NADPH Homeostasis in Cancer: Functions, Mechanisms and Therapeutic Implications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Regulation of Carbamoyl Phosphate Synthetase-Aspartate Transcarbamoylase-Dihydroorotase (Cad) by Phosphorylation and Protein-Protein Interactions
THE REGULATION OF CARBAMOYL PHOSPHATE SYNTHETASE-ASPARTATE TRANSCARBAMOYLASE-DIHYDROOROTASE (CAD) BY PHOSPHORYLATION AND PROTEIN-PROTEIN INTERACTIONS Eric M. Wauson A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Department of Pharmacology. Chapel Hill 2007 Approved by: Lee M. Graves, Ph.D. T. Kendall Harden, Ph.D. Gary L. Johnson, Ph.D. Aziz Sancar M.D., Ph.D. Beverly S. Mitchell, M.D. 2007 Eric M. Wauson ALL RIGHTS RESERVED ii ABSTRACT Eric M. Wauson: The Regulation of Carbamoyl Phosphate Synthetase-Aspartate Transcarbamoylase-Dihydroorotase (CAD) by Phosphorylation and Protein-Protein Interactions (Under the direction of Lee M. Graves, Ph.D.) Pyrimidines have many important roles in cellular physiology, as they are used in the formation of DNA, RNA, phospholipids, and pyrimidine sugars. The first rate- limiting step in the de novo pyrimidine synthesis pathway is catalyzed by the carbamoyl phosphate synthetase II (CPSase II) part of the multienzymatic complex Carbamoyl phosphate synthetase, Aspartate transcarbamoylase, Dihydroorotase (CAD). CAD gene induction is highly correlated to cell proliferation. Additionally, CAD is allosterically inhibited or activated by uridine triphosphate (UTP) or phosphoribosyl pyrophosphate (PRPP), respectively. The phosphorylation of CAD by PKA and ERK has been reported to modulate the response of CAD to allosteric modulators. While there has been much speculation on the identity of CAD phosphorylation sites, no definitive identification of in vivo CAD phosphorylation sites has been performed. Therefore, we sought to determine the specific CAD residues phosphorylated by ERK and PKA in intact cells. -

Sequence Variation in the Dihydrofolate Reductase-Thymidylate Synthase (DHFR-TS) and Trypanothione Reductase (TR) Genes of Trypanosoma Cruzi
Molecular & Biochemical Parasitology 121 (2002) 33Á/47 www.parasitology-online.com Sequence variation in the dihydrofolate reductase-thymidylate synthase (DHFR-TS) and trypanothione reductase (TR) genes of Trypanosoma cruzi Carlos A. Machado *, Francisco J. Ayala Department of Ecology and Evolutionary Biology, University of California, Irvine, CA 92697-2525, USA Received 15 November 2001; received in revised form 25 January 2002 Abstract Dihydrofolate reductase-thymidylate synthase (DHFR-TS) and trypanothione reductase (TR) are important enzymes for the metabolism of protozoan parasites from the family Trypanosomatidae (e.g. Trypanosoma spp., Leishmania spp.) that are targets of current drug-design studies. Very limited information exists on the levels of genetic polymorphism of these enzymes in natural populations of any trypanosomatid parasite. We present results of a survey of nucleotide variation in the genes coding for those enzymes in a large sample of strains from Trypanosoma cruzi, the agent of Chagas’ disease. We discuss the results from an evolutionary perspective. A sample of 31 strains show 39 silent and five amino acid polymorphisms in DHFR-TS, and 35 silent and 11 amino acid polymorphisms in TR. No amino acid replacements occur in regions that are important for the enzymatic activity of these proteins, but some polymorphisms occur in sites previously assumed to be invariant. The sequences from both genes cluster in four major groups, a result that is not fully consistent with the current classification of T. cruzi in two major groups of strains. Most polymorphisms correspond to fixed differences among the four sequence groups. Two tests of neutrality show that there is no evidence of adaptivedivergence or of selectiveevents having shaped the distribution of polymorphisms and fixed differences in these genes in T. -

View Eposter
Combined glucocorticoid and mineralocorticoid deficiency related to a new NNT mutation : a case report E.Doye 1, CL.Gay 1, S.Castets 1, F.Roucher-Boulez 2, Y.Morel 2, I.Plotton 2, M.Nicolino 1 1 CHU Hospices Civils de Lyon, Service d’Endocrinologie Pédiatrique, Lyon, France ; 2 Hospices Civils de Lyon, Laboratoire d’Endocrinologie Moléculaire et Maladies Rares, Lyon, France BACKGROUND OBJECTIVE Familial glucocorticoid deficiency is an autosomal recessive disorder To describe a new case of familial characterized by specific failure of adrenocortical glucocorticoid glucocorticoid deficiency with combined production in response to adrenocorticotropic hormone (ACTH). mineralocorticoid insufficiency and extra Mutations of the NNT (nicotinamide nucleotide transhydrogenase) adrenal manifestations. gene have recently been implicated in familial glucocorticoid deficiency. RESULTS Suffering from a febrile viral respiratory Diagnosis : during At one month At six months disease, an eight-month-old boy presented hypoglycémia and with status epilepticus caused by severe hypotension hypoglycemia. Multiple medical complications occurred, and invasive ventilation was Natremia (mmol/L) 135 126 136 required for 18 days. The results of blood tests performed during hypoglycemia revealed ACTH (ng/L) 1382 >2000 >2000 adrenal insufficiency. Renin and aldosterone Cortisol (nmol/L) <20 - <20 levels were high but considered consistent Renin (ng/L) 2880 278 177 with the mild hyponatremia and severe hypotension. Subsequent measurements Aldosterone (pmol/L) - 179 72 -

Mice Carrying a Human GLUD2 Gene Recapitulate Aspects of Human Transcriptome and Metabolome Development
Mice carrying a human GLUD2 gene recapitulate aspects of human transcriptome and metabolome development Qian Lia,b,1, Song Guoa,1, Xi Jianga, Jaroslaw Brykc,2, Ronald Naumannd, Wolfgang Enardc,3, Masaru Tomitae, Masahiro Sugimotoe, Philipp Khaitovicha,c,f,4, and Svante Pääboc,4 aChinese Academy of Sciences Key Laboratory of Computational Biology, Chinese Academy of Sciences-Max Planck Partner Institute for Computational Biology, Shanghai Institutes for Biological Sciences, Chinese Academy of Sciences, 200031 Shanghai, China; bUniversity of Chinese Academy of Sciences, 100049 Beijing, China; cMax Planck Institute for Evolutionary Anthropology, 04103 Leipzig, Germany; dMax Planck Institute of Molecular Cell Biology and Genetics, D-01307 Dresden, Germany; eInstitute for Advanced Biosciences, Keio University, 997-0035 Tsuruoka, Yamagata, Japan; and fSkolkovo Institute for Science and Technology, 143025 Skolkovo, Russia Edited by Joshua M. Akey, University of Washington, Seattle, WA, and accepted by the Editorial Board April 1, 2016 (received for review September 28, 2015) Whereas all mammals have one glutamate dehydrogenase gene metabolic flux from glucose and glutamine to lipids by way of the (GLUD1), humans and apes carry an additional gene (GLUD2), TCA cycle (12). which encodes an enzyme with distinct biochemical properties. To investigate the physiological role the GLUD2 gene may We inserted a bacterial artificial chromosome containing the human play in human and ape brains, we generated mice transgenic for GLUD2. GLUD2 gene into mice and analyzed the resulting changes in the a genomic region containing human We compared effects transcriptome and metabolome during postnatal brain development. on gene expression and metabolism during postnatal development Effects were most pronounced early postnatally, and predominantly of the frontal cortex of the brain in these mice and their wild-type genes involved in neuronal development were affected. -

Large Sex Differences in Chicken Behavior and Brain Gene Expression Coincide with Few Differences in Promoter DNA-Methylation
Large Sex Differences in Chicken Behavior and Brain Gene Expression Coincide with Few Differences in Promoter DNA-Methylation Daniel Na¨tt1,2*, Beatrix Agnvall1, Per Jensen1 1 IFM Biology, AVIAN Behaviour and Genomics group, Linko¨ping University, Linko¨ping, Sweden, 2 Department of Clinical and Experimental Medicine, Laboratory of Integrative and Behavioral Neuroscience, Linko¨ping University, Linko¨ping, Sweden Abstract While behavioral sex differences have repeatedly been reported across taxa, the underlying epigenetic mechanisms in the brain are mostly lacking. Birds have previously shown to have only limited dosage compensation, leading to high sex bias of Z-chromosome gene expression. In chickens, a male hyper-methylated region (MHM) on the Z-chromosome has been associated with a local type of dosage compensation, but a more detailed characterization of the avian methylome is limiting our interpretations. Here we report an analysis of genome wide sex differences in promoter DNA-methylation and gene expression in the brain of three weeks old chickens, and associated sex differences in behavior of Red Junglefowl (ancestor of domestic chickens). Combining DNA-methylation tiling arrays with gene expression microarrays we show that a specific locus of the MHM region, together with the promoter for the zinc finger RNA binding protein (ZFR) gene on chromosome 1, is strongly associated with sex dimorphism in gene expression. Except for this, we found few differences in promoter DNA-methylation, even though hundreds of genes were robustly differentially expressed across distantly related breeds. Several of the differentially expressed genes are known to affect behavior, and as suggested from their functional annotation, we found that female Red Junglefowl are more explorative and fearful in a range of tests performed throughout their lives. -

NNT Mutations: a Cause of Primary Adrenal Insufficiency, Oxidative Stress and Extra- Adrenal Defects
175:1 F Roucher-Boulez and others NNT, adrenal and extra-adrenal 175:1 73–84 Clinical Study defects NNT mutations: a cause of primary adrenal insufficiency, oxidative stress and extra- adrenal defects Florence Roucher-Boulez1,2, Delphine Mallet-Motak1, Dinane Samara-Boustani3, Houweyda Jilani1, Asmahane Ladjouze4, Pierre-François Souchon5, Dominique Simon6, Sylvie Nivot7, Claudine Heinrichs8, Maryline Ronze9, Xavier Bertagna10, Laure Groisne11, Bruno Leheup12, Catherine Naud-Saudreau13, Gilles Blondin13, Christine Lefevre14, Laetitia Lemarchand15 and Yves Morel1,2 1Molecular Endocrinology and Rare Diseases, Lyon University Hospital, Bron, France, 2Claude Bernard Lyon 1 University, Lyon, France, 3Pediatric Endocrinology, Gynecology and Diabetology, Necker University Hospital, Paris, France, 4Pediatric Department, Bab El Oued University Hospital, Alger, Algeria, 5Pediatric Endocrinology and Diabetology, American Memorial Hospital, Reims, France, 6Pediatric Endocrinology, Robert Debré Hospital, Paris, France, 7Department of Pediatrics, Rennes Teaching Hospital, Rennes, France, 8Pediatric Endocrinology, Queen Fabiola Children’s University Hospital, Brussels, Belgium, 9Endocrinology Department, L.-Hussel Hospital, Vienne, France, 10Endocrinology Department, Cochin University Hospital, Paris, France, 11Endocrinology Department, Lyon University Hospital, Bron-Lyon, France, 12Paediatric and Clinical Genetic Department, Correspondence Nancy University Hospital, Vandoeuvre les Nancy, France, 13Pediatric Endocrinology and Diabetology, should be -

Identification of Transcriptomic Differences Between Lower
International Journal of Molecular Sciences Article Identification of Transcriptomic Differences between Lower Extremities Arterial Disease, Abdominal Aortic Aneurysm and Chronic Venous Disease in Peripheral Blood Mononuclear Cells Specimens Daniel P. Zalewski 1,*,† , Karol P. Ruszel 2,†, Andrzej St˛epniewski 3, Dariusz Gałkowski 4, Jacek Bogucki 5 , Przemysław Kołodziej 6 , Jolanta Szyma ´nska 7 , Bartosz J. Płachno 8 , Tomasz Zubilewicz 9 , Marcin Feldo 9,‡ , Janusz Kocki 2,‡ and Anna Bogucka-Kocka 1,‡ 1 Chair and Department of Biology and Genetics, Medical University of Lublin, 4a Chod´zkiSt., 20-093 Lublin, Poland; [email protected] 2 Chair of Medical Genetics, Department of Clinical Genetics, Medical University of Lublin, 11 Radziwiłłowska St., 20-080 Lublin, Poland; [email protected] (K.P.R.); [email protected] (J.K.) 3 Ecotech Complex Analytical and Programme Centre for Advanced Environmentally Friendly Technologies, University of Marie Curie-Skłodowska, 39 Gł˛ebokaSt., 20-612 Lublin, Poland; [email protected] 4 Department of Pathology and Laboratory Medicine, Rutgers-Robert Wood Johnson Medical School, One Robert Wood Johnson Place, New Brunswick, NJ 08903-0019, USA; [email protected] 5 Chair and Department of Organic Chemistry, Medical University of Lublin, 4a Chod´zkiSt., Citation: Zalewski, D.P.; Ruszel, K.P.; 20-093 Lublin, Poland; [email protected] St˛epniewski,A.; Gałkowski, D.; 6 Laboratory of Diagnostic Parasitology, Chair and Department of Biology and Genetics, Medical University of Bogucki, J.; Kołodziej, P.; Szyma´nska, Lublin, 4a Chod´zkiSt., 20-093 Lublin, Poland; [email protected] J.; Płachno, B.J.; Zubilewicz, T.; Feldo, 7 Department of Integrated Paediatric Dentistry, Chair of Integrated Dentistry, Medical University of Lublin, M.; et al. -

Note: the Letters 'F' and 'T' Following the Locators Refers to Figures and Tables
Index Note: The letters ‘f’ and ‘t’ following the locators refers to figures and tables cited in the text. A Acyl-lipid desaturas, 455 AA, see Arachidonic acid (AA) Adenophostin A, 71, 72t aa, see Amino acid (aa) Adenosine 5-diphosphoribose, 65, 789 AACOCF3, see Arachidonyl trifluoromethyl Adlea, 651 ketone (AACOCF3) ADP, 4t, 10, 155, 597, 598f, 599, 602, 669, α1A-adrenoceptor antagonist prazosin, 711t, 814–815, 890 553 ADPKD, see Autosomal dominant polycystic aa 723–928 fragment, 19 kidney disease (ADPKD) aa 839–873 fragment, 17, 19 ADPKD-causing mutations Aβ, see Amyloid β-peptide (Aβ) PKD1 ABC protein, see ATP-binding cassette protein L4224P, 17 (ABC transporter) R4227X, 17 Abeele, F. V., 715 TRPP2 Abbott Laboratories, 645 E837X, 17 ACA, see N-(p-amylcinnamoyl)anthranilic R742X, 17 acid (ACA) R807X, 17 Acetaldehyde, 68t, 69 R872X, 17 Acetic acid-induced nociceptive response, ADPR, see ADP-ribose (ADPR) 50 ADP-ribose (ADPR), 99, 112–113, 113f, Acetylcholine-secreting sympathetic neuron, 380–382, 464, 534–536, 535f, 179 537f, 538, 711t, 712–713, Acetylsalicylic acid, 49t, 55 717, 770, 784, 789, 816–820, Acrolein, 67t, 69, 867, 971–972 885 Acrosome reaction, 125, 130, 301, 325, β-Adrenergic agonists, 740 578, 881–882, 885, 888–889, α2 Adrenoreceptor, 49t, 55, 188 891–895 Adult polycystic kidney disease (ADPKD), Actinopterigy, 223 1023 Activation gate, 485–486 Aframomum daniellii (aframodial), 46t, 52 Leu681, amino acid residue, 485–486 Aframomum melegueta (Melegueta pepper), Tyr671, ion pathway, 486 45t, 51, 70 Acute myeloid leukaemia and myelodysplastic Agelenopsis aperta (American funnel web syndrome (AML/MDS), 949 spider), 48t, 54 Acylated phloroglucinol hyperforin, 71 Agonist-dependent vasorelaxation, 378 Acylation, 96 Ahern, G. -
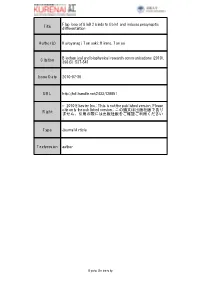
Title Flap Loop of Glud2 Binds to Cbln1 and Induces Presynaptic
Flap loop of GluD2 binds to Cbln1 and induces presynaptic Title differentiation Author(s) Kuroyanagi, Tomoaki; Hirano, Tomoo Biochemical and biophysical research communications (2010), Citation 398(3): 537-541 Issue Date 2010-07-30 URL http://hdl.handle.net/2433/128851 © 2010 Elsevier Inc.; This is not the published version. Please cite only the published version.; この論文は出版社版であり Right ません。引用の際には出版社版をご確認ご利用ください 。 Type Journal Article Textversion author Kyoto University Flap loop of GluD2 binds to Cbln1 and induces presynaptic differentiation Tomoaki Kuroyanagi and Tomoo Hirano Department of Biophysics, Graduate School of Science, Kyoto University, Kyoto 606-8502, Japan Department of Biophysics, Graduate School of Science, Kyoto University, Sakyo-ku, Kyoto 606-8502, Japan Correspondence should be addressed to: T. Hirano Tel, 81-75-753-4237 Fax, 81-75-753-4227 E-mail, [email protected] (Tomoaki Kuroyanagi); [email protected] (Tomoo Hirano) 1 Abstract Glutamate receptor δ2 (GluD2) is selectively expressed on the postsynaptic spines at parallel-fiber (PF)-Purkinje neuron (PN) synapses. GluD2 knockout mice show a reduced number of PF-PN synapses, suggesting that GluD2 is involved in synapse formation. Recent studies revealed that GluD2 induces presynaptic differentiation in a manner dependent on its N-terminal domain (NTD) through binding of Cbln1 secreted from cerebellar granule neurons. However, the underlying mechanism of the specific binding of the NTD to Cbln1 remains elusive. Here, we have identified the flap loop (Arg321-Trp339) in the NTD of GluD2 (GluD2-NTD) as a crucial region for the binding to Cbln1 and the induction of presynaptic differentiation. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase -

UC Irvine UC Irvine Previously Published Works
UC Irvine UC Irvine Previously Published Works Title The C57BL/6J Mouse Strain Background Modifies the Effect of a Mutation in Bcl2l2 Permalink https://escholarship.org/uc/item/5152r99k Journal G3-Genes|Genomes|Genetics, 2(1) ISSN 2160-1836 Authors Navarro, S. J Trinh, T. Lucas, C. A et al. Publication Date 2012-01-06 DOI 10.1534/g3.111.000778 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California INVESTIGATION The C57BL/6J Mouse Strain Background Modifies the Effect of a Mutation in Bcl2l2 Stefanie J. Navarro, Tuyen Trinh, Charlotte A. Lucas, Andrea J. Ross, Katrina G. Waymire, and Grant R. MacGregor1 Department of Developmental and Cell Biology, School of Biological Sciences, and Center for Molecular and Mitochondrial Medicine and Genetics, University of California Irvine, Irvine, California 92697-2300 ABSTRACT Bcl2l2 encodes BCL-W, an antiapoptotic member of the BCL-2 family of proteins. Intercross of KEYWORDS Bcl2l2 +/2 mice on a mixed C57BL/6J, 129S5 background produces Bcl2l2 2/2 animals with the expected –Nnt frequency. In contrast, intercross of Bcl2l2 +/2 mice on a congenic C57BL/6J background produces rela- mutation, genetic tively few live-born Bcl2l2 2/2 animals. Genetic modifiers alter the effect of a mutation. C57BL/6J mice modifier, BCL-W, (Mus musculus) have a mutant allele of nicotinamide nucleotide transhydrogenase (Nnt) that can act as apoptosis a modifier. Loss of NNT decreases the concentration of reduced nicotinamide adenine dinucleotide phos- phate within the mitochondrial matrix. Nicotinamide adenine dinucleotide phosphate is a cofactor for glutathione reductase, which regenerates reduced glutathione, an important antioxidant. -

Methotrexate Inhibits the First Committed Step of Purine
Biochem. J. (1999) 342, 143–152 (Printed in Great Britain) 143 Methotrexate inhibits the first committed step of purine biosynthesis in mitogen-stimulated human T-lymphocytes: a metabolic basis for efficacy in rheumatoid arthritis? Lynette D. FAIRBANKS*, Katarzyna RU$ CKEMANN*1, Ying QIU*2, Catherine M. HAWRYLOWICZ†, David F. RICHARDS†, Ramasamyiyer SWAMINATHAN‡, Bernhard KIRSCHBAUM§ and H. Anne SIMMONDS*3 *Purine Research Laboratory, 5th Floor Thomas Guy House, GKT Guy’s Hospital, London Bridge, London SE1 9RT, U.K., †Department of Respiratory Medicine and Allergy, 5th Floor Thomas Guy House, GKT Guy’s Hospital, London Bridge, London SE1 9RT, U.K., ‡Department of Chemical Pathology, GKT Guy’s Hospital, London Bridge, London SE1 9RT, U.K., and §DG Rheumatic/Autoimmune Diseases, Hoechst Marion Roussel, Deutschland GmbH, D-65926 Frankfurt am Main, Germany The immunosuppressive and anti-inflammatory effects of low- ribosyl-1-pyrophosphate (PP-ribose-P) as the molecular mech- dose methotrexate (MTX) have been related directly to inhibition anism underlying these disparate changes. These results provide of folate-dependent enzymes by polyglutamated derivatives, or the first substantive evidence that the immunosuppressive effects indirectly to adenosine release and\or apoptosis and clonal of low-dose MTX in primary blasting human T-lymphocytes deletion of activated peripheral blood lymphocytes in S-phase. In relate not to the inhibition of the two folate-dependent enzymes this study of phytohaemagglutinin-stimulated primary human T- of purine biosynthesis but to inhibition of the first enzyme, lymphocytes we show that MTX (20 nM to 20 µM) was cytostatic amidophosphoribosyltransferase, thereby elevating PP-ribose-P not cytotoxic, halting proliferation at G".