Pharmacotherapy Handbook, 7Th Edition
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Betamethasone Valerate Foam: a Look at the Clinical Data
Review: Clinical Trial Outcomes Betamethasone valerate foam: a look at the clinical data Clin. Invest. (2014) 4(3), 259–267 Topical corticosteroids and especially betamethasone valerate (BMV) have Avner Shemer1, Nicole Sakka1 & been used topically to relieve many inflammatory skin conditions such as Dov Tamarkin*2 psoriasis and atopic dermatitis. The vehicle used to deliver topical drugs 1Department of Dermatology, the Chaim Sheba Medical Center, Affiliated with the can influence the performance of these topical applications. BMV has Tel-Aviv University, Sackler School of Medicine, traditionally been available in creams, ointments, lotions and sprays. In Tel Hashomer, Israel the early 2000s, a topical hydroethanolic BMV foam became commercially 2Foamix Ltd., 2 Holzman Street, Weizmann available. Subsequently, alcohol-free emulsion- and petrolatum-based Science Park, Rehovot 76704, Israel foam formulations were also developed. This manuscript reviews the *Author for correspondence: Tel.: +972 52 457 5677 properties of BMV foams and clinical studies that have been conducted Fax: +972 8 853 1102 to assess their efficacy and safety as treatments for scalp and non-scalp [email protected] psoriasis, as well as other dermatological inflammatory conditions. Keywords: betamethasone valerate • foam • psoriasis • topical corticosteroids Topical corticosteroids have been ranked in four groups consisting of seven classes ranging from ultra-high potency preparations (class 1) to low-potency prepara- tions (class 7). Betamethasone valerate (BMV) is a mid-potency corticosteroid (class 3–5, depending on the dosage form), used topically to relieve inflammatory skin conditions. It is used as a treatment for psoriasis, atopic dermatitis and other corticosteroid-responsive dermatoses. The vehicle used to deliver topical drugs can influence the performance of these drugs. -

Albany-Molecular-Research-Regulatory
PRODUCT CATALOGUE API COMMERCIAL US EU Japan US EU Japan API Name Site CEP India API Name Site CEP India DMF DMF DMF DMF DMF DMF A Abiraterone Malta • Benztropine Mesylate Cedarburg • Adenosine Rozzano - Quinto de' Stampi • • * Betaine Citrate Anhydrous Bon Encontre • Betametasone-17,21- Alcaftadine Spain Spain • • Dipropionate Sterile • Alclometasone-17, 21- Spain Betamethasone Acetate Spain Dipropionate • • Altrenogest Spain • • Betamethasone Base Spain Amphetamine Aspartate Rensselaer Betamethasone Benzoate Spain * Monohydrate Milled • Betamethasone Valerate Amphetamine Sulfate Rensselaer Spain * • Acetate Betamethasone-17,21- Argatroban Rozzano - Quinto de' Stampi Spain • • Dipropionate • • • Atenolol India • • Betamethasone-17-Valerate Spain • • Betamethasone-21- Atracurium Besylate Rozzano - Quinto de' Stampi Spain • Phosphate Disodium Salt • • Bromfenac Monosodium Atropine Sulfate Cedarburg Lodi * • Salt Sesquihydrate • • Azanidazole Lodi Bromocriptine Mesylate Rozzano - Quinto de' Stampi • • • • • Azelastine HCl Rozzano - Quinto de' Stampi • • Budesonide Spain • • Aztreonam Rozzano - Valle Ambrosia • • Budesonide Sterile Spain • • B Bamifylline HCl Bon Encontre • Butorphanol Tartrate Cedarburg • Beclomethasone-17, 21- Spain Capecitabine Lodi Dipropionate • C • 2 *Please contact our Accounts Managers in case you are interested in this API. 3 PRODUCT CATALOGUE API COMMERCIAL US EU Japan US EU Japan API Name Site CEP India API Name Site CEP India DMF DMF DMF DMF DMF DMF Dexamethasone-17,21- Carbimazole Bon Encontre Spain • Dipropionate -

(12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 De Juan Et Al
US 200601 10428A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2006/0110428A1 de Juan et al. (43) Pub. Date: May 25, 2006 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA (US); A6F 2/00 (2006.01) Signe E. Varner, Los Angeles, CA (52) U.S. Cl. .............................................................. 424/427 (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Correspondence Address: Featured is a method for instilling one or more bioactive SCOTT PRIBNOW agents into ocular tissue within an eye of a patient for the Kagan Binder, PLLC treatment of an ocular condition, the method comprising Suite 200 concurrently using at least two of the following bioactive 221 Main Street North agent delivery methods (A)-(C): Stillwater, MN 55082 (US) (A) implanting a Sustained release delivery device com (21) Appl. No.: 11/175,850 prising one or more bioactive agents in a posterior region of the eye so that it delivers the one or more (22) Filed: Jul. 5, 2005 bioactive agents into the vitreous humor of the eye; (B) instilling (e.g., injecting or implanting) one or more Related U.S. Application Data bioactive agents Subretinally; and (60) Provisional application No. 60/585,236, filed on Jul. (C) instilling (e.g., injecting or delivering by ocular ion 2, 2004. Provisional application No. 60/669,701, filed tophoresis) one or more bioactive agents into the Vit on Apr. 8, 2005. reous humor of the eye. Patent Application Publication May 25, 2006 Sheet 1 of 22 US 2006/0110428A1 R 2 2 C.6 Fig. -
Vs VANCOMYCIN 125 Mg PO QID X10 DAYS PER PROTOCOL ANALYSIS P=NS
CLOSTRIDIUM DIFFICILE UPDATE: A JOINT VENTURE AMERICAN COLLEGE OF OSTEOPATHIC INTERNISTS CLINICAL CHALLENGES IN INPATIENT CARE MATTHEW BECHTOLD MD, FACP, FASGE, FACG, AGAF DIVISION OF GASTROENTEROLOGY UNIVERSITY OF MISSOURI – COLUMBIA MARCH 25, 2017 DISCLOSURE AMERICAN COLLEGE OF OSTEOPATHIC INTERNISTS NATIONAL MEETING Nestle Nutrition Institute Speaker & Consultant I will not discuss off label use or investigational use in my presentation Matthew Bechtold MD [email protected] QUESTIONS What is the burden of This is a crappy C. difficile? topic What are the C. It’s a dirty job but difficile treatment someone has to do it recommendations? How do we treat This should be severe C. difficile? stimulating C. DIFFICILE BACKGROUND ANAEROBIC GRAM + BACILLUS SPORE-FORMING TOXIN-PRODUCING FIRST DESCRIBED IN 1935 PATHOGENIC ROLE DESCRIBED IN 1970’s SPORE FORM VEGETATIVE FORM OUTSIDE COLON INSIDE COLON RESISTENT TO HEAT, ACID, TOXIN-PRODUCING ANTIBIOTICS SUSCEPTIBLE TO ANTIBIOTICS Hall IC, et al. Am J Dis Child 1935 Bartlett JG. Ann Intern Med 2006 Bartlett JG, et al. Gastroenterology 1978 C. DIFFICILE BACKGROUND ANTIBIOTIC THERAPY DISRUPTION OF COLONIC MICROFLORA C. DIFFICILE EXPOSURE AND COLONIZATION RELEASE OF TOXIN A (ENTEROTOXIN) & TOXIN B (CYTOTOXIN) MUCOSAL INJURY & INFLAMMATION LaMont JT, et al. UptoDate 2014 C. DIFFICILE BACKGROUND J-STRAIN 1989-1992 RESISTENT TO CLINDAMYCIN NAP1/BI/027 STRAIN NORTH AMERICAN PULSED- 2003-2006 FIELD TYPE 1 RESTRICTION ENZYME MORE SEVERE, REFRACTORY, RELAPSE ANALYSIS TYPE BI PCR RIBOTYPE 027 INCREASED TOXIN PRODUCTION MAY BE DUE TO FLUOROQUINOLONES 078 STRAIN SINCE 2005 SIMILAR TO 027 YOUNGER Miller M, et al. Clin Infect Dis 2010 COMMUNITY-ASSOCIATED Pepcin J, et al. -

Acute Diarrhea in Adults WENDY BARR, MD, MPH, MSCE, and ANDREW SMITH, MD Lawrence Family Medicine Residency, Lawrence, Massachusetts
Acute Diarrhea in Adults WENDY BARR, MD, MPH, MSCE, and ANDREW SMITH, MD Lawrence Family Medicine Residency, Lawrence, Massachusetts Acute diarrhea in adults is a common problem encountered by family physicians. The most common etiology is viral gastroenteritis, a self-limited disease. Increases in travel, comorbidities, and foodborne illness lead to more bacteria- related cases of acute diarrhea. A history and physical examination evaluating for risk factors and signs of inflammatory diarrhea and/or severe dehydration can direct any needed testing and treatment. Most patients do not require labora- tory workup, and routine stool cultures are not recommended. Treatment focuses on preventing and treating dehydra- tion. Diagnostic investigation should be reserved for patients with severe dehydration or illness, persistent fever, bloody stool, or immunosuppression, and for cases of suspected nosocomial infection or outbreak. Oral rehydration therapy with early refeeding is the preferred treatment for dehydration. Antimotility agents should be avoided in patients with bloody diarrhea, but loperamide/simethicone may improve symptoms in patients with watery diarrhea. Probiotic use may shorten the duration of illness. When used appropriately, antibiotics are effective in the treatment of shigellosis, campylobacteriosis, Clostridium difficile,traveler’s diarrhea, and protozoal infections. Prevention of acute diarrhea is promoted through adequate hand washing, safe food preparation, access to clean water, and vaccinations. (Am Fam Physician. 2014;89(3):180-189. Copyright © 2014 American Academy of Family Physicians.) CME This clinical content cute diarrhea is defined as stool with compares noninflammatory and inflamma- conforms to AAFP criteria increased water content, volume, or tory acute infectious diarrhea.7,8 for continuing medical education (CME). -

New Drug Evaluation Monograph Template
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Class Review: Antidiarrheals Date of Review: January 2017 Purpose for Class Review: To identify appropriate utilization management strategies for drugs used to treat diarrhea. Research Questions: 1. What is the comparative efficacy and effectiveness for bismuth subsalicylate, loperamide, diphenoxylate/atropine, paregoric, crofelemer, or opium tincture in management of diarrhea? 2. What are the comparative harms or potential abuses for bismuth subsalicylate, loperamide, diphenoxylate/atropine, paregoric, crofelemer, or opium tincture? 3. Are there subgroups of patients based on demographics (age, racial or ethnic groups and gender), other medications, or co-morbidities for which one treatment for diarrhea is more effective or associated with fewer adverse events? Conclusions: There is insufficient comparative evidence of efficacy and effectiveness between bismuth subsalicylate, loperamide, diphenoxylate/atropine, paregoric, crofelemer and opium tincture. Moderate quality evidence shows that the addition of loperamide to ciprofloxacin for treatment of traveler’s diarrhea may decrease the duration of diarrhea within the first 24 to 48 hours of symptom onset.1 Opium tincture has not been evaluated by the United States Food and Drug Administration (FDA) for safety and effectiveness because it was marketed before 1962.2 The FDA -

Improved Penetrating Topical Pharmaceutical Compositions Containing Corticosteroids
Europaisches Patentamt ® European Patent Office © Publication number: 0 129 283 Office europeen des brevets A2 © EUROPEAN PATENT APPLICATION © Application number: 84200821.1 ©Int CI.3: A 61 K 31/57 A 61 K 47/00, A 61 K 9/06 © Date of filing: 12.06.84 © Priority: 21.06.83 US 506274 © Applicant: THE PROCTER & GAMBLE COMPANY 01.02.84 US 576065 301 East Sixth Street Cincinnati Ohio 45201 (US) © Date of publication of application: © Inventor: Cooper, Eugene Rex 27.12.84 Bulletin 84/52 2425 Ambassador Drive Cincinnati, OH 45231 (US) © Designated Contracting States: BE CH DE FR GB IT Li NL SE © Inventor: Loomans, Maurice Edward 5231 Jessup Road Cincinnati, OH 45239IUS) © Inventor: Fawzi, Mahdi Bakir 11 Timberline Drive Flanders New Jersey 07836(US) © Representative: Suslic, Lydia et al, Procter & Gamble European Technical Center Temselaan 100 B-1820 Strombeek-Bever(BE) © Improved penetrating topical pharmaceutical compositions containing corticosteroids. Topical pharmaceutical compositions containing a cor- ticosteroid component and a penetration-enhancing vehicle are disclosed. The vehicle comprises a binary combination of a C3-C4 diol and a "cell-envelope disordering compound". The vehicle provides marked transepidermal and percutaneous delivery of corticosteroids. A method of treating certain rheumatic and inflammatory conditions, systemically or loc- ally, is also disclosed. TECHNICAL FIELD The present invention relates to topical compositions effective in delivering high levels of certain pharmaceutically-active cor- ticosteroid agents through the integument. Because of the ease of access, dynamics of application, large surface area, vast exposure to the circulatory and lymphatic networks, and non-invasive nature of the treatment, the delivery of pharmaceutically-active agents through the skin has long been a promising concept. -

AMRI India Pvt
WE’VE GOT API DEVELOPMENT AND MANUFACTURING DOWN TO AN EXACT SCIENCE API Commercial Product Catalogue PRODUCT CATALOGUE API Commercial US EU Japan US EU Japan API Name Site CEP India China API Name Site CEP India China DMF DMF DMF DMF DMF DMF Rozzano Quinto de Adenosine Betaine Citrate Anhydrous Bon Encontre, France A Stampi, Italy • Betametasone-17,21- Alcaftadine Valladolid, Spain Valladolid, Spain • Dipropionate Sterile • Alclometasone-17,21- Valladolid, Spain Betamethasone Acetate Valladolid, Spain Dipropionate • • • Altrenogest Valladolid, Spain • • Betamethasone Base Valladolid, Spain Aminobisamide HCl Rensselaer, US Betamethasone Benzoate Valladolid, Spain Amphetamine Aspartate Betamethasone Valerate Rensselaer, US Valladolid, Spain Monohydrate Milled • Acetate Betamethasone-17,21- Amphetamine Sulfate Rensselaer, US Valladolid, Spain • Dipropionate • • • • Rozzano Quinto de Argatroban Betamethasone-17-Valerate Valladolid, Spain Stampi, Italy • • • • Betamethasone-21- Atenolol Aurangabad, India Valladolid, Spain • • • Phosphate Disodium Salt • • Rozzano Quinto de Bromfenac Monosodium Atracurium Besylate Lodi, Italy Stampi, Italy • Salt Sesquihydrate • • Rozzano Quinto de Atropine Sulfate Grafton, US Bromocriptine Mesylate • Stampi, Italy • • • Rozzano Quinto de Azelastine HCl Budesonide Valladolid, Spain Stampi, Italy • • • • • Rozzano Valleambrosia, Aztreonam (not sterile) Budesonide Sterile Valladolid, Spain Italy • • • • B Bamifylline HCl Bon Encontre, France • C Capecitabine Lodi, Italy • • Beclomethasone-17,21- Valladolid, Spain -

(12) Patent Application Publication (10) Pub. No.: US 2011/0159073 A1 De Juan Et Al
US 20110159073A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2011/0159073 A1 de Juan et al. (43) Pub. Date: Jun. 30, 2011 (54) METHODS AND DEVICES FOR THE Publication Classification TREATMENT OF OCULAR CONDITIONS (51) Int. Cl. (76) Inventors: Eugene de Juan, LaCanada, CA A6F 2/00 (2006.01) (US); Signe E. Varner, Los (52) U.S. Cl. ........................................................ 424/427 Angeles, CA (US); Laurie R. Lawin, New Brighton, MN (US) (57) ABSTRACT Featured is a method for instilling one or more bioactive (21) Appl. No.: 12/981,038 agents into ocular tissue within an eye of a patient for the treatment of an ocular condition, the method comprising con (22) Filed: Dec. 29, 2010 currently using at least two of the following bioactive agent delivery methods (A)-(C): (A) implanting a Sustained release Related U.S. Application Data delivery device comprising one or more bioactive agents in a (63) Continuation of application No. 1 1/175,850, filed on posterior region of the eye so that it delivers the one or more Jul. 5, 2005, now abandoned. bioactive agents into the vitreous humor of the eye; (B) instill ing (e.g., injecting or implanting) one or more bioactive (60) Provisional application No. 60/585,236, filed on Jul. 2, agents Subretinally; and (C) instilling (e.g., injecting or deliv 2004, provisional application No. 60/669,701, filed on ering by ocular iontophoresis) one or more bioactive agents Apr. 8, 2005. into the vitreous humor of the eye. Patent Application Publication Jun. 30, 2011 Sheet 1 of 22 US 2011/O159073 A1 Patent Application Publication Jun. -

Recent Patents on Inflammation & Allergy Drug Discovery
Send Orders for Reprints to [email protected] 38 Recent Patents on Inflammation & Allergy Drug Discovery 2019, 13, 38-48 REVIEW ARTICLE ISSN: 1872-213X eISSN: 2212-2710 Inflammation & Allergy Drug Discovery Travelers’ Diarrhea: A Clinical Review Alexander K.C. Leung1,*, Amy A.M. Leung2, Alex H.C. Wong3 and Kam L. Hon4 1Department of Pediatrics, The University of Calgary, Alberta Children’s Hospital, Calgary, Alberta, Canada; 2Department of Family Medicine, The University of Alberta, Edmonton, Alberta, Canada; 3Department of Family Medi- cine, The University of Calgary, Calgary, Alberta, Canada; 4Department of Paediatrics, The Chinese University of Hong Kong, Shatin, Hong Kong Abstract: Background: Travelers’ diarrhea is the most common travel-related malady. It affects mil- lions of international travelers to developing countries annually and can significantly disrupt travel plans. Objective: To provide an update on the evaluation, diagnosis, treatment, and prevention of traveler’s diarrhea. Methods: A PubMed search was completed in Clinical Queries using the key term “traveler’s diarrhea”. The search strategy included meta-analyses, randomized controlled trials, clinical trials, observational studies, and reviews. The search was restricted to English literature. Patents were searched using the key term “traveler’s diarrhea” from www.freepatentsonline.com. Results: Between 10% and 40% of travelers develop diarrhea. The attack rate is highest for travelers A R T I C L E H I S T O R Y from a developed country who visit a developing country. Children are at particular risk. Travelers’ diarrhea is usually acquired through ingestion of food and water contaminated by feces. Most cases are Received: November 22, 2018 due to a bacterial pathogen, commonly, Escherichia coli, and occur within the first few days after arri- Revised: April 30, 2019 Accepted: May 10, 2019 val in a foreign country. -
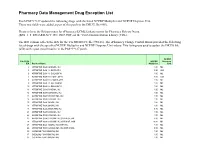
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

1 Topical Corticosteroids in Children
Pediatric Pharmacotherapy A Monthly Review for Health Care Professionals of the Children's Medical Center Volume 2, Number 1, January 1996 Topical Corticosteroid Preparations • Overview • Comparing Potencies o very high potency o high potency o moderate potency o low potency • Selecting a Vehicle • Evaluating Toxicity • Combination Products • Instructions for Parents • References Pharmacology Literature Reviews • Placental Drug Transfer • Antiepileptic Pharmacokinetics • Gentamicin in Children with Cancer Formularly Update Nearly fifty years ago the first topical corticosteroid preparation, hydrocortisone, was introduced in the United States, making a dramatic impact on the management of pediatric dermatologic conditions. Since that time, a wide spectrum of products has been developed in an effort to maximize anti -inflammatory properties while minimizing mineralocorticoid activity and adverse effects. Topical corticosteroid preparations have become a cornerstone in the treatment of children with a variety of skin conditions, including atopic dermatitis, psoriasis, eczema, seborrheic dermatitis, contact dermatitis, and some types of burns. They are useful adjunctive therapy in other dermatologic conditions, such as porphyria, lupus, epidermolysis bullosa, and severe cases of diaper dermatitis in infants.1 This brief review will focus on issues related to potency and drug selection, differences in vehicles, toxicities, and the use of combination corticosteroid products.2-5 Comparing Potency The most common method for comparing topical corticosteroid products is relat ive potency. Potency is determined by the degree of tissue penetration of a product (bioavailability) and the resulting vasoconstriction (skin -blanching) that is produced. It may not be relevant to efficacy in treating specific skin conditions. Testing to determine potency is conducted by pharmaceutical manufacturers and reflects a particular name brand product.