Assessing Normal and Abnormal Pregnancy from 4-10 Weeks
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

3 Embryology and Development
BIOL 6505 − INTRODUCTION TO FETAL MEDICINE 3. EMBRYOLOGY AND DEVELOPMENT Arlet G. Kurkchubasche, M.D. INTRODUCTION Embryology – the field of study that pertains to the developing organism/human Basic embryology –usually taught in the chronologic sequence of events. These events are the basis for understanding the congenital anomalies that we encounter in the fetus, and help explain the relationships to other organ system concerns. Below is a synopsis of some of the critical steps in embryogenesis from the anatomic rather than molecular basis. These concepts will be more intuitive and evident in conjunction with diagrams and animated sequences. This text is a synopsis of material provided in Langman’s Medical Embryology, 9th ed. First week – ovulation to fertilization to implantation Fertilization restores 1) the diploid number of chromosomes, 2) determines the chromosomal sex and 3) initiates cleavage. Cleavage of the fertilized ovum results in mitotic divisions generating blastomeres that form a 16-cell morula. The dense morula develops a central cavity and now forms the blastocyst, which restructures into 2 components. The inner cell mass forms the embryoblast and outer cell mass the trophoblast. Consequences for fetal management: Variances in cleavage, i.e. splitting of the zygote at various stages/locations - leads to monozygotic twinning with various relationships of the fetal membranes. Cleavage at later weeks will lead to conjoined twinning. Second week: the week of twos – marked by bilaminar germ disc formation. Commences with blastocyst partially embedded in endometrial stroma Trophoblast forms – 1) cytotrophoblast – mitotic cells that coalesce to form 2) syncytiotrophoblast – erodes into maternal tissues, forms lacunae which are critical to development of the uteroplacental circulation. -

Management of Patent Vitellointestinal Duct in Infants
Published online: 2021-02-17 94 OriginalPatent Vitellointestinal Article Duct Ghritlaharey Management of Patent Vitellointestinal Duct in Infants Rajendra K. Ghritlaharey1 1Department of Paediatric Surgery, Gandhi Medical College and Address for correspondence Rajendra K. Ghritlaharey, MS, MCh, Associated Kamla Nehru and Hamidia Hospital, Bhopal, Madhya FAIS, MAMS, DLitt, Department of Paediatric Surgery, Gandhi Medical Pradesh, India College and Associated Kamla Nehru and Hamidia Hospitals, Bhopal 462001, Madhya Pradesh, India (e-mail: [email protected]). Ann Natl Acad Med Sci (India) 2021;57:94–99. Abstract Objectives This study was undertaken to investigate and review the clinical presen- tation, surgical procedures executed, and the final outcome of infants managed for the patent vitellointestinal duct. Materials and Methods This is a single-institution, retrospective study and included infants who were operated for the patent vitellointestinal duct. This study was conducted at author’s Department of Paediatric Surgery during the last 20 years; from January 1, 2000 to December 31, 2019. Results A total of 24 infants were operated for the patent vitellointestinal duct during the study period and comprised 20 (83.3%) boys and 4 (16.6%) girls. The age of infants ranged from 7 days to 10 months, with a mean of 88.41 ± 64.9 days. Twenty-three (95.8%) infants were operated within 6 months of the age, 17 (70.8%) of them were operated within 3 months of the age. Only one (4.1%) infant was operated at the age of 10 months. Among 24 infants, 13 (54.1%) were presented with features suggestive of acute intestinal obstruction and remaining 11 (45.8%) were presented with fecal discharges through the umbilicus without intestinal obstruction. -

Extremely Rare Presentation of an Omphalomesenteric Cyst in a 61-Year-Old Patient
Turk J Surg 2017; 33: 43-44 Case Report DOI: 10.5152/UCD.2014.2748 Extremely rare presentation of an omphalomesenteric cyst in a 61-year-old patient Recep Aktimur1, Uğur Yaşar2, Elif Çolak1, Nuraydın Özlem1 ABSTRACT The umbilicus is remaining scar tissue from the umbilical cord in the fetus. If the omphalomesenteric duct in the umbilicus is not properly closed, an ileal-umbilical fistula, sinus formation, cysts, or, most commonly, Meckel’s di- verticulum can develop. The others are very rare and mostly occur in the pediatric population. We describe herein a 61-year-old female with a giant omphalomesenteric cyst presented as an asymptomatic infraumbilical mass. To our knowledge, this is the oldest patient reported and the largest cyst described in the literature. The diagnosis of a painless abdominal mass frequently suggests malignancy in older patients. But, extremely rare conditions can be detected, such as an omphalomesenteric cyst. Keywords: Adult, anomaly, cyst, duct, omphalomesenteric INTRODUCTION The umbilicus is remaining scar tissue from the umbilical cord in the fetus. It contains the urachus, om- phalomesenteric duct, and the round ligament’s embryonic remnants, which can be a source of many clinical problems. Also, umbilical hernia can occur in cases of closure defects of the umbilical ring. If the omphalomesenteric duct is not properly closed, an ileal-umbilical fistula, sinus formation, cysts, or Meckel’s diverticulum can develop. Meckel’s diverticulum is the most common omphalomesenteric duct anomaly, and it is also the most common congenital abnormality of the gastrointestinal tract (2%). Other anomalies associated with the omphalomesenteric duct are very rare and mostly occur in the pediatric population. -

Folding of Embryo
❑There is progressive increase in the size of the embryonic disc due to rapid growth of cells of central part of embryonic disc and rapid growth of somites. ❑ This causes conversion of flat pear-shaped germ disc into a cylindrical embryo. ❑The head and tail ends of the disc remain relatively close together.The increased length of the disc causes it to bulge upward into the amniotic cavity. ❑With the formation of the head and tail folds, parts of the yolk sac become enclosed within the embryo. ❑ In this way, a tube lined by endoderm is formed in the embryo. This is the primitive gut, from which most of the gastrointestinal tract is derived. ❑ At first, the gut is in wide communication with the yolk sac. The part of the gut cranial to this communication is called the foregut; the part caudal to the communication is called the hindgut; while the intervening part is called the midgut . ❑The communication with the yolk sac becomes progressively narrower. As a result of these changes, the yolk sac becomes small and inconspicuous, and is now termed the definitive yolk sac (also called the umbilical vesicle). ❑The narrow channel connecting it to the gut is called the vitellointestinal duct (also called vitelline duct; yolk stalk or omphalomesenteric duct). This duct becomes elongated and eventually disappears. ❑With the formation of the cavity, the embryo (along with the amniotic cavity and yolk sac) remains attached to the trophoblast only by extraembryonic mesoderm into which the coelom does not exist. This extraembryonic mesoderm forms the connecting stalk. -

Role of Ultrasound in the Evaluation of First-Trimester Pregnancies in the Acute Setting
University of Massachusetts Medical School eScholarship@UMMS Radiology Publications Radiology 2020-04-01 Role of ultrasound in the evaluation of first-trimester pregnancies in the acute setting Venkatesh A. Murugan University of Massachusetts Medical School Et al. Let us know how access to this document benefits ou.y Follow this and additional works at: https://escholarship.umassmed.edu/radiology_pubs Part of the Female Urogenital Diseases and Pregnancy Complications Commons, Obstetrics and Gynecology Commons, Radiology Commons, and the Women's Health Commons Repository Citation Murugan VA, Murphy BO, Dupuis CS, Goldstein AJ, Kim YH. (2020). Role of ultrasound in the evaluation of first-trimester pregnancies in the acute setting. Radiology Publications. https://doi.org/10.14366/ usg.19043. Retrieved from https://escholarship.umassmed.edu/radiology_pubs/526 Creative Commons License This work is licensed under a Creative Commons Attribution-Noncommercial 4.0 License This material is brought to you by eScholarship@UMMS. It has been accepted for inclusion in Radiology Publications by an authorized administrator of eScholarship@UMMS. For more information, please contact [email protected]. Role of ultrasound in the evaluation of first-trimester pregnancies in the acute setting Venkatesh A. Murugan, Bryan O’Sullivan Murphy, Carolyn Dupuis, Alan Goldstein, Young H. Kim PICTORIAL ESSAY Department of Radiology, University of Massachusetts Medical School, Worcester, MA, USA https://doi.org/10.14366/usg.19043 pISSN: 2288-5919 • eISSN: 2288-5943 Ultrasonography 2020;39:178-189 In patients presenting for an evaluation of pregnancy in the first trimester, transvaginal ultrasound is the modality of choice for establishing the presence of an intrauterine pregnancy; evaluating pregnancy viability, gestational age, and multiplicity; detecting pregnancy-related Received: July 25, 2019 complications; and diagnosing ectopic pregnancy. -
The Derivatives of Three-Layered Embryo (Germ Layers)
HUMANHUMAN EMBRYOLOGYEMBRYOLOGY Department of Histology and Embryology Jilin University ChapterChapter 22 GeneralGeneral EmbryologyEmbryology FourthFourth week:week: TheThe derivativesderivatives ofof trilaminartrilaminar germgerm discdisc Dorsal side of the germ disc. At the beginning of the third week of development, the ectodermal germ layer has the shape of a disc that is broader in the cephalic than the caudal region. Cross section shows formation of trilaminar germ disc Primitive pit Drawing of a sagittal section through a 17-day embryo. The most cranial portion of the definitive notochord has formed. ectoderm Schematic view showing the definitive notochord. horizon =ectoderm hillside fields =neural plate mountain peaks =neural folds Cave sinks into mountain =neural tube valley =neural groove 7.1 Derivatives of the Ectodermal Germ Layer 1) Formation of neural tube Notochord induces the overlying ectoderm to thicken and form the neural plate. Cross section Animation of formation of neural plate When notochord is forming, primitive streak is shorten. At meanwhile, neural plate is induced to form cephalic to caudal end, following formation of notochord. By the end of 3rd week, neural folds and neural groove are formed. Neural folds fuse in the midline, beginning in cervical region and Cross section proceeding cranially and caudally. Neural tube is formed & invade into the embryo body. A. Dorsal view of a human embryo at approximately day 22. B. Dorsal view of a human embryo at approximately day 23. The nervous system is in connection with the amniotic cavity through the cranial and caudal neuropores. Cranial/anterior neuropore Neural fold heart Neural groove endoderm caudal/posterior neuropore A. -
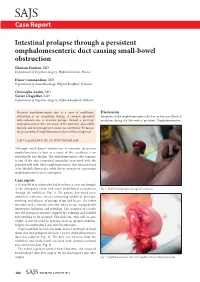
Intestinal Prolapse Through a Persistent Omphalomesenteric Duct
SAJS Case Report Intestinal prolapse through a persistent omphalomesenteric duct causing small-bowel obstruction Ghislain Pauleau, MD Department of Digestive Surgery, Hôpital Laveran, France Diane Commandeur, MD Department of Anaesthesiology, Hôpital Bouffard, Djibouti Christophe Andro, MD Xavier Chapellier, MD Department of Digestive Surgery, Hôpital Bouffard, Djibouti Persistent omphalomesenteric duct as a cause of small-bowel Discussion obstruction is an exceptional finding. A neonate presented Anomalies in the omphalomesenteric duct occur because of lack of with occlusion due to intestinal prolapse through a persistent involution during the 9th week of gestation. Omphalomesenteric omphalomesenteric duct. Remnants of the duct were successfully resected, and the postoperative course was uneventful. We discuss the presentation of omphalomesenteric duct and its management. S Afr J Surg 2012;50(3):102-103. DOI:7196/SAJS.1289 Although small-bowel obstruction is common, persistent omphalomesenteric duct as a cause of this condition is an exceptionally rare finding. The omphalomesenteric duct remnant is one of the rare congenital anomalies associated with the primitive yolk stalk. Most omphalomesenteric duct remnants tend to be Meckel’s diverticula, while the occurrence of a persistent omphalomesenteric duct is infrequent. Case report A 20-day-old male infant who had been born at term was brought to the emergency room with acute small-bowel evisceration Fig. 1. Small-bowel prolapse through the umbilicus. through the umbilicus (Fig. 1). His parents had noted peri- umbilical erythema, mucus-containing umbilical drainage, vomiting, and absence of passage of gas and faeces. The infant was taken to the intensive care unit, where he was managed with intravenous hydration and refeeding. -

What Is the Role of the Placenta—Does It Protect Against Or Is It a Target for Insult?
Teratology Primer, 3rd Edition www.teratology.org/primer What Is the Role of the Placenta—Does It Protect Against or Is It a Target for Insult? Richard K. Miller University of Rochester School of Medicine & Dentistry Rochester, New York The placenta is not just a barrier but has many functions that are vital to the health of the embryo/fetus. The placenta is the anchor, the conduit, and the controller of pregnancy—and it can also be a target for toxicant action. The placenta encompasses not only the chorioallantoic placenta but all of its extraembryonic membranes (chorion/amnion) and the yolk sac. (Figure 1). The placenta and its membranes secure the embryo and fetus to the decidua (uterine lining) and release a variety of steroid and protein hormones that characterize the physiology of the pregnant female. Figure 1. Placental Structure in the Mouse. Figures depict early development of the mouse conceptus at embryonic days (E3.5, E7.5, E12.5). In the fetus, the visceral yolk sac (vYS) inverts and remains active throughout the entire gestation providing for transfer of selective large molecules, e.g., immunoglobulins IgG and vitamin B12. Abbreviations: Al, allantois; Am, amnion; Ch, chorion; Dec, decidua; Emb, embryo; Epc, ectoplacental cone; ICM, inner cell mass; Lab, Labyrinth; pYS, parietal yolk sac; SpT, spongiotrophoblast; TCG, trophoblast giant cell; Umb Cord, umbilical cord; vYS, visceral yolk sac; C-TGC, maternal blood canal trophoblast giant cell; P-TGC, parietal trophoblast giant cell; S-TGC, sinusoidal trophoblast giant cell; SpA-TGC, Spiral artery-associated trophoblast giant cell; Cyan-trophectoderm and trophoblast lineage, Black- inner cell mass and embryonic ectoderm; Gray -endoderm, Red-maternal vasculature, Purple-mesoderm, Yellow- decidua, Pink-fetal blood vessels in labyrinth. -

Is Endometrial Scratching Beneficial for Patients Undergoing a Donor
diagnostics Article Is Endometrial Scratching Beneficial for Patients Undergoing a Donor-Egg Cycle with or without Previous Implantation Failures? Results of a Post-Hoc Analysis of an RCT Alexandra Izquierdo 1,*, Laura de la Fuente 2, Katharina Spies 3, David Lora 4,5 and Alberto Galindo 6 1 Gynaecology Unit, Médipôle Hôpital Mutualiste Lyon-Villeurbanne, 69100 Villeurbanne, France 2 Human Reproduction Unit, Department of Obstetrics and Gynaecology, University Hospital 12 de Octubre, Avda, Andalucia s/n, 28041 Madrid, Spain; [email protected] 3 ProcreaTec–IVF Spain, Manuel de Falla 6, 28036 Madrid, Spain; [email protected] 4 Clinical Research Unit (imas12-CIBERESP), University Hospital 12 de Octubre, Avda, Andalucia s/n, 28041 Madrid, Spain; [email protected] 5 Facultad de Estudios Estadísticos, Complutense University of Madrid, 28040 Madrid, Spain 6 Fetal Medicine Unit—Maternal and Child Health and Development Network (Red SAMIDRD12/0026/0016), Department of Obstetrics and Gynaecology, 12 de Octubre Research Institute (imas12), University Hospital 12 de Octubre, Complutense University of Madrid, Avda, Andalucia s/n, 28041 Madrid, Spain; [email protected] * Correspondence: [email protected] Abstract: Endometrial scratching (ES) has been proposed as a useful technique to improve outcomes in in vitro fertilization (IVF) cycles, particularly in patients with previous implantation failures. Our objective was to determine if patients undergoing egg-donor IVF cycles had better live birth rates Citation: Izquierdo, A.; de la Fuente, after ES, according to their previous implantation failures. Secondary outcomes were pregnancy L.; Spies, K.; Lora, D.; Galindo, A. Is rate, clinical pregnancy rate, ongoing pregnancy rate, miscarriage rate, and multiple pregnancy rate. -

Yolk Sac Diameter in Multiple Gestations
Case Studies Yolk Sac Diameter in Multiple Gestations Chelsea Fox, MD; Karenne Fru, MD, PhD; and Bruce A. Lessey, MD, PhD From the Department of OB/GYN, Greenville Health System, Greenville, SC (C.F., B.A.L.), University of South Carolina School of Medicine Greenville, Greenville, SC (B.A.L.), and Department of Obstet- rics and Gynecology, New Hanover Regional Medical Center, Wilmington, NC (K.F.) Abstract Enlargement of the yolk sacs is an ominous sign even in multi-gestational pregnancies. he yolk sac functions as the primary route ity conceived after placement of 2 embryos on of exchange between the embryo and post-retrieval day 3. Quantitative hCG levels were Tmother prior to the establishment of the higher than expected and transvaginal ultrasound placental circulation. It is well established that an at 6 weeks’ gestation demonstrated a triplet preg- abnormally large yolk sac serves as a prognostic nancy with a singleton sac and a separate mono- indicator for early pregnancy failure in singleton chorionic-monoamniotic versus conjoined twin gestation. However, no studies have been per- pregnancy with symmetrically enlarged yolk sacs, formed to describe normal versus abnormal yolk each with cardiac activity present (Figs. 1A and B). sac diameters (YSD) in multiple gestations. In this The yolk sacs associated with the twin pregnancy case, we describe a patient with triplet pregnancy were 6.15 mm and 7.37 mm, respectively, while the consisting of monochorionic-monoamniotic singleton had a normal yolk sac. A repeat ultra- twins both with enlarged yolk sacs in addition to sound 10 days later confirmed absence of fetal car- singleton pregnancy in a separate sac with a nor- diac activity in the monochorionic-monoamni- mal yolk sac. -

Human Embryologyembryology
HUMANHUMAN EMBRYOLOGYEMBRYOLOGY Department of Histology and Embryology Jilin University ChapterChapter 22 GeneralGeneral EmbryologyEmbryology DevelopmentDevelopment inin FetalFetal PeriodPeriod 8.1 Characteristics of Fetal Period 210 days, from week 9 to delivery. characteristics: maturation of tissues and organs rapid growth of the body During 3-5 month, fetal growth in length is 5cm/M. In last 2 month, weight increases in 700g/M. relative slowdown in growth of the head compared with the rest of the body 8.2 Fetal AGE Fertilization age lasts 266 days, from the moment of fertilization to the day when the fetal is delivered. menstrual age last 280 days, from the first day of the last menstruation before pregnancy to the day when the fetal is delivered. The formula of expected date of delivery: year +1, month -3, day+7. ChapterChapter 22 GeneralGeneral EmbryologyEmbryology FetalFetal membranesmembranes andand placentaplacenta Villous chorion placenta Decidua basalis Umbilical cord Afterbirth/ secundines Fusion of amnion, smooth chorion, Fetal decidua capsularis, membrane decidua parietalis 9.1 Fetal Membranes TheThe fetalfetal membranemembrane includesincludes chorionchorion,, amnion,amnion, yolkyolk sac,sac, allantoisallantois andand umbilicalumbilical cord,cord, originatingoriginating fromfrom blastula.blastula. TheyThey havehave functionsfunctions ofof protection,protection, nutrition,nutrition, respiration,respiration, excretion,excretion, andand producingproducing hormonehormone toto maintainmaintain thethe pregnancy.pregnancy. delivery 1) Chorion: villous and smooth chorion Villus chorionic plate primary villus trophoblast secondary villus extraembryonic tertiary villus mesoderm stem villus Amnion free villus decidua parietalis Free/termin al villus Stem/ancho chorion ring villus Villous chorion Smooth chorion Amniotic cavity Extraembyonic cavity disappears gradually; Amnion is added into chorionic plate; Villous and smooth chorion is formed. -

Embryology and Teratology in the Curricula of Healthcare Courses
ANATOMICAL EDUCATION Eur. J. Anat. 21 (1): 77-91 (2017) Embryology and Teratology in the Curricula of Healthcare Courses Bernard J. Moxham 1, Hana Brichova 2, Elpida Emmanouil-Nikoloussi 3, Andy R.M. Chirculescu 4 1Cardiff School of Biosciences, Cardiff University, Museum Avenue, Cardiff CF10 3AX, Wales, United Kingdom and Department of Anatomy, St. George’s University, St George, Grenada, 2First Faculty of Medicine, Institute of Histology and Embryology, Charles University Prague, Albertov 4, 128 01 Prague 2, Czech Republic and Second Medical Facul- ty, Institute of Histology and Embryology, Charles University Prague, V Úvalu 84, 150 00 Prague 5 , Czech Republic, 3The School of Medicine, European University Cyprus, 6 Diogenous str, 2404 Engomi, P.O.Box 22006, 1516 Nicosia, Cyprus , 4Department of Morphological Sciences, Division of Anatomy, Faculty of Medicine, C. Davila University, Bucharest, Romania SUMMARY Key words: Anatomy – Embryology – Education – Syllabus – Medical – Dental – Healthcare Significant changes are occurring worldwide in courses for healthcare studies, including medicine INTRODUCTION and dentistry. Critical evaluation of the place, tim- ing, and content of components that can be collec- Embryology is a sub-discipline of developmental tively grouped as the anatomical sciences has biology that relates to life before birth. Teratology however yet to be adequately undertaken. Surveys (τέρατος (teratos) meaning ‘monster’ or ‘marvel’) of teaching hours for embryology in US and UK relates to abnormal development and congenital medical courses clearly demonstrate that a dra- abnormalities (i.e. morphofunctional impairments). matic decline in the importance of the subject is in Embryological studies are concerned essentially progress, in terms of both a decrease in the num- with the laws and mechanisms associated with ber of hours allocated within the medical course normal development (ontogenesis) from the stage and in relation to changes in pedagogic methodol- of the ovum until parturition and the end of intra- ogies.