Rohtas ( Sasaram )
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

B-Ed Student List for Current Session 2018-20
Person With Parent Annual Income S.No. Student Name DOB (DD/MM/YYYY) Father Name Mother Name Gender Caste Minority Status Email Id Mobile No. Aadhaar No. (in 12 digit) Village City Tehsil District State Pin Code Disability (In Rs.) SATYANARAYAN AMIT KUMAR 10/02/1997 [email protected] 9708051882 1 PRAJAPATI Indrasna Devi Male BC-I N.A 85000 735946468396 Nokha Nokha Sasaram Rohtas Bihar 802215 RAJENDRA SURYA PRAKASH 10/02/1997 [email protected] 9472931917 2 UPADHYAY Lalita Devi Male Gen. N.A 200000 956706930054 Mangraon Dehri On Sone Dehri On Sone Rohtas Bihar 821310 RAJENDRA PRASAD JYOTI KUMARI 10/10/1991 [email protected] 8873080048 3 SINGH Meena Devi Female BC-II N.A 85000 919442926780 Mani Sasaram Sasaram Rohtas Bihar 802217 SUMESHWAR DEEPAK KUMAR 02/10/1994 [email protected] 9576301984 4 SINGH Pushpa Devi Male BC-II N.A 90000 684435196910 Maruan Dinara Dinara Rohtas Bihar 802213 KHUSHBOO 12/28/1990 RAJBANSH SINGH [email protected] 7870306027 5 KUMARI Lalita Devi Female BC-II N.A 85000 680549423744 Mashihabad Sasaram Sasaram Rohtas Bihar 821115 POOJA KUMARI 10/04/1997 ANIL KUMAR [email protected] 9631858587 6 Pavitra devi Female SC N.A 92000 824942774100 Sakarouli Kochas Sasaram Rohtas Bihar 821108 PARAMHANSH 2/18/1997 GORAKH SETH [email protected] 8935822301 7 SETH Radhika Devi Male BC-II N.A 71000 727656403970 Takiya Sasaram Sasaram Rohtas Bihar 821113 SHIV PRAKASH 03/02/1995 BABAN SINGH [email protected] 7654917596 8 KUMAR Tetri Devi Male BC-I N.A 78000 713201058209 -

S.No DISTRICT VLE Name Mobile Number ADDRESS 1 ARARIA AMIT
S.No DISTRICT VLE Name Mobile Number ADDRESS ARARIA AMIT THAKUR 8210580921 TIRASKUND ARARIA 1 ARARIA Suman Devi 7070306717 Pipra ghat tola ward no-10 2 KSHITIZ KR ARARIA 8002927600 S/o Dinesh kr chaudhary,vill+po+block palasi,gp miya pur,araria,854333 3 CHOUDHARY SHRAVAN KUMAR 9470261463 / S/o Udichand bhagat,vill - lailokhar (gariyaa),po - pahusi,block+ps - ARARIA 4 BHAGAT 9199722522 kursakaanta,Araria,854332 ARARIA SURAJ JHA 8210905501 S/O-RAJKUMAR JHA,SOGHMARG,ARARIA-854331 5 ARARIA ABUNASAR KHAN 9708226603 VILL-BAIRGACHHI CHOWK,POST-ARARIA-854311 6 ARARIA HARDEV CHOURASIA 8002908166 S/o Udranand chaourasia,vill+po Gunwanti,block Raniganj,Araria,854312 7 S/o Satrudhan pd singh,h.no - 293,vill+po - Kushjhoul,block+ps - ARARIA JITENDRA KR SINGH 9199918908 8 Bhargama,Araria,854318 ARARIA DEWAKAR KUMAR 8210000876 AT-HASANPUR RANIGANJ, PO-MARYGANJ, PS-RANIGANJ 9 S/o Dev shankar roy,vill - mathura east,po+ps+block - narpatganj,dist - Araria,pin - ARARIA Suryabhushan Roy 7979831042 10 854335 S/O MD SHABBIR ALAM CHILHANIYA WARD NO 8 BAGNAGAR GARHBANAILI ARARIA MD ALAM 9939531771 11 JOKIHAT ARARIA RAHUL THAKUR 9430083371 marwari patti,ward no-17 12 9939960471/912348986 ARARIA AJIT KUMAR YADAV MAHISHAKOL ARARIYA 13 6 S/o Chandra kumar mallik,h.no - 42,po - ghurna,block+ps - ARARIA Nigam Kumar 9661213287 14 Narpatganj,Araria,854336 ARARIA Raman Jha 9430634408 S/o Sri Nitya Nand Jha, Vill - Rahatmeena, Block - Kursakanta, Dist - Araria, 15 ARARIA MD ASLAM 9110168570 AT+P.0+P.S-JOKIHAT; DIST-ARARIA 16 RATAN PRABHA W/o Chandan kr mandal,vill - wara/maanikpur,po+block+ps - Forbisganj,Araria - ARARIA 9608725491 17 KUMARI 854318 ARARIA AFROZ ALAM 9771213243 S/O-SHAMSUDDIN,MUSLIM TOLA,WARD NO-1,ARARIA-854311 18 ARARIA ABHILASH PANDIT 7461873031 AMHARA 19 ARARIA RAJESH KUMAR 7004007692 AT-RAJABALAI; P.0-GUNWANTI; P.S-RANIGANJ; ARARIA 20 ARARIA HARE SAH 9955019540 AT BHORHAR PO BHANGHI ARARIA BIHAR 21 S/o Md Salimuddin,vill - budheshwari,po - rampur mohanpur,block+ps+dist - ARARIA MD. -

State District Name of Bank Bank Branch/ Financial Literacy Centre
State District Name of Bank Branch/ Address ITI Code ITI Name ITI Address State District Phone Email Bank Financial Category Number Literacy Centre Bihar Araria State Araria Lead Bank Office, PR10000055 Al-Sahaba Industrial P Alamtala Forbesganj Bihar Araria NULL Bank of ADB Building, Training Institute India Araria, Pin- 854311 Bihar Arwal PNB ARWAL ARWAL PR10000083 Adarsh ITC P Umerabad Bihar Arwal NULL Bihar Arwal PNB ARWAL ARWAL PR10000284 Shakuntalam ITC P Prasadi English Bihar Arwal NULL Bihar Arwal PNB ARWAL ARWAL PR10000346 Aditya ITC P At. Wasilpur, Main Road, Bihar Arwal NULL P.O. Arwal, Bihar Arwal PNB ARWAL ARWAL PR10000396 Vikramshila Private P At. Rojapar, P.O. Arwal Bihar Arwal NULL ITI Bihar Arwal PNB ARWAL ARWAL PR10000652 Ram Bhaman Singh P At-Purani Bazar P.o+P.S- Bihar Arwal NULL Private ITI Arwal Bihar Arwal PNB ARWAL ARWAL PR10000677 Sukhdeo Institute Of P Kurtha, Arwal Bihar Arwal NULL Tecnology Private ITI, Bihar Arwal PNB ARWAL ARWAL PR10000707 Dr. Rajendra Prasad P Mubarkpur, Kurtha Arwal Bihar Arwal NULL Private ITI, Bihar Aurangabad PUNJAB DAUDNAGAR DAUDNAGAR PR10000027 New Sai Private ITI- P Aurangabad Road, Bihar Aurangabad NULL NATIONA Bhakharuan More, , Tehsil- L BANK Daudnagar , , Aurangabad - 824113 Bihar Aurangabad PUNJAB AURANGABAD AURANGABAD PR10000064 Adharsh Industrial P Josai More Udyog Bihar Aurangabad NULL NATIONA Training Centre Pradhikar Campus L BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000108 Sardar Vallabh Bhai P Daudnagar Bihar Aurangabad NULL BIHAR Patel ITC, Daudnagar GRAMIN BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000142 Adarsh ITC, P AT-,Growth centre ,Jasoia Bihar Aurangabad NULL BIHAR Daudnagar More Daudnagar GRAMIN BANK Bihar Aurangabad PUNJAB RATANUA RATANUA PR10000196 Progresive ITC P At-Growth Center Josia Bihar Aurangabad NULL NATIONA More L BANK Bihar Aurangabad MADHYA DAUDNAGAR DAUDNAGAR PR10000199 Arya Bhatt ITC P Patel Nagar, Daud Nagar Bihar Aurangabad NULL BIHAR GRAMIN BANK Bihar Aurangabad PUNJAB OLD GT RD. -

Dist. Rohtas, Bihar Usari Gidha
83°15'0"E 83°30'0"E 83°45'0"E 84°0'0"E 84°15'0"E 84°30'0"E MEDANI PUR SAISER JAMSONA SEMARI ITWAN BISIKALA BHARA SARA Koath (NP) © D A W A TT H BHUI SAHI NAUN BABHNAUL GIDHA DIST. ROHTAS, BIHAR USARI GIDHA DERGAUN GARA BHANPUR LILWACH GUNSEJ DAWATH GOSAL DIH SIOBAHAR AGRER KALA NARWAR 30 S U R Y A P U R A JAM RODH 0 S U R Y A P U R A KARANJ .H KUCHHILA N SURAJ PURA MOHINI N HARIBANS PUR SURAJ PURA N " " 0 BALIHAR 0 ' KUSUMHRA MORAUNA ' 5 CHITAWN 5 NAUWAN AKODHA D II N A R A 1 SARAYA 30 1 ° N.H 0 JAMORI ° 5 DINARA TENUAJ 5 2 KOCHAS CHITAWN 2 MAHARODH NONHAR SHIWPUR KHAIRA BHUDHAR MORAUNA CHITTAINI K O C H A S RAJPUR B IIK R A M G A N JJ Bikramganj (NP) LAHERI KANJAR MUNJI SAMHUTI GHUSIYA-KALAN I2 MANPUR BIKRAMGANJ BALATHARI CHANDI ENGLISH KATHRAI CHILHAR;UWA BALIA GHUSIYAI2 KHURD INDEX MAP REDIA SARAWAN JONHI KARAKAT PACHIM CHAMPAR* KAPASIYA GHUSIYAKALA CHIKSIL SAKLA KARMAINI AGARSI DIHRA ± AKODHI MOTHA SONBARSA ARANG KHAIRA SAHMAL MANI JAI SHREE DANWAR MANJHAULI GHUSIYAKALA KIRHI SHIWAN KARAHANSI MANJHAULI AMONA PURBI CHAMPARAN BAKSARA GARURA SITAMARHI BARAHRI KARUP SEMARI K A R A K A TT SHEOHAR DHARAMPURA I2 GOPALGANJ BENSAGAR MADHUBANI DHANHARA S A N JJH A U LL IISANJHAULI KAITHI AMARTHA KISHANGANJ AMAITHI SUPAUL KARGAHAR SOTWA GAMHARIYA ARARIA ARARUWA SENDUWAR UDAI PUR GORARI SIWAN MUZAFFARPUR BHOKHARI NONSARI BURHAWAL DARBHANGA RUPAITHA DEO SAMARDIHA KHIRIYANW K A R G A H A R Nokha (NP) BARNA SARAN SHIYAWAK SAMASTIPUR BARADIH SAHARSAMADHEPURA PURNIA GHUSIA CHATTONA VAISHALI I2 ) BASDIHA NOKHA PARARIYA PARASIYA THORSON MANGRAWAN HATHINI -

Annexure-V State/Circle Wise List of Post Offices Modernised/Upgraded
State/Circle wise list of Post Offices modernised/upgraded for Automatic Teller Machine (ATM) Annexure-V Sl No. State/UT Circle Office Regional Office Divisional Office Name of Operational Post Office ATMs Pin 1 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA PRAKASAM Addanki SO 523201 2 Andhra Pradesh ANDHRA PRADESH KURNOOL KURNOOL Adoni H.O 518301 3 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM AMALAPURAM Amalapuram H.O 533201 4 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Anantapur H.O 515001 5 Andhra Pradesh ANDHRA PRADESH Vijayawada Machilipatnam Avanigadda H.O 521121 6 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA TENALI Bapatla H.O 522101 7 Andhra Pradesh ANDHRA PRADESH Vijayawada Bhimavaram Bhimavaram H.O 534201 8 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA VIJAYAWADA Buckinghampet H.O 520002 9 Andhra Pradesh ANDHRA PRADESH KURNOOL TIRUPATI Chandragiri H.O 517101 10 Andhra Pradesh ANDHRA PRADESH Vijayawada Prakasam Chirala H.O 523155 11 Andhra Pradesh ANDHRA PRADESH KURNOOL CHITTOOR Chittoor H.O 517001 12 Andhra Pradesh ANDHRA PRADESH KURNOOL CUDDAPAH Cuddapah H.O 516001 13 Andhra Pradesh ANDHRA PRADESH VISAKHAPATNAM VISAKHAPATNAM Dabagardens S.O 530020 14 Andhra Pradesh ANDHRA PRADESH KURNOOL HINDUPUR Dharmavaram H.O 515671 15 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA ELURU Eluru H.O 534001 16 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudivada Gudivada H.O 521301 17 Andhra Pradesh ANDHRA PRADESH Vijayawada Gudur Gudur H.O 524101 18 Andhra Pradesh ANDHRA PRADESH KURNOOL ANANTAPUR Guntakal H.O 515801 19 Andhra Pradesh ANDHRA PRADESH VIJAYAWADA -

Report of the Examiner of Local Accounts, Bihar For
REPORTOF THEEXAMINEROFLOCALACCOUNTS,BIHAR FORTHEYEARENDED 31STMARCH2009and2010 PANCHAYATRAJINSTITUTIONS GOVERNMENTOFBIHAR i TABLEOFCONTENTS Particulars Paragraph Page No. PrefaceVII OverviewIX CHAPTERͲI:IntroductiontoPRIsintheStateofBihar Background 1.1 1 StateProfile 1.2 1 OrganisationalStructureofPRIs 1.3 3 PowersandRolesofStateGovernmentinrelationto 1.4 4 PRIs DelegationofFunctionstoPRIs 1.5 5 BestPractices 1.6 6 AuditArrangement 1.7 6 AuditCoverage 1.8 7 StatusofRecoverybySurchargeProceedings 1.9 7 Impactofaudit 1.10 7 CHAPTERͲII:FinancialManagementandReporting FundFlowArrangement 2.1 8 NonͲrealisationofrevenue 2.2 9 Lossof` 1.34lakhduetoirregularremissionbythe 2.3 11 ChiefExecutiveOfficer Misappropriationof`0.23croreinPanchayatSamiti, 2.4 12 Punpun Advancesof`104.18crorelying 2.5 12 unadjusted/unrecovered Expenditureonidlestaff 2.6 12 MaintenanceofAccountsbyPRIs 2.7 13 Upkeepofrecords 2.8 14 StatusofpresentationofGPFSinPRI 2.9 15 Recommendation 2.10 16 CHAPTERͲIII:InternalControlMechanism Internalcontrols 3.1 17 i Commonlapsesinmaintenanceofrecordsrelatingto 3.2 17 executionofworks SegregationofDuties 3.3 18 Monitoring 3.4 18 InternalAudit 3.5 20 ExternalAudit 3.6 21 Poorresponsetoauditobservations 3.7 21 PersistenceofIrregularities 3.8 22 AnnualAdministrativeReport(AAR) 3.9 23 Recommendation 3.10 23 CHAPTERͲIV:ExecutionofSchemes SGRYschemes 4.1 24 IrregularitiesinSGRYschemesmeantforSC/ST 4.1.1 24 community IrregularitiesinExecutionofschemes 4.1.2 25 IrregularitiesrelatedtoFoodGrainsinSGRY 4.1.3 27 NationalRuralEmploymentGuaranteeAct/BREGS -

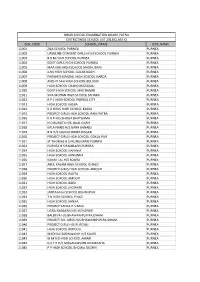
School with School Code.Xlsx
blkname schcd schname schmgt_desc schcat_desc Department SASARAM 10320100101 P S BANSA Primary only with grades 1 to 5 of Education Private SASARAM 10320100102 DEDICATED PUBLIC SCHOOL Secondary with grades 1 to 10 Unaided Department SASARAM 10320100301 P S DURGAPUR Primary only with grades 1 to 5 of Education Department SASARAM 10320100401 M S AMRA TALAB Upper Primary with grades 1 to 8 of Education Private SASARAM 10320100402 JEMS D . C . C SCHOOL KARBANDIYA Upper Primary with grades 1 to 8 Unaided Private SASARAM 10320100403 R.B.S PUBLIC SCHOOL Upper Primary with grades 1 to 8 Unaided Un- SASARAM 10320100404 DAYA NIDHI INTERNATIONAL SCHOOL Upper Primary with grades 1 to 8 Recognised THE MANAV BHARTI PUBLIC SCHOOL Un- SASARAM 10320100405 Upper Primary with grades 1 to 8 AMRA TALAB Recognised Un- SASARAM 10320100406 J.P MISSION SCHOOL Upper Primary with grades 1 to 8 Recognised NEW BAL VIKASH ENGLISH SCHOOL Un- SASARAM 10320100407 Upper Primary with grades 1 to 8 AMARA Recognised Department SASARAM 10320100501 URDU P S AMARI Primary only with grades 1 to 5 of Education Department SASARAM 10320100502 NEW P S AMARI Primary only with grades 1 to 5 of Education Department SASARAM 10320100601 UPGRADED H S DAWANPUR (2013-14) Higher Secondary with grades 1 to 12 of Education Un- SASARAM 10320100602 BABA KIDS GARDEN SCHOOL Upper Primary with grades 1 to 8 Recognised Department SASARAM 10320100702 NEW P S KARMA Primary only with grades 1 to 5 of Education Department SASARAM 10320101001 P S ADAMAPUR Primary only with grades 1 to 5 of Education -

Citizen Registration Report ( District : Rohtas) S.No
20-Aug-2018 06:04:22 PM Citizen Registration Report ( District : Rohtas) S.No. District Block Panchayat Dealer License FPShop No Name Mobile No 1 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 ARUN KUMAR CHOUBEY 8294376001 2 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 ANJANI KANT PANDEY 8002120143 3 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 MURHARAM ANSARI 8521925135 4 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 LAL BIHARI RAM 9801106495 5 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 PRABHA DEVI 9661912855 6 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 RAMABADAN SINGH 8809298872 7 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 BISHUNPATO DEVI 9576665648 8 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 KRISHNA PANDEY 8521868036 9 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 RAM NATH CHAUBEY 9939478255 10 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 BAIJNATH CHOUBEY 9939477255 11 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 JANARAN PANDEY 9162199711 12 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 SURENDRA SINGH 9006039260 13 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 GOVARDHAN CHAUBEY 9431680020 14 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 SUDHIR KUMAR SINGH 9455057992 15 Rohtas Akorhi Gola Tet Rarh Ajit Kumar Singh 26/07 123400300096 RAVI SHANKAR SINGH 9572138265 16 Rohtas -

TACR: India: Preparing the Bihar State Highways II Project
Technical Assistance Consultant’s Report Project Number: 41629 October 2010 India: Preparing the Bihar State Highways II Project Prepared by Sheladia Associates, Inc. Maryland, USA For Road Construction Department Government of Bihar This consultant’s report does not necessarily reflect the views of ADB or the Government concerned, and ADB and the Government cannot be held liable for its contents. (For project preparatory technical assistance: All the views expressed herein may not be incorporated into the proposed project’s design. TA No. 7198-INDIA: Preparing the Bihar State Highways II Project Final Report TTTAAABBBLLLEEE OOOFFF CCCOOONNNTTTEEENNNTTTSSS 1 INTRODUCTION .............................................................................................................................. 8 1.1 INTRODUCTION .............................................................................................................................. 8 1.2 PROJECT APPRECIATION............................................................................................................. 8 1.2.1 Project Location and Details 9 1.2.2 Road Network of Bihar 11 1.3 PERFORMANCE OF THE STUDY ................................................................................................ 14 1.3.1 Staff Mobilization 14 1.3.2 Work Shop 14 1.4 STRUCTURE OF THE FINAL REPORT ....................................................................................... 14 2 SOCIO ECONOMIC PROFILE OF PROJECT AREA .................................................................. -
Sch Code School Name Dist Name 11001 Zila School
BIHAR SCHOOL EXAMINATION BOARD PATNA DISTRICTWISE SCHOOL LIST 2013(CLASS X) SCH_CODE SCHOOL_NAME DIST_NAME 11001 ZILA SCHOOL PURNEA PURNEA 11002 URSULINE CONVENT GIRLS HIGH SCHOOL PURNEA PURNEA 11003 B B M HIGH SCHOOL PURNEA PURNEA 11004 GOVT GIRLS HIGH SCHOOL PURNEA PURNEA 11005 MAA KALI HIGH SCHOOL MADHUBANI PURNEA 11006 JLNS HIGH SCHOOL GULAB BAGH PURNEA 11007 PARWATI MANDAL HIGH SCHOOL HARDA PURNEA 11008 ANCHIT SAH HIGH SCHOOL BELOURI PURNEA 11009 HIGH SCHOOL CHANDI RAZIGANJ PURNEA 11010 GOVT HIGH SCHOOL SHRI NAGAR PURNEA 11011 SIYA MOHAN HIGH SCHOOL SAHARA PURNEA 11012 R P C HIGH SCHOOL PURNEA CITY PURNEA 11013 HIGH SCHOOL KASBA PURNEA 11014 K D GIRLS HIGH SCHOOL KASBA PURNEA 11015 PROJECT GIRLS HIGH SCHOOL RANI PATRA PURNEA 11016 K G P H/S BHOGA BHATGAMA PURNEA 11017 N D RUNGTA H/S JALAL GARH PURNEA 11018 KALA NAND H/S GARH BANAILI PURNEA 11019 B N H/S JAGNICHAMPA NAGAR PURNEA 11020 PROJECT GIRLS HIGH SCHOOL GOKUL PUR PURNEA 11021 ST THOMAS H S MUNSHIBARI PURNEA PURNEA 11023 PURNEA H S RAMBAGH,PURNEA PURNEA 11024 HIGH SCHOOL HAFANIA PURNEA 11025 HIGH SCHOOL KANHARIA PURNEA 11026 KANAK LAL H/S SOURA PURNEA 11027 ABUL KALAM HIGH SCHOOL ICHALO PURNEA 11028 PROJECT GIRLS HIGH SCHOOL AMOUR PURNEA 11029 HIGH SCHOOL RAUTA PURNEA 11030 HIGH SCHOOL AMOUR PURNEA 11031 HIGH SCHOOL BAISI PURNEA 11032 HIGH SCHOOL JHOWARI PURNEA 11033 JANTA HIGH SCHOOL BISHNUPUR PURNEA 11034 T N HIGH SCHOOL PIYAZI PURNEA 11035 HIGH SCHOOL KANJIA PURNEA 11036 PROJECT KANYA H S BAISI PURNEA 11037 UGRA NARAYAN H/S VIDYAPURI PURNEA 11038 BALDEVA H/S BHAWANIPUR RAJDHAM -

Press Note Bihar 2020
भारत निर्ााचि आयोग ELECTION COMMISSION OF INDIA Tel. No. 011-23052246 निर्ााचि सदि, Fax 011-23052001 अशोक रोड, िई दद쥍 ली-110001. Website: www.eci.gov.in Nirvachan Sadan, Asoka Road, New Delhi-110001 No. ECI/PN/64/2020 Dated:25th September, 2020 PRESS NOTE Subject: General Election to the Legislative Assembly of Bihar, 2020 -reg. The term of the Legislative Assembly of Bihar is due to expire on 29.11.2020. The term and strength of the assembly is indicated as below: Name of State Term of Assembly No. of Assembly Seats Bihar 30.11.2015 to 29.11.2020 243 81 The Election Commission of India (hereinafter ECI) is committed to hold free, fair and safe election to the Legislative Assembly of Bihar before the cessation of its term, in exercise of the authority and powers conferred upon under Article 324 read with Article 172 (1) of the Constitution of India and Section 15 of the Representation of the People Act, 1951. 1. Assembly Constituencies- The total number of Assembly Constituencies in the State of Bihar and seats reserved for the Scheduled Castes and the Scheduled Tribes, as determined by the Delimitation of Parliamentary and Assembly Constituencies Order, 2008, are as under: - State Total No. of ACs Reserved for SCs Reserved for STs Bihar 243 38 2 2. Broad Guidelines to be followed during entire election processes for all persons- 1) Every person shall wear face mask during every election related activity. 2) At the entry of hall/ room/ premises used for election purposes: (a) Thermal Scanning of all persons shall be carried out; (b) Sanitizer shall be made available at all locations. -
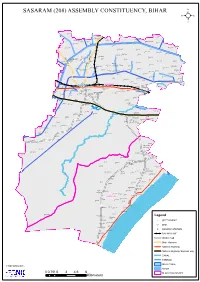
Sasaram (208) Assembly Constituency, Bihar ² !
SASARAM (208) ASSEMBLY CONSTITUENCY, BIHAR ² ! ! ! ! ! ! ! ! Fatepur ! ! ! ! ! Agrer ! Diliva ! ! ! ! Diiya ! ! Ramgarh ! Parsantola ! Mosahebpur ! ! ! Raksiya Nimiya Kothara ! Babhan Purwa ! ! Karup Rasulpur Bhagwanpur Jhalkhoriaya Sumbha Garura ! ! ! ! ! ! AKasi ! ! Bishunur ! ! Bhainsahi ! Samardiha ! ! Chamraha Paisara ! Rudana ! ! Mokar ! ! ! ! Tiwari Dih ! ! Barka Mor ! ! Chhotka Mor Mau Diha Belwa ! Kunrwa ! ! ! ! ! Gamhariya ! Semra 2 ! ! S ! 1 Bhorman H ! Nekara H 1 ! Pipri 7 Baradih S ! Balpur ! ! ! Bara Dih Jaipur Chitauli Baijla ! ! ! ! ! Khurhunu Chitauli ! ! Birajpur ! ! Nahauna ! ! ! Turki Kat Dehri Gotpa Jigina ! ! Karam Dihri ! Chhatarpur ! Kaupa Dih ! ! ! ! ! Chimney Basuhara ! Bararhi ! Uchitpur ! Æb! ! Dhuan Tendua Muradabad ! Sumbha ! Nirmalpur ! ! Sukharikhera Patiya ! ! Bishunpur ! Lodhi ! ! Shahpur Dumariya Karma ! ! ! Ugar Bigha ! Ahrawan ! ! Bisrampur Bharar ! ! ! ! Nima Durgapur ! ! Rampur Dawanpur ! ! Jagdaun Dih ! Amri ! Gajrah ! ! ! Dhan Purwa ! Amra ! SASARAM Æb SASARAM ! NH2 Almapur Belthua Beda ! ! ! ! R Sasaram Sita Bigha ! Naniatola Fazalganj ! ! ! ! Madaini SASARAM ! Dayal Æb ! ! ! Bigha ! Banrasia ! Barhaiyabagah ! Rameshwarganj KARWANDIYA ! Basantnur Kar Purwa ! Belarh ! ! Khara ! ! ! Patelganj ! Fazilpur ! ! ! ! NH Kadirganj Gaighat ! 2 ! ! ! Mahranian ! ! Gijwahi Singuhi ! ! Naugain ! Bhadokhara Wazirganj ! ! ! ! ! ! Agni ! Dangra ! Kachanpur ! ! Karkhana ! ! Belahar ! ! ! ! ! Rahuliya ! ! Sikariya Burhan ! ! ! ! ! Shivpur ! Dhankarha ! Lerua ! Dhanpurwa Malanw ! ! Chintawanpur ! ! Bhagwan Bigha