COVID-19) Pandemic December 18, 2020
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Coronavirus Preparedness and Response Hearing
CORONAVIRUS PREPAREDNESS AND RESPONSE HEARING BEFORE THE COMMITTEE ON OVERSIGHT AND REFORM HOUSE OF REPRESENTATIVES ONE HUNDRED SIXTEENTH CONGRESS SECOND SESSION MARCH 11–12, 2020 (A TWO DAY HEARING) Serial No. 116–96 Printed for the use of the Committee on Oversight and Reform ( Available on: http://www.govinfo.gov, oversight.house.gov or docs.house.gov U.S. GOVERNMENT PUBLISHING OFFICE 40–428 PDF WASHINGTON : 2020 COMMITTEE ON OVERSIGHT AND REFORM CAROLYN B. MALONEY, New York, Chairwoman ELEANOR HOLMES NORTON, District of JIM JORDAN, Ohio, Ranking Minority Member Columbia PAUL A. GOSAR, Arizona WM. LACY CLAY, Missouri VIRGINIA FOXX, North Carolina STEPHEN F. LYNCH, Massachusetts THOMAS MASSIE, Kentucky JIM COOPER, Tennessee MARK MEADOWS, North Carolina GERALD E. CONNOLLY, Virginia JODY B. HICE, Georgia RAJA KRISHNAMOORTHI, Illinois GLENN GROTHMAN, Wisconsin JAMIE RASKIN, Maryland JAMES COMER, Kentucky HARLEY ROUDA, California MICHAEL CLOUD, Texas RO KHANNA, California BOB GIBBS, Ohio DEBBIE WASSERMAN SCHULTZ, Florida CLAY HIGGINS, Louisiana JOHN P. SARBANES, Maryland RALPH NORMAN, South Carolina PETER WELCH, Vermont CHIP ROY, Texas JACKIE SPEIER, California CAROL D. MILLER, West Virginia ROBIN L. KELLY, Illinois MARK E. GREEN, Tennessee MARK DESAULNIER, California KELLY ARMSTRONG, North Dakota BRENDA L. LAWRENCE, Michigan W. GREGORY STEUBE, Florida STACEY E. PLASKETT, Virgin Islands FRED KELLER, Pennsylvania JIMMY GOMEZ, California ALEXANDRIA OCASIO-CORTEZ, New York AYANNA PRESSLEY, Massachusetts RASHIDA TLAIB, Michigan KATIE PORTER, California DEB HAALAND, New Mexico DAVID RAPALLO, Staff Director DANIEL REBNORD, Subcommittee Staff Director ALEXANDRA GOLDEN, Chief Health Counsel RICHARD TRUMKA, Subcommittee Staff Director AMY STRATTON, Clerk CHRISTOPHER HIXON, Minority Staff Director CONTACT NUMBER: 202-225-5051 (II) CONTENTS MARCH 11 AND 12, 2020 (DAY 1 AND DAY 2) Page WITNESSES Dr. -

1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27
Case 2:20-cv-04074 Document 1 Filed 05/04/20 Page 1 of 27 Page ID #:1 1 Mary E. Alexander, Esq. (State Bar No. 104173) Brendan D.S. Way, Esq. (State Bar No. 261705) 2 MARY ALEXANDER & ASSOCIATES, P.C. 44 Montgomery Street, Suite 1303 3 San Francisco, California 94104 Telephone: (415) 433-4440 4 Facsimile: (415) 433-5440 5 Elizabeth J. Cabraser (State Bar No. 083151) [email protected] 6 Jonathan D. Selbin (State Bar No. 170222) [email protected] 7 LIEFF CABRASER HEIMANN & BERNSTEIN, LLP 8 275 Battery Street, 29th Floor San Francisco, CA 94111-3339 9 Telephone: 415.956.1000 Facsimile: 415.956.1008 10 11 Attorneys for Plaintiff 12 UNITED STATES DISTRICT COURT 13 CENTRAL DISTRICT OF CALIFORNIA 14 15 CHRISTOPHER WEIDNER, Case No. 2:20-cv-4074 Individually and as Personal 16 Representative of the Decedent, PLAINTIFF’S COMPLAINT FOR CARL WEIDNER, DAMAGES 17 Plaintiff, 1. NEGLIGENCE – WRONGFUL 18 DEATH, 46 U.S.C. § 30301 et seq. v. 19 2. NEGLIGENCE - WRONGFUL CARNIVAL CORPORATION, DEATH 20 CARNIVAL PLC, and PRINCESS CRUISE LINES LTD., 3. GROSS NEGLIGENCE – 21 WRONGFUL DEATH Defendants. 22 23 COMPLAINT 24 Plaintiff CHRISTOPHER WEIDNER, Individually and as Personal 25 Representative of the Decedent, his father, CARL WEIDNER, brings this action 26 against Defendants, PRINCESS CRUISE LINES LTD. ("PRINCESS"), 27 CARNIVAL CORPORATION, and CARNIVAL PLC (collectively, 28 “CARNIVAL”) and allege: PLAINTIFF'S COMPLAINT FOR DAMAGES -1- CASE NO. _______________ Case 2:20-cv-04074 Document 1 Filed 05/04/20 Page 2 of 27 Page ID #:2 1 THE PARTIES 2 1. -
T1 Emails Received
Miller, Roger From: J & J Schroeder <[email protected]> Sent: Friday, March 06, 2020 5:07 PM To: Kesarwani, Rashi; Miller, Roger; T1 Cc: [email protected] Subject: Follow up question after 1600 block Curtis St. 3/5/20 meeting Hello Rashi, Roger and Andrew, Thank you very much for the time you gave us last night to discuss T1 Bond Phase 1 & 2 infrastructure improvement projects. You very patiently and attentively listened to our concerns, feedback and questions regarding the T1 Bond infrastructure improvement projects. I sincerely appreciate your diligence and efforts of outreach to the Berkeley community to make this T1 Phase 1 & 2 planning process transparent and accessible to the public for input. After speaking with my neighbors, we would like clarification regarding the email Director of Public Works Phil Harrington sent to Joan Hamilton and me on February 7, 2020. Mr. Harrington's email was in response to an email both Joan and I sent regarding the unsafe, degraded condition of the 1600 block of Curtis St. This is the email I sent 1/29/20: City of Berkeley Department of Public Works 2180 Milvia St. Berkeley, CA 94704 January 29, 2020 Department of Public Works Director Phil Harrington: I am here tonight to strongly urge the Department of Public Works to have the second phase of Measure T1 (infrastructure bond money) go towards paving more streets. I have lived at 1610 Curtis St. for the past 41 years. According to Beth Gerstein, District 1 Council member Rashi Kesarwani’s Legislative Aide, the 1600 block of Curtis St. -

NHS Knightlife April 9 2021 Edition
April 9, 2021 Vol. 59 No. 5 Image By Jaime Chen This Year’s Musical Huang, Liu, and Kim: It’s Time To Cancel At Newport: Theory of Advocating for Boys’ Hospital Playlist Daylight Savings Relativity Volleyball Page 20 Page 17 Page 8 Page 9 4333 Factoria Blvd. SE // Bellevue, WA // 98006 2 News April 9, 2021 APRIL - MAY SUNDAY MONDAY TUESDAY WEDNESDAY THURSDAY FRIDAY SATURDAY 4 5 6 7 8 9 10 Easter Sunday Easter Monday ASB Executive Board Election Week 2021 Virtual STEM Fair 11 12 13 14 15 16 17 Tax Day Spring Break 18 19 20 21 22 23 24 25 26 27 28 29 30 1 Springfest Spirit Week First Week of In-Person Hybrid Schedule 2 3 4 5 6 7 8 Cinco de Mayo Atlanta Shootings Shine Spotlight on Anti-Asian Hate Crimes “Nothing is off the table for our investigation,” said the past year, there was a 149% increase in hate KATHERINE CHANG Hampton when asked if the police were going to crimes against Asian Americans despite the Editor classify the shooting as a hate crime. decrease in overall hate crimes. Many of these Captain Jay Baker was originally the hate crimes stem primarily from false claims spokesperson for the case but was removed after pertaining to COVID-19 and China that spread The fight for racial equality has always been one intense criticism of his initial updates. Baker violence and harassment like wildfire throughout of America’s longest and most grueling struggles. seemed to amplify Long’s narrative by describing Asian communities. -
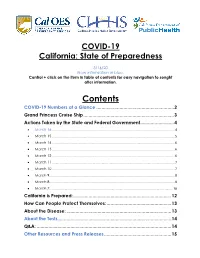
Contents for Easy Navigation to Sought After Information
COVID-19 California: State of Preparedness 3/16/20 New information in blue. Control + click on the item in table of contents for easy navigation to sought after information. Contents COVID-19 Numbers at a Glance ............................................................ 2 Grand Princess Cruise Ship ...................................................................... 3 Actions Taken by the State and Federal Government .......................... 4 • March 16, ........................................................................................................................................ 4 • March 15 ........................................................................................................................................ 5 • March 14 ........................................................................................................................................ 6 • March 13 ........................................................................................................................................ 6 • March 12 ........................................................................................................................................ 6 • March 11 ........................................................................................................................................ 7 • March 10 ........................................................................................................................................ 7 • March 9 .......................................................................................................................................... -
5446 Positives, 118 Deaths in State Who Gets Access to Experimental
PREPS: Bishop O’Dowd’s Marsalis Roberson is the Bay Area high school basketball player of the year. SPORTS Eat Drink Play: Wise Sons Deli in San Francisco serves up Passover recipes to celebrate at home. F1 24/7 COVERAGE: MERCURYNEWS.COM Volume 169, issue 284 $2.50 111 MARCH 29, 2020 CORONAVIRUS CORONAVIRUS THE DOCTOR WHO 5,446 ‘You’ve got your first positive’ positives, 118 deaths SHUT IT ALL DOWN in state Good news: Santa Clara County saw fewest new cases since March 20 By Emily DeRuy and Nico Savidge Staff writers California hit several grim milestones Saturday in the coro- navirus pandemic, surging past 5,000 positive cases and surpass- ing 100 deaths even as people re- mained sheltered at home in a desperate bid to stem the spread. Continuing a steady march up- ward over the weekend, the num- ber of positive COVID-19 cases in California reached 5,446 and deaths soared to 118 by the after- noon, according to data compiled by the Bay Area News Group. And, Gov. Gavin Newsom an- nounced during a visit to Sunny- vale earlier in the day, the number of people in intensive care beds across the state because of the vi- rus doubled overnight to 410 from 200 on Friday. Still, officials said they hoped the weekend’s rainy weather would prompt more people to re- main indoors and stick to Califor- nia’s shelter-in-place order, with social distancing being the best tool to fight COVID-19. Data compiled by this news organization showed there were 1,801 confirmed COVID-19 cases in the 10-county Bay Area as of Saturday afternoon, up from 1,648 on Friday, and 46 deaths, up from 36. -

Brochure Fincantieri CRUISE C-03-18 INTERNO.Indd
fincantieri / cruise ships _ cruise ships world class leisure C-03-18 - _ world-class leisure fincantieri.com fincantieri / cruise ships _ cruise ships world class leisure C-03-18 - _ world class leisure - seven seas, one company fincantieri.com Like a grand design in the stars, there Come il riflesso di un grande disegno is a global network of interconnected tracciato tra le stelle, c’è una rete globale knowledge and expertise, on sea and di connessioni del fare e del sapere, land, where day by day a group sul mare e sulla terra, lungo la quale is growing and adding fresh value all nasce e cresce un gruppo che aumenta, along the chain, creating a whole that is giorno dopo giorno, il valore di ogni so much greater than the sum of its parts. singolo elemento, in una somma This is Fincantieri. che è straordinariamente più grande A global Group that is a cutting-edge and delle sue parti. active player in all the highest added- Questa è Fincantieri. value market segments, across the water Un Gruppo globale, da sempre and around the world. all’avanguardia e protagonista in tutti i segmenti a più alto valore aggiunto, sul mare e nel mondo. fincantieri group the world in one design il mondo in un disegno — Twenty shipyards across Europe, Americas and — Venti cantieri tra Europa, Americhe e Asia. Asia. A workforce of more than twenty thousand peo- Ventimila persone al lavoro, il 60% delle quali ple, 60% abroad. Revenues of four billion euros. all’estero. Quattro miliardi di euro di ricavi. -

79667 FCCA Profiles
TableTable ofofContentsContents CARNIVAL CORPORATION Mark M. Kammerer, V.P., Worldwide Cruise Marketing . .43 Micky Arison, Chairman & CEO (FCCA Chairman) . .14 Stein Kruse, Senior V.P., Fleet Operations . .43 Giora Israel, V.P., Strategic Planning . .14 A. Kirk Lanterman, Chairman & CEO . .43 Francisco Nolla, V.P., Port Development . .15 Gregory J. MacGarva, Director, Procurement . .44 Matthew T. Sams, V.P., Caribbean Relations . .44 CARNIVAL CRUISE LINES Roger Blum, V.P., Cruise Programming . .15 NORWEGIAN CRUISE LINE Gordon Buck, Director, Port Operations. .16 Capt. Kaare Bakke, V.P. of Port Operations . .48 Amilicar “Mico” Cascais, Director, Tour Operations . .16 Sharon Dammar, Purchasing Manager, Food & Beverages . .48 Brendan Corrigan, Senior V.P., Cruise Operations . .16 Alvin Dennis, V.P., Purchasing & Logistics Bob Dickinson, President . .16 (FCCA Purchasing Committee Chairman) . .48 Vicki L. Freed, Senior V.P. of Sales & Marketing . .17 Colin Murphy, V.P, Land & Air Services . .48 Joe Lavi, Staff V.P. of Purchasing . .18 Joanne Salzedo, Manager, International Shore Programs . .49 David Mizer, V.P., Strategic Sourcing Global Source . .18 Andrew Stuart, Senior V.P., Marketing & Sales . .49 Francesco Morrello, Director, Port Development Group . .18 Colin Veitch, President & CEO . .49 Gardiner Nealon, Manager, Port Logistics . .19 Mary Sloan, Director, Risk Management . .19 PRINCESS CRUISES Terry L. Thornton, V.P., Marketing Planning Deanna Austin, V.P., Yield Management . .52 (FCCA Marketing Committee Chairman) . .19 Dean Brown, Executive V.P., Customer Service Capt. Domenico Tringale, V.P., Marine & Port Operations . .19 & Sales; Chairman & CEO of Princess Tours . .52 Jeffrey Danis, V.P., Global Purchasing & Logistics . .52 CELEBRITY CRUISES Graham Davis, Manager, Shore Operations, Caribbean and Atlantic . -

Tidal Wave of COVID-19 Lawsuits on the Way | Baker Donelson - Jdsupra
4/28/2020 Tidal Wave of COVID-19 Lawsuits on the Way | Baker Donelson - JDSupra April 22, 2020 Tidal Wave of COVID-19 Lawsuits on the Way Samuel Lanier Felker, Matthew Mulqueen Baker Donelson + Follow Contact As the "new normal" sinks in with social distancing and government-imposed shutdowns, some businesses are struggling to stay afloat. Now, many are about to be slammed with a tidal wave of litigation as consumers and injured parties seek compensation for COVID-related losses. A recent flurry of class action and other mass filings gives us a hint of what lies ahead – and they appear to be only the tip of the iceberg. This article will summarize the developing litigation landscape and provide guidance for businesses that may find themselves in the crosshairs. Consumer Class Actions In the past week or so there have been a host of consumer class actions filed against businesses that continued charging dues and membership fees even though their business operations substantially shut down or curtailed services because of the pandemic. Across the country, numerous suits alleging breach of contract and consumer protection violations have been filed against gyms and sporting clubs in particular. Jason Blank v. Youfit Health Clubs LLC, No. CACE2006161 (Broward Circuit, Fla.) involved allegations of deceptive trade practices when the defendant gym continued to charge the plaintiff and other members monthly gym fees despite its facilities being closed due to the novel coronavirus outbreak. See also Delvercchio v. Boston Sports Clubs, No. 20-cv-10666 (D. Mass.); Jampol v. Blink Holdings, No. 20-cv-02760 (S.D.N.Y.); and Namorato v. -

COMPLAINT For: 19 RONALD WONG; BENJAMIN 20 WONG, Individually; and the ESTATE 1
Case 2:20-cv-04727 Document 1 Filed 05/27/20 Page 1 of 34 Page ID #:1 1 NANCI E. NISHIMURA (SBN 152621) [email protected] 2 ALISON E. CORDOVA (SBN 284982) 3 [email protected] ANDREW L. KIRTLEY (SBN 328023) 4 [email protected] COTCHETT, PITRE & McCARTHY, LLP 5 840 Malcolm Road 6 Burlingame, California 94010 Telephone: (650) 697-6000 7 Facsimile: (650) 697-0577 8 KELLY W. WEIL (SBN 291398) P. TERRY ANDERLINI (SBN 44783) [email protected] 9 COTCHETT, PITRE & McCARTHY, LLP [email protected] 2716 Ocean Park Boulevard, Suite 3088 CAROLINE A. RIETZ (SBN 326412) 10 Santa Monica, CA 90405 [email protected] Telephone: (310) 392-2008 11 ANDERLINI & McSWEENEY LLP Facsimile: (310) 392-0111 66 Bovet Road, Suite 285 12 San Mateo, California 94402 Telephone: (650) 242-4884 13 Facsimile: (650) 212-0001 14 Attorneys for Plaintiffs 15 UNITED STATES DISTRICT COURT 16 CENTRAL DISTRICT OF CALIFORNIA 17 EVA YUK WAH MA WONG, CASE NO: 18 individually and as personal representative of the ESTATE OF COMPLAINT for: 19 RONALD WONG; BENJAMIN 20 WONG, individually; and the ESTATE 1. NEGLIGENCE – OF RONALD WONG, PERSONAL INJURIES AND 21 WRONGFUL DEATH 22 Plaintiffs, v. 2. SURVIVAL ACTION 23 24 CARNIVAL CORPORATION & PLC, DEMAND FOR JURY TRIAL a Bermuda Corporation; and PRINCESS 25 CRUISE LINES, LTD., a Bermuda 26 Corporation, 27 Defendants. 28 ♼ LAW OFFICES COTCHETT, PITRE & COMPLAINT MCCARTHY, LLP Case 2:20-cv-04727 Document 1 Filed 05/27/20 Page 2 of 34 Page ID #:2 1 TABLE CONTENTS 2 I. INTRODUCTION ............................................................................................ 1 3 II. THE PARTIES ................................................................................................ -

North American COVID-19 Policy Response Monitor: United States
North American COVID-19 Policy Response Monitor: United States December 23, 2020 What is the North American COVID-19 Policy Response Monitor? The North American COVID-19 policy monitor has been designed to collect and organize up-to-date information on how jurisdictions are responding to the crisis. It summarizes responses of health systems as well as wider public health initiatives. The North American policy monitor is an offshoot of the international COVID-19 Health System Response Monitor (HSRM), a joint undertaking of the WHO Regional Office for Europe, the European Commission and the European Observatory on Health Systems and Policies. Contents List of Acronyms and Abbreviations ............................................................................................................. 2 1. Preventing Transmission ........................................................................................................................... 3 2. Ensuring sufficient physical infrastructure and workforce capacity ....................................................... 12 3. Providing health services effectively....................................................................................................... 17 4. Paying for services .................................................................................................................................. 20 5. Governance ............................................................................................................................................. 23 6. Measures -

Framework for Conditional Sailing Order
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES (HHS) CENTERS FOR DISEASE CONTROL AND PREVENTION (CDC) ORDER UNDER SECTIONS 361 & 365 OF THE PUBLIC HEALTH SERVICE ACT (42 U.S.C. 264, 268) AND 42 CODE OF FEDERAL REGULATIONS PART 70 (INTERSTATE) AND PART 71 (FOREIGN): FRAMEWORK FOR CONDITIONAL SAILING AND INITIAL PHASE COVID-19 TESTING REQUIREMENTS FOR PROTECTION OF CREW Executive Summary The Centers for Disease Control and Prevention (CDC), a component of the U.S. Department of Health and Human Services (HHS), announces this framework for a phased resumption of cruise ship passenger operations. Considering the continued spread of COVID-19 worldwide and increased risk of COVID-19 on cruise ships, a careful approach is needed to safely resume cruise ship passenger operations. CDC is establishing requirements to mitigate the COVID-19 risk to passengers and crew, prevent the further spread of COVID-19 from cruise ships into U.S. communities, and protect public health and safety. After expiration of CDC’s No Sail Order (NSO) on October 31, 2020, CDC will take a phased approach to resuming cruise ship passenger operations in U.S. waters. The initial phases will consist of testing and additional safeguards for crew members. CDC will ensure cruise ship operators have adequate health and safety protections for crew 1 members while these cruise ship operators build the laboratory capacity needed to test future passengers. Subsequent phases will include simulated voyages to test cruise ship operators’ ability to mitigate COVID-19 risk, certification for ships that meet specific requirements, and a phased return to cruise ship passenger voyages in a manner that mitigates COVID-19 risk among passengers, crew members, and U.S.