2016 Annual Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Oral Antifungal Agent Nailin® Capsules 100Mg Approved in Japan
FOR IMMEDIATE RELEASE January 19, 2018 Sato Pharmaceutical Co., Ltd. Eisai Co., Ltd. ORAL ANTIFUNGAL AGENT NAILIN® CAPSULES 100MG APPROVED IN JAPAN Sato Pharmaceutical Co., Ltd. (Headquarters: Tokyo, President and CEO: Seiichi Sato, “Sato Pharma”) obtained marketing and manufacturing approval for the oral antifungal agent NAILIN® Capsules 100mg containing the active ingredient fosravuconazole L-lysine ethanolate (“fosravuconazole”) for the treatment of onychomycosis in Japan on January 19, 2018. Sato Pharma and Eisai Co., Ltd. (Headquarters: Tokyo, CEO: Haruo Naito, “Eisai”) are jointly providing information on its proper use. Fosravuconazole, the active ingredient of NAILIN® Capsules 100mg, is a new triazole class oral antifungal component discovered by Eisai. Sato Pharma conducted a Phase III clinical study of the agent in patients with onychomycosis in Japan, and after confirming efficacy and safety of the agent in the study, Sato Pharma applied for marketing and manufacturing authorization in January 2017. Onychomycosis affects 1 in every 10 Japanese people, and there are an estimated approximately 11 million sufferers in Japan. With Sato Pharma now having obtained marketing and manufacturing approval for NAILIN® Capsules 100mg, as an oral treatment for onychomycosis, this is the first new treatment for the disease in approximately 20 years. By providing NAILIN® Capsules 100mg as a new option for the treatment of onychomycosis, Sato Pharma and Eisai will strive to fulfil the needs of onychomycosis patients and healthcare professionals. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG . -
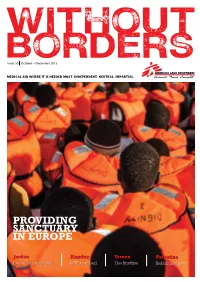
Providing Sanctuary in Europe
WITHOUT BORDERS Issue 30 October – December 2015 MEDICAL AID WHERE IT IS NEEDED MOST. INDEPENDENT. NEUTRAL. IMPARTIAL. PROVIDING SANCTUARY IN EUROPE Jordan Kunduz Yemen Palestine Reconstructing lives MSF bombed The frontline Rebuilding lives MSF_AD_Nablus_V2_ENG.pdf 1 10/27/15 8:05 AM UPFRONT CONTENTS WELCOME In the last three months MSF has faced disease, malnutrition, natural disasters and refugee crises. And in the early hours of 3 October, we faced an 10 YEARS air strike on our hospital in Kunduz, Afghanistan. This strike killed over 30 people, including at least 13 MSF staff members. The attack was devastating and the MSF community mourns the loss of our colleagues and patients. OF MENTAL 3| International news 5| In the region In this issue of Without Borders, we share MSF President Dr MSF situation updates Upgraded hospital Joanne Liu’s speech in response to the attack and we continue to highlight the numerous humanitarian situations MSF is responding to around the world. In Europe, we focus on the essential health care and support HEALTHCARE MSF is providing for refugees caught between the conflict and poverty of their homelands, and European borders. As of WHERE IT IS NEEDED MOST September, MSF staff have quite literally pulled more than 16,000 people from the Mediterranean. The European refugee crisis is just one of many situations in which MSF is providing emergency care and support for refugees 7| From the field 9| Special report and internally displaced people, but the relief and even joy of Refugee crisis Hospital bombed those who make it to land in Europe clearly illustrates the need for support and the cause for hope. -

R&D Model & Portfolio
R&D MODEL & PORTFOLIO ADAPTED TREATMENTS FOR THE BENEFIT OF NEGLECTED PATIENTS The R&D strategies developed by DNDi since its inception aim to Phase II trials as a potential single- address the immediate needs of patients by improving existing dose oral treatment and is the first therapeutic options in the short term, whilst undertaking longer molecule to arise from DNDi’s lead term research to identify and develop entirely new compounds optimization programme. which will be valuable adapted tools, particularly for elimination targets set by the World Health Organization. Although not Leishmaniasis is a complex family necessarily breakthrough medicines, six new treatments have of diseases, and the identification been delivered to date as a result of the short-term strategy, of new compounds has proved which have brought significant benefits to patients. challenging. Compound libraries from a variety of sources have been screened and, despite the inevitable The year 2015 has been a turning are orally available compounds for loss of compounds to attrition, NCEs point for DNDi, as long-term systemic use. The most clinically from the nitroimidazole, oxaborole, investments have now filled the advanced of these are for sleeping and aminopyrazole chemical drug development pipeline with sickness: fexinidazole, which was families are undergoing lead thirteen new chemical entities identified from compound mining optimization to combat Leishmania (NCEs) included by the end of the and is a ten day oral treatment, infections, with the nitroimidazole year, the vast majority of which and SCYX-7158, which is entering VL-0690 selected to go forward to 14 › DNDi Annual Report 2015 R&D MODEL & PORTFOLIO pre-clinical development in 2015. -

Minutes of the 612Thmeeting Ofthe State
Minutes of the 612thmeeting ofthe State Level Expert Appraisal Committee(SEAC) held on 18/03/2020 at Committee Room, Gujarat Pollution Control Board, Sector 10A,Gandhinagar. The 612thmeeting of the State Level Expert Appraisal Committee (SEAC) was held on 18th March 2020 at Committee Room, Gujarat Pollution Control Board, Sector 10A, Gandhinagar. Following members attended the meeting: 1. Dr. Dinesh Misra, Chairman, SEAC 2. Shri S. C. Srivastav, Vice Chairman, SEAC 3. Shri V. N. Patel, Member, SEAC 4. Shri. R. J. Shah, Member, SEAC 5. Shri A. K. Muley, Member, SEAC 6. Dr. V. K. Jain, Member, SEAC 7. Shri A. V. Shah, Secretary, SEAC The regular agenda of Appraisal, Screening & Scoping/ToR / EC – Reconsiderationcases were taken up. The Committee considered the applications made by project proponents, additional details submitted as required by the SEAC/SEIAA and details furnished in the Form-1, PFR, EIA-EMP reports. Proposal No. Name and Address of the Unit Remarks 1 SIA/GJ/IND2/27657/2018 M/s. Lincoln Pharmaceutical Limited Appraisal Block No. 176 (old Block No. 95/5-B), At – Khatraj, Ta. Kalol, Dist. Gandhinagar. Category of the unit: 5(f) Project status: New Project proponent (PP) has submitted online application vide no. SIA/GJ/IND2/27657/2018 on dated 05/11/2019 for obtaining Environmental Clearance. The SEAC had recommended TOR to SEIAA and SEIAA issued TOR to PP vide their letter dated 30/10/2018. Project proponent has submitted EIA Report prepared by M/s. Bhagwati Enviro Care Pvt. Ltd., Ahmedabad based on the TOR issued by SEIAA. Public Hearing of the Project was conducted by Gujarat Pollution Control Board at Project Site of M/s. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

A Abacavir Abacavirum Abakaviiri Abagovomab Abagovomabum
A abacavir abacavirum abakaviiri abagovomab abagovomabum abagovomabi abamectin abamectinum abamektiini abametapir abametapirum abametapiiri abanoquil abanoquilum abanokiili abaperidone abaperidonum abaperidoni abarelix abarelixum abareliksi abatacept abataceptum abatasepti abciximab abciximabum absiksimabi abecarnil abecarnilum abekarniili abediterol abediterolum abediteroli abetimus abetimusum abetimuusi abexinostat abexinostatum abeksinostaatti abicipar pegol abiciparum pegolum abisipaaripegoli abiraterone abirateronum abirateroni abitesartan abitesartanum abitesartaani ablukast ablukastum ablukasti abrilumab abrilumabum abrilumabi abrineurin abrineurinum abrineuriini abunidazol abunidazolum abunidatsoli acadesine acadesinum akadesiini acamprosate acamprosatum akamprosaatti acarbose acarbosum akarboosi acebrochol acebrocholum asebrokoli aceburic acid acidum aceburicum asebuurihappo acebutolol acebutololum asebutololi acecainide acecainidum asekainidi acecarbromal acecarbromalum asekarbromaali aceclidine aceclidinum aseklidiini aceclofenac aceclofenacum aseklofenaakki acedapsone acedapsonum asedapsoni acediasulfone sodium acediasulfonum natricum asediasulfoninatrium acefluranol acefluranolum asefluranoli acefurtiamine acefurtiaminum asefurtiamiini acefylline clofibrol acefyllinum clofibrolum asefylliiniklofibroli acefylline piperazine acefyllinum piperazinum asefylliinipiperatsiini aceglatone aceglatonum aseglatoni aceglutamide aceglutamidum aseglutamidi acemannan acemannanum asemannaani acemetacin acemetacinum asemetasiini aceneuramic -

Mediation for Peace
MEDIATION FOR PEACE The Centre for Humanitarian Dialogue (HD) is a private diplomacy organisation PHOTO CREDITS founded on the principles of humanity, impartiality, neutrality and independence. Its mission is to help prevent, mitigate, and resolve armed conflict through dialogue Page 4: Photo of Mr Espen Barth Eide. © HD - Photo credit: Alban Kakulya and mediation. Page 14: David Gorman in Indonesia. © HD Page 14: Oslo Forum banner. © HD Centre for Humanitarian Dialogue (HD) 114 rue de Lausanne, 1202 – Geneva, Switzerland Page 14: JEM and UNICEF Agreement. © HD Tel: +41 (0)22 908 11 30 Page 15: Nakuru County Peace Accord. © HD Email: [email protected] Page 15: Signing of the Tunisian Charter of Honour. © HD Website: www.hdcentre.org Page 16: HD Villa. © HD Follow HD on Twitter and Linkedin: Page 16: Member of Libyan forces. © Reuters/Esam Omran https://twitter.com/hdcentre Page 17: Government and Renamo sign a peace accord to end military hostilities. https://www.linkedin.com/company/centreforhumanitariandialogue © EPA-EFE/Andre Catueira Page 17: BOL Presentation to MILF, Duterte. © Government of the Philippines Cover images: Pages 35: Photo of Mr Espen Barth Eide. © HD – Photo credit: Alban Kakulya Front – Community mediator in the Sahel region. © HD Page 35: Photo of Mr Pierre Vimont. © Ministère français des Affaires étrangères Back – Demonstration against President Daniel Ortega in Nicaragua to demand the Page 36: Photo of Ms Sarah F. Cliffe. © Center on International Cooperation liberation of all political prisoners. © EPA-EFE/Jorge Torres Page 36: Photo of Mr Neil Janin. © HD – Photo credit: Alban Kakulya Design and layout: Rick Jones, StudioExile Page 36: Photo of Mr Armin Slotta. -

(MSF), to Be New Cleveringa Lecturer at Leiden University
Doctor Joanne Liu, International President of Médecins Sans Frontières (MSF), to be new Cleveringa lecturer at Leiden University Word of welcome by Rector prof. Carel Stolker Leiden, 25 November 2016 Dear professor Liu, Re-reading the famous opening lines of Charles Dickens' A Tale of Two Cities, it struck me how well they apply to our own time and age. Let me read them to you: “It was the best of times, it was the worst of times, it was the age of wisdom, it was the age of foolishness, it was the epoch of belief, it was the epoch of incredulity, it was the season of Light, it was the season of Darkness, it was the spring of hope, it was the winter of despair, ...” Dickens was, of course, writing about the age of the French Revolution and the Jacobin Reign of Terror that eventually followed. Our current global situation is different in many ways. And still, this is both the best of times and the worst of times, both the spring of hope and the winter of despair. Your own work and the work of your organisation, Médecins sans Frontières, Doctors without Borders, is a wonderful example of the best that humanity has to offer. You help people who need it most, often in situations where other organisations do not even dare to tread. And you do so without favouring any faction or any ethnic group, and without serving any specific political agenda. It certainly is the best of times when such an organisation receives widespread recognition and appreciation, including the 1999 Nobel Peace Prize, "in recognition of the organization's pioneering humanitarian work on several continents". -

Fosravuconazole L-Lysine Ethanolate | Medchemexpress
Inhibitors Product Data Sheet Fosravuconazole L-lysine ethanolate • Agonists Cat. No.: HY-16779B CAS No.: 914361-45-8 Molecular Formula: C₃₁H₄₀F₂N₇O₈PS • Molecular Weight: 739.73 Screening Libraries Target: Fungal; Parasite Pathway: Anti-infection Storage: Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month SOLVENT & SOLUBILITY In Vitro DMSO : 50 mg/mL (67.59 mM; Need ultrasonic) H2O : < 0.1 mg/mL (ultrasonic) (insoluble) Mass Solvent 1 mg 5 mg 10 mg Concentration Preparing 1 mM 1.3518 mL 6.7592 mL 13.5184 mL Stock Solutions 5 mM 0.2704 mL 1.3518 mL 2.7037 mL 10 mM 0.1352 mL 0.6759 mL 1.3518 mL Please refer to the solubility information to select the appropriate solvent. In Vivo 1. Add each solvent one by one: 10% DMSO >> 40% PEG300 >> 5% Tween-80 >> 45% saline Solubility: ≥ 2.5 mg/mL (3.38 mM); Clear solution 2. Add each solvent one by one: 10% DMSO >> 90% (20% SBE-β-CD in saline) Solubility: ≥ 2.5 mg/mL (3.38 mM); Clear solution BIOLOGICAL ACTIVITY Description Fosravuconazole L-lysine ethanolate (BMS-379224 L-lysine ethanolate), a prodrug of Ravuconazole, is an orally active broad spectrum antifungal agent. Fosravuconazole L-lysine ethanolate can be used for candidiasis, onychomycosis and parasitemia research[1][2][3]. In Vitro Fosravuconazole has potent in vitro antifungal activity against a wide range of fungal species, including Candida, Aspergillus , and Trichophyton species[1]. MCE has not independently confirmed the accuracy of these methods. -

Surveillance of Antifungal Use in Japan Oral Medicine + Injection Change in Antifungal Use for All of Japan by Rout of Administration 1
Surveillance of antifungal use in Japan Oral medicine + Injection Change in antifungal use for all of Japan by rout of administration 1 0.9 / day 0.8 0.7 0.6 0.5 0.4 Dose / inhabitants / 1,000 Dose 0.3 Daily 0.2 0.1 Defined 0 2013 2014 2015 2016 2017 2018 2019 Injection注射薬 内服薬Oral medicine(テルビナフィン・ホスラブコナゾールを除く (except for terbinafine and fosravuconazole) ) ホスラブコナゾールFosravuconazole テルビナフィンTerbinafine Oral medicine Change in antifungal use (oral medicine) for all of Japan 1 0.9 / day 0.8 0.7 0.6 0.5 0.4 Dose / inhabitants / 1,000 Dose 0.3 Daily 0.2 0.1 Defined 0 2013 2014 2015 2016 2017 2018 2019 フルシトシンFlucytosine ボリコナゾールVoriconazole イトラコナゾールItraconazole フルコナゾールFluconazole ホスラブコナゾールFosravuconazole テルビナフィンTerbinafine Injection Change in antifungal use (injection) for all of Japan 0.035 / day 0.03 0.025 0.02 0.015 Dose / inhabitants / 1,000 Dose 0.01 Daily 0.005 Defined 0 2013 2014 2015 2016 2017 2018 2019 Amphotericinアムホテリシン BB ミコナゾールMiconazole フルコナゾールFluconazole イトラコナゾールItraconazole Voriconazoleボリコナゾール Caspofunginカスポファンギン ミカファンギンMicafungin 〇The data are calculated from claims registered in the NDB. The data do not always reflect the precise antibiotic use because the data of patients who receive publicly funded health care are not always included. The numerical values are different from those of the surveillance of antibiotic sales (http://amrcrc.ncgm.go.jp/surveillance/020/20190902163931.html) due to the different data source. 〇The figures indicate drug utilization standardized by defined daily dose (DDD) per population and drug, called DID (DDDs/1,000 inhabitants/day) (Reference:https://www.whocc.no/atc_ddd_index/ ). -

Mining Sudanese Medicinal Plants for Natural Compounds Against Malaria and Neglected Tropical Diseases
Mining Sudanese Medicinal Plants for Natural Compounds against Malaria and Neglected Tropical Diseases INAUGURALDISSERTATION zur Erlangung der Würde eines Doktors der Philosophie vorgelegt der Philosophisch-Naturwissenschaftlichen Fakultät der Universität Basel von Abdelhalim Babiker Mohamed Mahmoud aus dem Sudan Basel, 2020 Originaldokument gespeichert auf dem Dokumentenserver der Universität Basel edoc.unibas.ch Genehmigt von der Philosophisch-Naturwissenschaftlichen Fakultät auf Antrag von Prof. Dr. Pascal Mӓser Prof. Dr. Thomas J. Schmidt Basel, den 23.06.2020 Prof. Dr. Martin Spiess Dekan To my father Who taught me that perseverance and hard work always pays off. May your inspiring soul rest in peace. Table of Contents Acknowledgment ...................................................................................................................................................... I Abbreviations .......................................................................................................................................................... III Summary .................................................................................................................................................................... V 1. INTRODUCTION: Neglected Tropical Diseases, Drug Discovery, and the Sudan .................... 1 1.1 Neglected Tropical Diseases ............................................................................................................................ 3 1.1.1 NTDs and Sudan .........................................................................................................................................