financial Activities 36 Director of People Joy Madeiros National Director of Secondary Philip Beaumont Balance Sheet 37 National Director of Primary Chris Chamberlain Cash Flow Statement 38 Chief Operating Officer & Accounting Officer John Barneby