Official Report of This Meeting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Economy, Energy and Fair Work Committee: Annual Report 2020-21 Published in Scotland by the Scottish Parliamentary Corporate Body
Published 25 March 2021 SP Paper 1012 5th Report 2021 (Session 5) Economy, Energy and Fair Work Committee Comataidh Eaconamaidh, Lùth is Obair Chothromach Economy, Energy and Fair Work Committee: Annual Report 2020-21 Published in Scotland by the Scottish Parliamentary Corporate Body. All documents are available on the Scottish For information on the Scottish Parliament contact Parliament website at: Public Information on: http://www.parliament.scot/abouttheparliament/ Telephone: 0131 348 5000 91279.aspx Textphone: 0800 092 7100 Email: [email protected] © Parliamentary copyright. Scottish Parliament Corporate Body The Scottish Parliament's copyright policy can be found on the website — www.parliament.scot Economy, Energy and Fair Work Committee Economy, Energy and Fair Work Committee: Annual Report 2020-21, 5th Report 2021 (Session 5) Contents Introduction ____________________________________________________________1 Membership changes____________________________________________________1 Inquiries and reports_____________________________________________________2 COVID-19 – impact on Scotland’s businesses, workers and the economy ___________2 2021-22 Budget scrutiny _________________________________________________3 Energy Inquiry _________________________________________________________3 BiFab, the offshore wind energy sector and the Scottish supply chain ______________3 Scottish National Investment Bank draft missions ______________________________3 Climate Change Plan____________________________________________________4 One-off -

Scottish Government Events
For Operational Guidance Only - Not for Publication Scottish Government Events Sunday 15 November Joe FitzPatrick: Announces additional funding for prevention of obesity in Early Years (00:01) (news release) Desk Contact: Kirsty Jenkins 0131 244 3054 Monday 16 November Roseanna Cunningham: Takes part in COP26 Cast panel discussion, run by University of Edinburgh Business School on COP and the wellbeing economy (19:30) Desk Contact: Alice Robertson 07500 030559 Roseanna Cunningham: Speaks at launch of WWF and Scottish Power's COP 26 Climate Collaboration Challenge (14:00) (Twitter) Desk Contact: Alice Robertson 07500 030 559 Fiona Hyslop: Congratulates two Scottish finalists in the Festival UK 2022 innovation competition (00:01) (quote in stakeholder news release, Twitter) Desk Contact: Louise Aitken 07769 357170 Maree Todd: Comments on start of Adoption Week Scotland (10:00) (quote in stakeholder news release, Twitter) Desk Contact: Lana Montgomery 07880 462019 Jeane Freeman: Announces £1 million fund for digital devices in care homes (14:00) (news release) (Twitter) Desk Contact: Matt Paterson 07468 766475 Tuesday 17 November John Swinney: Launches this year's Read, Write, Count book bags as part of Book Week Scotland (09:30) (Twitter) Desk Contact: Richard Clarke 07467 447253 Wednesday 18 November Mairi Gougeon: Launches Buy a Puppy Safely animal welfare campaign (00:01) (news release, Twitter) Desk Contact: Thomas Barker 0131 244 5181 Fergus Ewing: Welcomes a new guide by Scottish Forestry to help small landholders plant new woodlands -
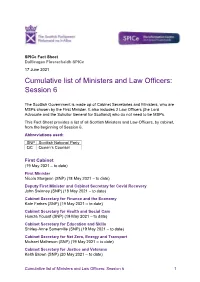
Cumulative List of Ministers and Law Officers: Session 6
SPICe Fact Sheet Duilleagan Fiosrachaidh SPICe 17 June 2021 Cumulative list of Ministers and Law Officers: Session 6 The Scottish Government is made up of Cabinet Secretaries and Ministers, who are MSPs chosen by the First Minister. It also includes 2 Law Officers (the Lord Advocate and the Solicitor General for Scotland) who do not need to be MSPs. This Fact Sheet provides a list of all Scottish Ministers and Law Officers, by cabinet, from the beginning of Session 6. Abbreviations used: SNP Scottish National Party QC Queen’s Counsel First Cabinet (19 May 2021 – to date) First Minister Nicola Sturgeon (SNP) (18 May 2021 – to date) Deputy First Minister and Cabinet Secretary for Covid Recovery John Swinney (SNP) (18 May 2021 – to date) Cabinet Secretary for Finance and the Economy Kate Forbes (SNP) (19 May 2021 – to date) Cabinet Secretary for Health and Social Care Humza Yousaf (SNP) (19 May 2021 – to date) Cabinet Secretary for Education and Skills Shirley-Anne Somerville (SNP) (19 May 2021 – to date) Cabinet Secretary for Net Zero, Energy and Transport Michael Matheson (SNP) (19 May 2021 – to date) Cabinet Secretary for Justice and Veterans Keith Brown (SNP) (20 May 2021 – to date) Cumulative list of Ministers and Law Officers: Session 6 1 Cabinet Secretary for Social Justice, Housing and Local Government Shona Robison (SNP) (20 May 2021 – to date) Cabinet Secretary for Rural Affairs and Islands Mairi Gougeon (SNP) (20 May 2021 – to date) Cabinet Secretary for the Constitution, External Affairs and Culture Angus Robertson (SNP) (20 -

Legacy Paper Published in Scotland by the Scottish Parliamentary Corporate Body
Published 22 March 2021 SP Paper 1008 12th Report, 2021 (Session 5) Health and Sport Committee Legacy Paper Published in Scotland by the Scottish Parliamentary Corporate Body. All documents are available on the Scottish For information on the Scottish Parliament contact Parliament website at: Public Information on: http://www.parliament.scot/abouttheparliament/ Telephone: 0131 348 5000 91279.aspx Textphone: 0800 092 7100 Email: [email protected] © Parliamentary copyright. Scottish Parliament Corporate Body The Scottish Parliament's copyright policy can be found on the website — www.parliament.scot Health and Sport Committee Legacy Paper, 12th Report, 2021 (Session 5) Contents Committee Remit________________________________________________________1 Committee Membership (at dissolution) _____________________________________2 Introduction ____________________________________________________________4 Getting started__________________________________________________________5 Business Planning Days _________________________________________________5 Strategic Plan and Vision 2016-2021 ________________________________________6 Summary of main activity this session ______________________________________7 Session 5 overview _____________________________________________________7 Scrutiny of the Scottish Government Budget__________________________________7 Systemic Inquiry Work ___________________________________________________9 Short and one-off inquiries________________________________________________9 Scrutiny of Public Bodies ________________________________________________10 -

2021 MSP Spreadsheet
Constituency MSP Name Party Email Airdrie and Shotts Neil Gray SNP [email protected] Coatbridge and Chryston Fulton MacGregor SNP [email protected] Cumbernauld and Kilsyth Jamie Hepburn SNP [email protected] East Kilbride Collette Stevenson SNP [email protected] Falkirk East Michelle Thomson SNP [email protected] Falkirk West Michael Matheson SNP [email protected] Hamilton, Larkhall and Stonehouse Christina McKelvie SNP [email protected] Motherwell and Wishaw Clare Adamson SNP [email protected] Uddingston and Bellshill Stephanie Callaghan SNP [email protected] Regional Central Scotland Richard Leonard Labour [email protected] Central Scotland Monica Lennon Labour [email protected] Central Scotland Mark Griffin Labour [email protected] Central Scotland Stephen Kerr Conservative [email protected] Central Scotland Graham Simpson Conservative [email protected] Central Scotland Meghan Gallacher Conservative [email protected] Central Scotland Gillian Mackay Green [email protected] Constituency MSP Name Party Email Glasgow Anniesland Bill Kidd SNP [email protected] Glasgow Cathcart James Dornan SNP [email protected] Glasgow Kelvin Kaukab Stewart SNP [email protected] Glasgow Maryhill and Springburn Bob Doris SNP [email protected] -

Open PDF 178KB
International Trade Committee Oral evidence: UK Freeports, HC 258 Wednesday 7 October 2020 Ordered by the House of Commons to be published on 7 October 2020. Watch the meeting Members present: Angus Brendan MacNeil (Chair); Mark Garnier; Mark Menzies; Taiwo Owatemi; Lloyd Russell-Moyle; Martin Vickers; Mick Whitley; Craig Williams. Questions 166 - 196 Witnesses II: Aidan McMahon, Deputy Director, Strategic Policy Division, Department of Finance, Northern Ireland Executive; Ivan McKee MSP, Minister for Trade, Investment and Innovation, Scottish Government; and Rebecca Evans MS, Minister for Finance and Trefnydd, Welsh Government. Examination of Witnesses Witnesses: Aidan McMahon, Ivan McKee and Rebecca Evans. Q166 Chair: We now move to our second panel. Thank you for joining us. Again a very illustrious panel. This is from the three Governments in Wales, Scotland and Northern Ireland. We have Aidan McMahon, Ivan McKee and Rebecca Evans, and I will let you all introduce yourselves in your own terms. Far be it from me to put words in anybody’s mouth here. Aidan McMahon: My name is Aidan McMahon, deputy director of the strategic policy division in the Department of Finance. My Minister leads and co-ordinates on behalf of the Executive in relation to the freeports policy. Thanks for the invite today. I would like to offer my Minister’s apologies for not being able to make the session. Chair: Thank you, apology accepted. Ivan McKee, who I might have met once or twice in the past. Ivan McKee: Feasgar math, Chair. Good afternoon. It is good to be here, and I am looking forward to talking to your Committee. -

Scottish Parliament Photographs of Msps
Photographs of MSPs Dealbhan de na BPA May 2021 Each person in Scotland is represented by 8 Members of the Scottish Parliament (MSPs); 1 constituency MSP and 7 regional MSPs. A region is a larger area which covers a number of constituencies. Scottish National Party Scottish Conservative and Unionist Party Scottish Labour Party Scottish Green Party Scottish Liberal Democrats No party affiliation C R Constituency Member Regional Member Contents MSP Photographs 2 Index of MSPs by Party 13 Index of MSPs by Constituency 15 Index of MSPs by Region 18 1 George Claire Adam Baker Paisley Mid Scotland and Fife C R Karen Jeremy Adam Balfour Banffshire and Lothian Buchan Coast C R Clare Colin Adamson Beattie Motherwell and Midlothian North Wishaw and Musselburgh C C Alasdair Neil Allan Bibby Na h-Eileanan West Scotland an Iar C R Tom Sarah Arthur Boyack Renfrewshire Lothian South C R Jackie Miles Baillie Briggs Dumbarton Lothian C R 2 Keith Jackson Brown Carlaw Clackmannanshire Eastwood and Dunblane C C Siobhian Finlay Brown Carson Ayr Galloway and West Dumfries C C Ariane Maggie Burgess Chapman Highlands and North East Islands Scotland R R Alexander Foysol Burnett Choudhury Aberdeenshire Lothian West C R Stephanie Katy Callaghan Clark Uddingston and West Bellshill Scotland C R Donald Willie Cameron Coffey Highlands and Kilmarnock and Islands Irvine Valley R C 3 Alex James Cole-Hamilton Dornan Edinburgh Glasgow Cathcart Western C C Angela Sharon Constance Dowey Almond Valley South Scotland C R Ash Jackie Denham Dunbar Edinburgh Aberdeen Eastern Donside -
Official Report
Meeting of the Parliament (Hybrid) Tuesday 16 March 2021 Session 5 © Parliamentary copyright. Scottish Parliamentary Corporate Body Information on the Scottish Parliament’s copyright policy can be found on the website - www.parliament.scot or by contacting Public Information on 0131 348 5000 Tuesday 16 March 2021 CONTENTS Col. TIME FOR REFLECTION ....................................................................................................................................... 1 POINT OF ORDER ............................................................................................................................................... 3 BUSINESS MOTION ............................................................................................................................................. 4 Motion moved—[Graeme Dey]—and agreed to. TOPICAL QUESTION TIME ................................................................................................................................... 5 Violence Against Women ............................................................................................................................. 5 Curriculum for Excellence (Organisation for Economic Co-operation and Development Review) .............. 9 COVID-19 ........................................................................................................................................................ 13 Statement—[First Minister]. The First Minister (Nicola Sturgeon) .......................................................................................................... -
Standards, Procedures and Public Appointments Committee
Standards, Procedures and Public Appointments Committee Thursday 7 June 2018 Session 5 © Parliamentary copyright. Scottish Parliamentary Corporate Body Information on the Scottish Parliament’s copyright policy can be found on the website - www.parliament.scot or by contacting Public Information on 0131 348 5000 Thursday 7 June 2018 CONTENTS Col. CROSS-PARTY GROUP ........................................................................................................................................... 1 STANDARDS, PROCEDURES AND PUBLIC APPOINTMENTS COMMITTEE 12th Meeting 2018, Session 5 CONVENER *Clare Haughey (Rutherglen) (SNP) DEPUTY CONVENER *Patrick Harvie (Glasgow) (Green) COMMITTEE MEMBERS *Tom Arthur (Renfrewshire South) (SNP) *Jamie Halcro Johnston (Highlands and Islands) (Con) *Tom Mason (North East Scotland) (Con) *Elaine Smith (Central Scotland) (Lab) *David Torrance (Kirkcaldy) (SNP) *attended THE FOLLOWING ALSO PARTICIPATED: Ivan McKee (Glasgow Provan) (SNP) CLERK TO THE COMMITTEE Katy Orr LOCATION The Adam Smith Room (CR5) 1 7 JUNE 2018 2 Is it perhaps a bit soon to set up a cross-party Scottish Parliament group? Would the group not be doing the same work as is being done through the pilots? Would Standards, Procedures and the group add value to the pilots? Public Appointments Committee Ivan McKee: The group would add value to the pilots. Clearly, it would allow MSPs to get involved Thursday 7 June 2018 and bring their perspectives, but it would also provide a forum in which the work of the pilots— which will involve looking in a fairly practical and [The Convener opened the meeting at 10:00] hands-on way at how basic income could work in Cross-party Group a specific area—and the theoretical aspects can be considered in one place. -

Lobbying Act 2016 Guidance
The Lobbying (Scotland) Act 2016 This is an Act of the Scottish Parliament which has created a Lobbying Register and introduced new duties to register lobbying activity which comes within the definition of “regulated lobbying”. The Act came fully in force on 12 March 2018. On that date the duty to provide information to the Lobbying Registrar took effect and a new criminal offences relating to the failure to provide information also came into operation. Lobbying Registrar The Church of Scotland is registered with the Lobbying Registrar and this covers all the Councils and Committees of the General Assembly of the Church of Scotland. If you are a congregation or Presbytery with 10 or more full time employees it is recommended you email [email protected] with your legal name and charity number and our Parliamentary Officer will arrange for you to be registered with the Lobbying Register. This is important as you must be entered on the Register within 30 days of your first act of regulated lobbying but there is a longer period for the actual act of regulated lobbying to be registered. Exemption for the Unincorporated Councils and Committees of the General Assembly of the Church of Scotland The Church of Scotland, i.e. the Councils and Committees of the General Assembly, have gained an exemption to all face to face communication with MSPs who are not Scottish Government Ministers (or a Law Officer, Special Adviser or Permanent Secretary). A list of the MSPs who do not come within this exemption because they are in the Cabinet or are Scottish Ministers can be found at the end of this circular. -

MINUTES of PROCEEDINGS Parliamentary Year 5, No. 110
MINUTES OF PROCEEDINGS Parliamentary Year 5, No. 110, Session 5 Meeting of the Parliament Thursday 18 March 2021 Note: (DT) signifies a decision taken at Decision Time. The meeting opened at 12.30 pm. 1. First Minister’s Questions: Questions were answered by the First Minister (Nicola Sturgeon). 2. Committee Meeting Times: The Minister for Parliamentary Business and Veterans (Graeme Dey), on behalf of the Parliamentary Bureau, moved S5M-24423— That the Parliament agrees that, under Rule 12.3.3B of Standing Orders, the Committee on the Scottish Government Handling of Harassment Complaints can meet, if necessary, at the same time as a meeting of the Parliament on Thursday 18 March 2021. The motion was agreed to. 3. Portfolio Questions: Questions on Economy, Fair Work and Culture were answered by a Cabinet Secretary and Ministers. 4. Local Government Finance (Scotland) Order 2021 [draft]: The Minister for Trade, Innovation and Public Finance (Ivan McKee) moved S5M-24395—That the Parliament agrees that the Local Government Finance (Scotland) Order 2021 [draft] be approved. The motion was agreed to (DT). 5. National Mission to Reduce Drug Deaths and Harms: The Minister for Drugs Policy (Angela Constance) moved S5M-24396—That the Parliament recognises that almost 3,400 people in Scotland have lost their lives to drug misuse in the last three years; believes that this scale of loss of life is not only a tragedy on the friends and families left behind, but is also a mark of shame on the nation; notes the Scottish Government's proposal to lead a national mission to reduce drug deaths and harms, and to agree that this is a public health emergency requiring partnership working and concerted action at all levels of public life, and welcomes the announcement of significant increased funding to support this national mission to be invested in a range of areas that will have the biggest impact in getting individuals into treatment and keeping them alive. -

Tuesday 28 February 2017 Business Bulletin Iris Ghnothaichean
Tuesday 28 February 2017 Business Bulletin Iris Ghnothaichean Today's Business Meeting of the Parliament Committee Meetings 2:00 pm Time for Reflection - Dr Mohammad 9:30am Economy, Jobs and Fair Work Ali Shomali, resident Imam and Director of Committee the Islamic Centre of England 9:30am Environment, Climate Change and followed by Parliamentary Bureau Motions Land Reform Committee followed by Topical Questions 10:00am Delegated Powers and Law Reform followed by Economy, Jobs and Fair Work Committee Committee Debate: Report on the Economic 10:00am Justice Committee Impact of Leaving the European Union followed by Business Motions followed by Parliamentary Bureau Motions 5:00 pm Decision Time followed by Members' Business — S5M- 03354 Kenneth Gibson: It’s OK to Talk. Period. Tuesday 28 February 2017 1 Today's Business Future Business Motions & Questions Legislation Other Gnothaichean an-diugh Gnothaichean ri teachd Gluasadan agus Ceistean Reachdas Eile Chamber | Seòmar Meeting of the Parliament 2:00 pm Time for Reflection - Dr Mohammad Ali Shomali, resident Imam and Director of the Islamic Centre of England followed by Parliamentary Bureau Motions followed by Topical Questions 1. Douglas Ross: To ask the Scottish Government what its position is on the consultation document, Policing 2026: Our 10 year strategy for policing in Scotland. (S5T-00419) 2. Daniel Johnson: To ask the Scottish Government, in light of reports that one-in-10 training places are going unfilled, what action it is taking to encourage more people into teaching. (S5T- 00412) 3. Liam McArthur: To ask the Scottish Government whether the Highlands and Islands Enterprise board will retain its current “strategic, operational and budgetary” decision-making powers in accordance with the recent vote in the Parliament.