ORTHOPAEDIC SURGERY) 2 | P a G E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

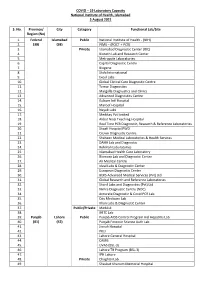
19 Laboratory Capacity National Institute of Health, Islamabad 16 July 2021
COVID – 19 Laboratory Capacity National Institute of Health, Islamabad 16 July 2021 S. No. Province/ City Category Functional Lab/Site Region (No) 1. Federal Islamabad Public National Institute of Health - (NIH) 2. (37) (37) PIMS – (POCT + PCR) 3. Private Islamabad Diagnostic Center (IDC) 4. Biotech Lab and Research Center 5. Metropole Laboratories 6. Capital Diagnostic Centre 7. Biogene 8. Shifa International 9. Excel Labs 10. Global Clinical Care Diagnostic Centre 11. Temar Diagnostics 12. Margalla Diagnostics and Clinics 13. Advanced Diagnostics Centre 14. Kulsum Intl Hospital 15. Maroof Hospital 16. Nayab Labs 17. Medikay Pvt limited 18. Akbar Niazi Teaching Hospital 19. Real Time PCR Diagnostic, Research & Reference Laboratories 20. Shaafi Hospital PWD 21. Crown Diagnostic Centre 22. Shaheen Medical Laboratories & Health Services 23. DAHA Lab and Diagnostic 24. Rehman Laboratories 25. Islamabad Health Care Laboratory 26. Biomaxx Lab and Diagnostic Centre 27. Ali Medical Centre 28. Ideal Labs & Diagnostic Center 29. European Diagnostic Center 30. BEKS Advanced Medical Services (Pvt) Ltd 31. Global Research and Reference Laboratories 32. Sharif Labs and Diagnostics (Pvt) Ltd 33. Nimra Diagnostic Centre (NDC) 34. Accurate Diagnostic & Covid PCR Lab 35. City Medicare Lab 36. Public/Private MedAsk 37. IHITC Lab 38. Punjab Lahore Public Punjab AIDS Control Program incl Hepatitis Lab 39. (79) (40) Punjab Forensic Science Auth Lab 40. Jinnah Hospital 41. PKLI 42. Lahore General Hospital 43. CAMB 44. UVAS (BSL-3) 45. Lahore TB Program (BSL-3) 46. IPH Lahore 47. Private Chughtai Lab 48. Shaukat Khanum Memorial Hospital 49. Islamabad Diagnostic Center (IDC) 50. Rahila Research and Reference Lab 51. -

FPSC - JULY2021 Sr
FPSC - JULY2021 Sr. Sepecility Hospital Seats Punjab 1Anaesthesia Allied Hospital, Faisalabad 2 2Anaesthesia Benazir Bhutto Hospital, Rawalpindi 1 3Anaesthesia Choudhary Prevez Ilahi Institute of Cardiology , Multan 4 4Anaesthesia DHQ Hospital, Faisalabad 2 5Anaesthesia Holy Family Hospital, Rawalpindi 1 6Anaesthesia Lahore General Hospital, Lahore 5 7Anaesthesia Mayo Hospital, Lahore 9 8Anaesthesia Nishtar Hospital, Multan 5 9Anaesthesia Punjab Institute of Cardiology, Lahore 1 10Anaesthesia Sir Ganga Ram Hospital, Lahore 3 11Anaesthesia SZ Hospital, Rahim Yar Khan 2 12Biochemistry Mayo Hospital, Lahore 1 13 Cardiac Surgery Choudhary Prevez Ilahi Institute of Cardiology , Multan 2 14Cardiac Surgery Faisalabad Institute of Cardiology 2 15Cardiac Surgery Mayo Hospital, Lahore 1 16Cardiac Surgery Punjab Institute of Cardiology, Lahore 3 17Cardiac Surgery SZ Hospital, Rahim Yar Khan 1 18Cardiology Choudhary Prevez Ilahi Institute of Cardiology , Multan 4 19Cardiology Faisalabad Institute of Cardiology 3 20Cardiology Mayo Hospital, Lahore 2 21Cardiology Nishtar Hospital, Multan 1 22Cardiology Punjab Institute of Cardiology, Lahore 7 23Cardiology SZ Hospital, Rahim Yar Khan 2 24Chemical Pathology Nishtar Hospital, Multan 1 25Chemical Pathology SZ Hospital, Rahim Yar Khan 1 26Community Medicine Mayo Hospital, Lahore 2 27Community Medicine Nishtar Hospital, Multan 2 28Community Medicine RMU Allied Hospital, Rawalpindi 2 29Community Medicine SZ Hospital, Rahim Yar Khan 3 30Dermatology Benazir Bhutto Hospital, Rawalpindi 1 31Dermatology DHQ Hospital, -

MD - JULY2021 Sr
MD - JULY2021 Sr. Sepecility Hospital Seats Punjab 1Cardiology Benazir Bhutto Hospital, Rawalpindi 1 2Cardiology Bahawal Victoria Hospital, Bahawalpur 3 3Cardiology Choudhary Prevez Ilahi Institute of Cardiology , Multan 4 4Cardiology Faisalabad Institute of Cardiology 3 5Cardiology Mayo Hospital, Lahore 2 6Cardiology Nishtar Hospital, Multan 1 7Cardiology Punjab Institute of Cardiology, Lahore 7 8Dermatology Benazir Bhutto Hospital, Rawalpindi 1 9Dermatology Bahawal Victoria Hospital, Bahawalpur 1 10Dermatology DHQ Hospital, Faisalabad 1 11Dermatology Lahore General Hospital, Lahore 1 12Dermatology Mayo Hospital, Lahore 2 13Dermatology Sir Ganga Ram Hospital, Lahore 1 14Diagnostic Radiology Benazir Bhutto Hospital, Rawalpindi 1 15 Diagnostic Radiology Choudhary Prevez Ilahi Institute of Cardiology , Multan 1 16Diagnostic Radiology Holy Family Hospital, Rawalpindi 1 17Diagnostic Radiology Lahore General Hospital, Lahore 4 18Diagnostic Radiology Mayo Hospital, Lahore 2 19Diagnostic Radiology Sir Ganga Ram Hospital, Lahore 1 20Diagnostic Radiology Punjab Institute of Neurosciences, Lahore 1 21Emergency Medicine Holy Family Hospital, Rawalpindi 1 22Gastroenterology Holy Family Hospital, Rawalpindi 1 23Gastroenterology Govt. Teaching Hospital GM Abad, Faisalabad 1 24Gastroenterology Lahore General Hospital, Lahore 1 25Gastroenterology Mayo Hospital, Lahore 1 26Medical Oncology Jinnah Hospital, Lahore 1 27Medical Oncology Mayo Hospital, Lahore 1 28Medicine Mayo Hospital, Lahore 6 29Medicine Allied Hospital, Faisalabad 4 30Medicine Benazir -

List of Hospitals Province-Wise with Isolation Facilities
LIST OF HOSPITALS PROVINCE-WISE WITH ISOLATION FACILITIES Sr Districts Hospitals Beds Islamabad 1. Islamabad Pakistan Institute of Medical Sciences (PIMS) 10 TOTAL 1 (Medical Facility) 10 Balochistan Sr Districts Hospitals Beds 1. BHU Dalbandin 4 2. Chaghi DHQ Hospital Dalbandin 10 3. Pakistan House, Taftan 9 4. Panjgur DHQ Hospital Panjgur 12 5. Kech DHQ Hospital Kech 10 6. Gwadar GDA Hospital 10 7. Washuk DHQ Hospital Washuk 5 8. Chaman DHQ Hospital Chaman 10 9. Killa Abdullah DHQ Hospital Killa Abdullah 14 10. Killa Saifullah DHQ Hospital Killa Saifullah 15 11. Zhob DHQ Hospital and BHU Qamardin Karez 5 12. Sheikh Khalifa Bin Zayed Hospital 225 Quetta 13. Fatima Jinnah General and Chest Hospital 200 14. Lasbella DHQ Hospital Lasbella 5 TOTAL 14 (Medical Facilities) 534 Khyber Pakhtunkhwa Sr Districts Hospitals Beds 1. DHQ Hospital Abbottabad 15 2. Ayub Teaching Hospital 24 3. Abbottabad Medical Complex 10 4. Gillani Hospital 5 5. Cat-D Hospital Havellian 5 Abbottabad 6. Cat-D Hospital Lora 5 7. Cat-D Hospital Boi 5 8. Nathiagali 4 9. Khairagali 5 10. Sherwan 3 11. Bajaur DHQ Hospital Khar 8 12. DHQ Hospital Bannu 10 13. KGN Hospital Bannu 6 14. Type-D Hospital Kakki 4 15. Bannu Type-D Hospital Janni Khel 4 16. RHC Domel 3 17. RHC Ghori Wala 8 18. DHQ Hospital Battagram 10 19. Type-D Hospital Banna 5 20. Battagram RHC Thakot 4 21. Kozabanda 12 22. Buner DHQ Hospital Buner 4 23. DHQ Hospital Charsadda 5 24. THQ Hospital Shabqadar 2 Charsadda 25. THQ Hospital Tangi 4 26. -

Screening Mammography; Anxiety and Pain Associated, an Experience at Benazir Bhutto Hospital
The Professional Medical Journal www.theprofesional.com ORIGINAL PROF-2338 SCREENING MAMMOGRAPHY; ANXIETY AND PAIN ASSOCIATED, AN EXPERIENCE AT BENAZIR BHUTTO HOSPITAL. Dr. Shafia Naeem1, Dr. Faisal Mahmood2, Dr. Ali Qamar3, Dr. Umer Liaqat4, Dr. Ayesha Anwar5, Dr. Muhammad Imran Aftab6, Dr. Farkhanda Abbassi7 1. MBBS, PGT Radiology, Benazir Bhutto Hospital, Rawalpindi ABSTRACT…Background: Worry about risk for breast cancer and pain are associated with 2. MBBS, PGT Radiology, Holy Family Hospital, Rawalpindi mammography use. Both have been found to be a barrier to mammography use by women. 3. MBBS, PGT Radiology, Objective: To examine the anxiety and pain associated with mammography use in a sample of Benazir Bhutto Hospital, Rawalpindi 4. MBBS, PGT Orthopeadics/Medical Officer, women stratified according to breast cancer risk. Design: This prospective observational study. Benazir Bhutto Hospital, Rawalpindi Setting: Department of Obstetric and Gynecology, Benazir Bhutto Hospital. Period: August 5. MBBS, Pathology Dept., Benazir Bhutto Hospital, Rawalpindi 2011 to June 2012. Patients & Methods: Women awaiting screening mammography in the 6. Senior Demonstrator, Physiology Dept., reception area were asked to complete a questionnaire containing demographics for calculation Independent Medical College, Faisalabad. 7. MBBS, MCPS, FCPS Radiology, of breast cancer risk and the Likert scale for anxiety before the procedure and VAS for Benazir Bhutto Hospital, Rawalpindi assessment of pain after the procedure. Results: Our study included 100 women undergoing screening mammography with an average age of 53.9±8.8 years. 15% were classified “higher risk” by the Gail model. The average anxiety level was 4.03±1.3 on Likert scale and average pain Correspondence Address: during the procedure was 3.3±2.18 on VAS. -

Frequency and Associated Factors for Postnatal Depression Ather Muneer1, Fareed Aslam Minhas1, Asad Tamiz-Ud-Din Nizami1, Faiza Mujeeb1 and Asma Tanvir Usmani2
ORIGINAL ARTICLE Frequency and Associated Factors for Postnatal Depression Ather Muneer1, Fareed Aslam Minhas1, Asad Tamiz-ud-Din Nizami1, Faiza Mujeeb1 and Asma Tanvir Usmani2 ABSTRACT Objective: To determine the frequency and associated sociodemographic, obstetric and medical factors for postnatal depression in an outpatient sample. Study Design: A descriptive, cross-sectional study. Place and Duration of Study: Department of Obstetrics and Gynaecology, Benazir Bhutto Hospital (formerly Rawalpindi General Hospital), Rawalpindi, between June 2006 and February 2007. Methodology: The sample consisted of women who were in the puerperal period (6 weeks postpartum). They were screened with the help of Edinburgh Postnatal Depression Scale (Urdu version) and the severity of depression was rated with the Hamilton Rating Scale for Depression. Results: A total of 51 participants, or 33.1% of a sample of 154 women suffered from postnatal depression, the majority of whom were either moderately or severely depressed. The demographic profile of depressed patients showed that they were young (mean age around 25 years), had a low level of education (below the matriculate level) and came from the lower socioeconomic class. They had small families comprising of fewer than 3 children, were married for less than 5 years and the majority were from extended families (living with in-laws). Conclusion: Postnatal depression was found in almost 1/3rd of the study participants and the pre-ponderance of them suffered from moderate or severe depression. They were young and came from a background of socio-economic adversity. Since postnatal depression had adverse consequences for the mother and her newborn baby, there was an urgent need to direct more attention to this problem, in particular towards its early detection, so that morbidity could be reduced in this group of women. -

Governor Punjab
Governor Punjab Chaudhry Muhammad Sarwar Chancellor of Rawalpindi Medical University 1 Messages Prof. Dr. Yasmin Rashid Health Minister Punjab I am extremely pleased to hear about 4th RMU International Scientific Conference. It is endeavor of Government to ensure equitable health facilities for every part of society. Holding such events will help to upgrade existing facilities and bring new knowledge regarding patient management. It is indeed a noble gesture of the health community working nationally and abroad to come forward and help their countrymen. I extend my full cooperation to Prof. Muhammad Umar and Organizing Committee, on behalf of Government of Punjab, in holding such an important event and wish RMU faculty every Success. Prof. Muhammad Umar Vice Chancellor RMU It is my immense pleasure to invite you and accompany us at 4 th International Scientific Conference going to be held from 20th-23rd March 2019. Being the Rawalian graduate and now proudly first Rawalian VC, this was may ambition to hold such an endeavor of international standard which aimed to apprise, nurture and globalize mastery technological innovation, knowledge and research of medicine which help the young Rawalians to make an early debut on international stage. I hope this conference will be the landmark to implement our mission as university. I wish great success to conference. Prof. Muhammad Ajmal Chairperson It is indeed an occasion of great pride and pleasure for the organizing committee to host 4th International Rawalpindi Medical University conference on 21st to 23rd March2019. The theme of this conference is” From Excellence to Revolution in Medical Education.” Rawalpindi Medical University has always taken a lead to play a pivotal role in this regard. -
HEALTH Nov 30Th, 2013 - Volume:1, Issue: 6
HEALTH Nov 30th, 2013 - Volume:1, Issue: 6 Polio cases in Pakistan pass 2012 total IN THIS BULLETIN No debate on dengue deaths Health News 1-9 Anti-polio drive begins in twin cities today’ Militants free teachers after questioning DCO warns of polio virus carriers from tribal areas Humanitarian Organizations’ 10 Sindh dengue deaths reach 30 Interventions in Health Sector Mardan at high-risk as parents refuse to vaccinate children Moot on health innovations starts tomorrow Health Profile Lahore 12 Dengue patients keep pouring in Public health: All set for Dengue Day 9 out of 10 injections administered in Pakistan are unnecessary Articles 16 Polio virus strain found in Syria confirmed as originating from Pakistan: WHO Polio campaign: 2,755 teams to vaccinate 1.18m children in Faisalabad Health Maps 13,15,17,19 WHO-Report: WHO rejects NIH report on polio virus in Multan Health dept and WHO all set for vaccination drive Urdu News 21-23 15 percent hike in medicine prices withdrawn Maternal mortality rate in Pakistan highest in region Three districts to be listed as high-risk for dengue Health Directory 25-37 KP to unveil new health policy next week HEALTH FACILITY - LAHORE LAHORE TOWN WISE DISTRIBUTION OF DRUG USERS - 2011 MAPS PERSONS WITH DISABILITIES (PWDS) STATISTICS 2012 - PUNJAB ACUTE RESPIRATORY INFECTION - 2012 Legend HEALTH FACILITY - LAHORE "' Basic Health Unit "' Sub Health Centre Mian Munshi Hospital Railway Hospital Arooj Hospital Maqssoda Family Government Nawaz Shalamar Hospital Iqra Surraya "' Shah Abdul Latif Health Lady Sharif Hospital Murad Clinic Rural Health Centre Azeem Family Faree Clinic Center Aitcheson Hospital Hospital Pathi Ground Mayo Hospital Clinic Ali Hospital "' Muhammad Physician Hospital Janki Devi Hospital Tanveer Cairns Railway Maham Clinic "' Eisha Hospital MCH Filter Clinic British Clinic Hospital Rabia Clinic Pasban Waqar Clinic Ultrasound Zanib Clinic "&F Puff Clinic Agakhan Health Center Aftab Clinic Society Homeopathic Hyder Umar Hospital Clinic Laboratory Neelam Dr. -

A Comparision of Tablet Nifedipine with Tablet Methyldopa in Controlling Mild to Moderate Pregnancy Induced Hypertension (PIH)
ORIGINAL ARTICLE A Comparision of Tablet Nifedipine with Tablet Methyldopa in Controlling Mild to Moderate Pregnancy induced Hypertension (PIH) NAZIA FAKHIR1, HUMAIRA MASOOD2, WAJIHA KHANUM3, JAWERIA FAISAL4, SADIA KANWAL5, NIGHAT AFRIDI6 1Senior Registrar, Obstetrics & Gynaecology, Benazir Bhutto Hospital, Rawalpindi 2Senior Registrar, Benazir Bhutto Hospital, Rawalpindi 3Post graduate trainee Benazir Bhutto hospital, Rawalpindi. 4Associate professor, Obstetrics & Gynaecology, Al-Nafees medical college and hospital, Isra University Islamabad 5Assistant Professor, Al-Nafees Medical College and Hospital Isra University Islamabad 6Head of Obstetrics & Gynaecology, Department, Combined Military Hospital Peshawar Correspondence to: Dr Nazia Fakhir e-mail: [email protected] Cell 03136294236 ABSTRACT Objective: To compare the efficacy of tablet nifedipine and tablet methyldopa in controlling mild to moderate pregnancy induced hypertension. Study Design: Randomized control trial. Place and Duration of Study: Department of Obstetrics & Gynaecology Benazir Bhutto Hospital Rawalpindi Pakistan from 01 May 2019 to October 2019. Methodology: Two hundred and thirty six patients with mild to moderate pregnancy induced hypertension were selected and randomized based on lottery method to either group A or group B. Group A received tablet Methyldopa 250mg TDS while Group B received tablet Nifedipine 10mg bd. BP was checked 4 hourly for 24 hours and then decided which medicine control the BP best. Results: The mean age of the study group was 30.39±5.087 years. There was no statistically significant difference in the age of both groups. The majority of the patient in our study was multigravida, in the last trimester of pregnancy and had a history of hypertension in previous pregnancy. There were eight treatment failure in Methyldopa group while two treatment failure in Nifedipine group. -

Frequency and Predictors of Anxiety and Depression Among Pregnant
Ghaffar et al. BMC Women's Health (2017) 17:51 DOI 10.1186/s12905-017-0411-1 RESEARCHARTICLE Open Access Frequency and predictors of anxiety and depression among pregnant women attending tertiary healthcare institutes of Quetta City, Pakistan Rahila Ghaffar1, Qaiser Iqbal1, Adnan Khalid2, Fahad Saleem1, Mohamed Azmi Hassali3, Nosheen Sikandar Baloch4, Fiaz ud Din Ahmad5, Sajid Bashir6, Sajjad Haider1 and Mohammad Bashaar7* Abstract Background: Anxiety and depression (A&D) are commonly reported among pregnant women from all over the world; however, there is a paucity of workable data from the developing countries including Pakistan. The current study, therefore, aims to find out the frequency and predictors of A&D among pregnant women attending a tertiary healthcare institutes in the city of Quetta, in the Balochistan province, Pakistan. Methods: A questionnaire based, cross-sectional survey was conducted. The pre-validated Hospital Anxiety and Depression Scale (HADS) were used to assess the frequency of A&D among study respondents. Anxiety and depression scores were calculated via standard scoring procedures while logistic regression was used to identify the predictors of A&D. SPSS v. 20 was used for data analysis and p < 0.05 was taken as significant. Results: Seven hundred and fifty pregnant women responded to the survey. The majority of the respondents belonged to age group of 26–35 year (424, 56.4%) and had no formal education (283, 37.6%). Furthermore, 612 (81.4%) of the respondents were unemployed and had urban residencies (651, 86.6%). The mean anxiety score was 10.08 ± 2.52; the mean depression score was 9.51 ± 2.55 and the total HADS score was 19.23 ± 3.91 indicating moderate A&D among the current cohort. -

COVID-19 Laboratory Capacity, National Institute of Health, Islamabad
COVID – 19 Laboratory Capacity National Institute of Health, Islamabad 22 February 2021 S. No. Province/ City Category Functional Lab/Site Region (No) 1. Federal Islamabad Public National Institute of Health - (NIH) 2. (27) (27) PIMS – (POCT + PCR) 3. Private Islamabad Diagnostic Center (IDC) 4. Biotech Lab and Research Center 5. Metropole Laboratories 6. Capital Diagnostic Centre 7. Biogene 8. Shifa International 9. Excel Labs 10. Global Clinical Care Diagnostic Centre 11. Temar Diagnostics 12. Margalla Diagnostics and Clinics 13. Advanced Diagnostics Centre 14. Kulsum Intl Hospital 15. Maroof Hospital 16. Nayab Labs 17. Medikay Pvt limited 18. Akbar Niazi Teaching Hospital 19. Real Time PCR Diagnostic, Research & Reference Laboratories 20. Shaafi Hospital PWD 21. Crown Diagnostic Centre 22. Shaheen Medical Laboratories & Health Services 23. DAHA Lab and Diagnostic 24. Rehman Laboratories 25. Islamabad Health Care Laboratory 26. Public/Private MedAsk 27. IHITC Lab 28. Punjab Lahore Public Punjab AIDS Control Program incl Hepatitis Lab 29. (62) (35) Punjab Forensic Science Auth Lab 30. Jinnah Hospital 31. PKLI 32. Lahore General Hospital 33. CAMB 34. UVAS (BSL-3) 35. Lahore TB Program (BSL-3) 36. IPH Lahore 37. Private Chughtai Lab 38. Shaukat Khanum Memorial Hospital 39. Islamabad Diagnostic Center (IDC) 40. Rahila Research and Reference Lab 41. Venous Diagnostics 42. Hameed Lateef Hospital 43. Citilab & Research Centre 44. Alam International Lab 45. Horizon Molecular Laboratory 46. Agha Khan 47. Surgimed Lab 48. Testzone 49. Zeenat Lab 50. Genome Lab 51. Al Nasar Lab 52. Doctor Hospital 53. University of Lahore 54. Mughal Lab 55. Lab Genetix 56. Hormone Lab 57. -
Laboratory Testing Capacity
COVID – 19 Laboratory Capacity National Institute of Health, Islamabad 5 August 2021 S. No. Province/ City Category Functional Lab/Site Region (No) 1. Federal Islamabad Public National Institute of Health - (NIH) 2. (38) (38) PIMS – (POCT + PCR) 3. Private Islamabad Diagnostic Center (IDC) 4. Biotech Lab and Research Center 5. Metropole Laboratories 6. Capital Diagnostic Centre 7. Biogene 8. Shifa International 9. Excel Labs 10. Global Clinical Care Diagnostic Centre 11. Temar Diagnostics 12. Margalla Diagnostics and Clinics 13. Advanced Diagnostics Centre 14. Kulsum Intl Hospital 15. Maroof Hospital 16. Nayab Labs 17. Medikay Pvt limited 18. Akbar Niazi Teaching Hospital 19. Real Time PCR Diagnostic, Research & Reference Laboratories 20. Shaafi Hospital PWD 21. Crown Diagnostic Centre 22. Shaheen Medical Laboratories & Health Services 23. DAHA Lab and Diagnostic 24. Rehman Laboratories 25. Islamabad Health Care Laboratory 26. Biomaxx Lab and Diagnostic Centre 27. Ali Medical Centre 28. Ideal Labs & Diagnostic Center 29. European Diagnostic Center 30. BEKS Advanced Medical Services (Pvt) Ltd 31. Global Research and Reference Laboratories 32. Sharif Labs and Diagnostics (Pvt) Ltd 33. Nimra Diagnostic Centre (NDC) 34. Accurate Diagnostic & Covid PCR Lab 35. City Medicare Lab 36. Khan Labs & Diagnostic Center 37. Public/Private MedAsk 38. IHITC Lab 39. Punjab Lahore Public Punjab AIDS Control Program incl Hepatitis Lab 40. (81) (42) Punjab Forensic Science Auth Lab 41. Jinnah Hospital 42. PKLI 43. Lahore General Hospital 44. CAMB 45. UVAS (BSL-3) 46. Lahore TB Program (BSL-3) 47. IPH Lahore 48. Private Chughtai Lab 49. Shaukat Khanum Memorial Hospital 50. Islamabad Diagnostic Center (IDC) 51.