Fat, Obesity, Epidemics, and America's Children A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Excesss Karaoke Master by Artist
XS Master by ARTIST Artist Song Title Artist Song Title (hed) Planet Earth Bartender TOOTIMETOOTIMETOOTIM ? & The Mysterians 96 Tears E 10 Years Beautiful UGH! Wasteland 1999 Man United Squad Lift It High (All About 10,000 Maniacs Candy Everybody Wants Belief) More Than This 2 Chainz Bigger Than You (feat. Drake & Quavo) [clean] Trouble Me I'm Different 100 Proof Aged In Soul Somebody's Been Sleeping I'm Different (explicit) 10cc Donna 2 Chainz & Chris Brown Countdown Dreadlock Holiday 2 Chainz & Kendrick Fuckin' Problems I'm Mandy Fly Me Lamar I'm Not In Love 2 Chainz & Pharrell Feds Watching (explicit) Rubber Bullets 2 Chainz feat Drake No Lie (explicit) Things We Do For Love, 2 Chainz feat Kanye West Birthday Song (explicit) The 2 Evisa Oh La La La Wall Street Shuffle 2 Live Crew Do Wah Diddy Diddy 112 Dance With Me Me So Horny It's Over Now We Want Some Pussy Peaches & Cream 2 Pac California Love U Already Know Changes 112 feat Mase Puff Daddy Only You & Notorious B.I.G. Dear Mama 12 Gauge Dunkie Butt I Get Around 12 Stones We Are One Thugz Mansion 1910 Fruitgum Co. Simon Says Until The End Of Time 1975, The Chocolate 2 Pistols & Ray J You Know Me City, The 2 Pistols & T-Pain & Tay She Got It Dizm Girls (clean) 2 Unlimited No Limits If You're Too Shy (Let Me Know) 20 Fingers Short Dick Man If You're Too Shy (Let Me 21 Savage & Offset &Metro Ghostface Killers Know) Boomin & Travis Scott It's Not Living (If It's Not 21st Century Girls 21st Century Girls With You 2am Club Too Fucked Up To Call It's Not Living (If It's Not 2AM Club Not -

Food in Prison: an Eighth Amendment Violation Or Permissible Punishment?
University of South Dakota USD RED Honors Thesis Theses, Dissertations, and Student Projects Spring 2020 Food In Prison: An Eighth Amendment Violation or Permissible Punishment? Natasha M. Clark University of South Dakota Follow this and additional works at: https://red.library.usd.edu/honors-thesis Part of the Courts Commons, Food and Drug Law Commons, Human Rights Law Commons, and the Legal Ethics and Professional Responsibility Commons Recommended Citation Clark, Natasha M., "Food In Prison: An Eighth Amendment Violation or Permissible Punishment?" (2020). Honors Thesis. 109. https://red.library.usd.edu/honors-thesis/109 This Honors Thesis is brought to you for free and open access by the Theses, Dissertations, and Student Projects at USD RED. It has been accepted for inclusion in Honors Thesis by an authorized administrator of USD RED. For more information, please contact [email protected]. FOOD IN PRISON: AN EIGHTH AMENDMENT VIOLATION OR PERMISSIBLE PUNISHMENT? By Natasha Clark A Thesis Submitted in Partial Fulfillment Of the Requirements for the University Honors Program Department of Criminal Justice The University of South Dakota Graduation May 2020 The members of the Honors Thesis Committee appointed to examine the thesis of Natasha Clark find it satisfactory and recommend that it be accepted. Professor Sandy McKeown Associate Professor of Criminal Justice Director of the Committee Professor Thomas Horton Professor & Heidepriem Trial Advocacy Fellow Dr. Thomas Mrozla Assistant Professor of Criminal Justice ii ABSTRACT FOOD IN PRISON: AN EIGHTH AMENDMENT VIOLATION OR PERMISSIBLE PUNISHMENT? Natasha Clark Director: Prof. Sandy McKeown, Associate Professor of Criminal Justice This piece analyzes aspects such as; Eighth Amendment provisions, penology, case law, privatization and monopoly, and food law, that play into the constitutionality of privatized prisons using food as punishment. -

R&B/ -NOP Timbaland Makes a `Proposal'
R&B/ -NOP Timbaland Makes A `Proposal' Rapper Says Duo's Second Project On Blackground Is His Last As An Artist BY RASHAUN HALL Timbaland says the CD will be his understanding how it works and NEW YORK- Timing is everything last as an artist. how the money is made." when it comes to releasing a record. For Magoo, who found himself Working with renewed focus, the Just ask Timbaland & Magoo, whose grappling with newfound fame after duo crafted Indecent Proposal, a 15- and The Blues,. BlackgroundNirgin sophomore proj- track set featuring guest appear- ect, Indecent Proposal, is now set for ances by Aaliyah, Ludacris, Jay -Z, SNOOP'S NEW HOME: Snoop Dogg is Backstage after the Atlanta show, a Nov. 20 release after a long delay. and Tweet, among others. Magoo setting up shop at MCA Records. But Wright commented on her desire for "I turned [the album] in a year - credits Timbaland with matching the former No Limit/Priority rapper onstage spontaneity. "I'm just being and -a -half ago, and it's just [now] artists to its tracks. still has one more studio album under me," she says. "It's easy. I wrote a coming out," a frustrated Timbaland "He has an idea of what direction that contract before he can exit. The bunch of songs that I really like, and I says. "And now we're in a recession - each song should go in," Magoo says. MCA deal also includes Snoop Dogg's have some very capable musicians and it doesn't make sense." "It has a lot to do with the concept Doggy Style Records, formerly distrib- vocalists helping me create the colors The delay was partially due to and who can come up with a good uted by TVT, and the production of and the pictures that I want onstage. -

Razorcake Issue #25 As A
ot too long ago, I went to visit some relatives back in Radon, the Bassholes, or Teengenerate, during every spare moment of Alabama. At first, everybody just asked me how I was my time, even at 3 A.M., was often the only thing that made me feel N doing, how I liked it out in California, why I’m not mar- like I could make something positive out of my life and not just spend N it mopping floors. ried yet, that sort of thing. You know, just the usual small talk ques- tions that people feel compelled to ask, not because they’re really For a long time, records, particularly punk rock records, were my interested but because they’ll feel rude if they don’t. Later on in the only tether to any semblance of hope. Growing up, I was always out of day, my aunt started talking to me about Razorcake, and at one point place even among people who were sort of into the same things as me. she asked me if I got benefits. It’s probably a pretty lame thing to say, but sitting in my room listen- I figured that it was pretty safe to assume that she didn’t mean free ing to Dillinger Four or Panthro UK United 13 was probably the only records and the occasional pizza. “You mean like health insurance?” time that I ever felt like I wasn’t alone. “Yeah,” she said. “Paid vacation, sick days, all that stuff. But listening to music is kind of an abstract. -

The Bird That Flew Backwards
Ursinus College Digital Commons @ Ursinus College English Honors Papers Student Research 4-15-2018 The irB d That Flew Backwards Robin Gow Ursinus College, [email protected] Adviser: Meredith Goldsmith Follow this and additional works at: https://digitalcommons.ursinus.edu/english_hon Part of the American Studies Commons, Digital Humanities Commons, English Language and Literature Commons, Lesbian, Gay, Bisexual, and Transgender Studies Commons, and the Other Feminist, Gender, and Sexuality Studies Commons Click here to let us know how access to this document benefits oy u. Recommended Citation Gow, Robin, "The irB d That Flew Backwards" (2018). English Honors Papers. 7. https://digitalcommons.ursinus.edu/english_hon/7 This Paper is brought to you for free and open access by the Student Research at Digital Commons @ Ursinus College. It has been accepted for inclusion in English Honors Papers by an authorized administrator of Digital Commons @ Ursinus College. For more information, please contact [email protected]. Gow 1 The Bird that Flew Backwards Robin F. Gow 04/20/2018 Submission Statement: Submitted to the Faculty of Ursinus College in fulfillment of the requirements for Honors in English Gow 2 Abstract: The Bird that Flew Backwards examines women poets from literary Modernism in the 1910s and Beat culture in the 1950s. Analyzing these eras in tandem reveals contrasting historical constructions of American womanhood and how sociocultural trends influenced how the “poetess” constructed herself and her work and illustrates the retrograde nature of women’s rights in the 1950s. Through close reading, digital mapping, and historical background, The Bird that Flew Backwards establishes a new critical perspective by linking the more well-known Modernists with lesser-known women in 1910s Greenwich Village Bohemia. -

REM E. Bow the Letter Nelly E.I Katy Perry E.T Cam Zoller Earl Didn't Die
REM E. Bow The Letter Nelly E.I Katy Perry E.T Cam Zoller Earl Didn't Die Weeknd Earned It Penguins Earth Angel UB40 Earth dies screaming Michael Jackson Earth Song Ricochet Ease My Troubled Mind Michael Jackson and Diana Ross Ease On Down The Road Jerry Reed East Bound and Down Commodores Easy Rascal Flatts & Natasha Bedingfield Easy Kiss Easy as it Seems George Strait Easy Come Easy Go Clint Black and Lisa Hartman Easy For Me To Say Terri Clark Easy From Now On Uriah Heep Easy Livin' Charlie Rich Easy Look Three Dog Night Easy To Be Hard Five For Fighting Easy Tonight Weird Al Yankovic Eat It Krokus Eat The rich Aerosmith Eat The Rich Wheeler Walker Jr Eatin Pussy/Kickin Ass Stevie Wonder & Paul McCartney Ebony And Ivory Everyly Brothers Ebony Eyes Trapt Echo Martha & The Muffins Echo Beach Pink Floyd Eclipse Sound of Music Edelweis Vince Hill Edelweiss Lady Gaga Edge of Glory Stevie Nicks Edge of Seventeen TED GÄRDESTAD Egen måne Beyonce Ego Beatles Eight Days a Week Alanis Morissette Eight Easy Steps Byrds Eight Miles High Kathy Mattea Eighteen Wheels And A Dozen Roses Marty Robbins El Paso City Amy Grant El Shaddai Sia Elastic Heart Pearl Jam Elderly woman Behind a Counter In A Small Town Low Millions Eleanor Alice Cooper Elected Eddie Grant Electric Avenue Lady Gaga Electric Chapel Marcia Griffiths Electric Slide REM Electrolite INXS Elegantly Wasted Tears for Fears Elemental Moulin Rouge Elephant Love Medley U2 Elevation Three Dog Night Eli's Coming Billy Gilman Elizabeth Bob Lind Elusive Butterfly Oak Ridge Boys Elvira Confederate -

Songs by Artist
Songs by Artist Title Title (Hed) Planet Earth 2 Live Crew Bartender We Want Some Pussy Blackout 2 Pistols Other Side She Got It +44 You Know Me When Your Heart Stops Beating 20 Fingers 10 Years Short Dick Man Beautiful 21 Demands Through The Iris Give Me A Minute Wasteland 3 Doors Down 10,000 Maniacs Away From The Sun Because The Night Be Like That Candy Everybody Wants Behind Those Eyes More Than This Better Life, The These Are The Days Citizen Soldier Trouble Me Duck & Run 100 Proof Aged In Soul Every Time You Go Somebody's Been Sleeping Here By Me 10CC Here Without You I'm Not In Love It's Not My Time Things We Do For Love, The Kryptonite 112 Landing In London Come See Me Let Me Be Myself Cupid Let Me Go Dance With Me Live For Today Hot & Wet Loser It's Over Now Road I'm On, The Na Na Na So I Need You Peaches & Cream Train Right Here For You When I'm Gone U Already Know When You're Young 12 Gauge 3 Of Hearts Dunkie Butt Arizona Rain 12 Stones Love Is Enough Far Away 30 Seconds To Mars Way I Fell, The Closer To The Edge We Are One Kill, The 1910 Fruitgum Co. Kings And Queens 1, 2, 3 Red Light This Is War Simon Says Up In The Air (Explicit) 2 Chainz Yesterday Birthday Song (Explicit) 311 I'm Different (Explicit) All Mixed Up Spend It Amber 2 Live Crew Beyond The Grey Sky Doo Wah Diddy Creatures (For A While) Me So Horny Don't Tread On Me Song List Generator® Printed 5/12/2021 Page 1 of 334 Licensed to Chris Avis Songs by Artist Title Title 311 4Him First Straw Sacred Hideaway Hey You Where There Is Faith I'll Be Here Awhile Who You Are Love Song 5 Stairsteps, The You Wouldn't Believe O-O-H Child 38 Special 50 Cent Back Where You Belong 21 Questions Caught Up In You Baby By Me Hold On Loosely Best Friend If I'd Been The One Candy Shop Rockin' Into The Night Disco Inferno Second Chance Hustler's Ambition Teacher, Teacher If I Can't Wild-Eyed Southern Boys In Da Club 3LW Just A Lil' Bit I Do (Wanna Get Close To You) Outlaw No More (Baby I'ma Do Right) Outta Control Playas Gon' Play Outta Control (Remix Version) 3OH!3 P.I.M.P. -

Xzibit Rap Zone Hip-Hop Video Collection Mp3, Flac, Wma
Xzibit Rap Zone Hip-Hop Video Collection mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Hip hop Album: Rap Zone Hip-Hop Video Collection Country: Russia Style: Thug Rap, Gangsta, Pop Rap MP3 version RAR size: 1419 mb FLAC version RAR size: 1108 mb WMA version RAR size: 1671 mb Rating: 4.5 Votes: 421 Other Formats: VOC MP3 AU ASF ADX MP4 AA Tracklist Ludacris - Best Of Videos 1 –Ludacris What's Your Fantasy 4:04 2 –Missy Elliott One Minute Man 4:11 3 –Ludacris Southern Hospitality 4:33 4 –Ludacris Rollout 3:48 5 –Ludacris / LL Cool J / Keith Murray Fatty Girl 3:52 6 –Ludacris feat. Nate Dogg Area Codes 3:27 7 –Ludacris Saturday Night (Oooh, Oooh) 3:37 8 –Jermaine Dupri feat. Ludacris Welcome To Atlanta 3:45 9 –Shawnna feat. Ludacris Shake Da **** 3:14 10 –Ludacris P-Poppin 5:05 11 –Ludacris Act A Fool 4:33 12 –Ludacris feat. Shawnna Stand Up 3:33 13 –Ludacris Splash Waterfalls 4:06 14 –Ludacris Get Back 5:19 Xzibit 15 –Xzibit Paparazzi 3:50 16 –Xzibit The Foundation 3:50 17 –Snoop Dogg feat. Xzibit B-Please 3:44 18 –Xzibit Year 2000 4:18 19 –Xzibit feat. Dr. Dre & Snoop Dogg X 4:09 20 –Xzibit Front To Back 3:00 21 –Xzibit Get Your Walk On 3:42 22 –Xzibit What You See Is What You Get 4:46 23 –Xzibit Multiply 3:49 24 –Xzibit Hey Now (Mean Muggin) 4:00 Notes No barcode. Track 5 listed on cover and in DVD menu as "Tatty Girl" Track 24 listed on cover and in DVD menu as "Hay Now (mean muggin)" Videos contain "MTV" and "yo! hip hop videos" logos and were most possibly recorded digitally from satellite TV. -

Songs by Artist
Andromeda II DJ Entertainment Songs by Artist www.adj2.com Title Title Title 10,000 Maniacs 50 Cent AC DC Because The Night Disco Inferno Stiff Upper Lip Trouble Me Just A Lil Bit You Shook Me All Night Long 10Cc P.I.M.P. Ace Of Base I'm Not In Love Straight To The Bank All That She Wants 112 50 Cent & Eminen Beautiful Life Dance With Me Patiently Waiting Cruel Summer 112 & Ludacris 50 Cent & The Game Don't Turn Around Hot & Wet Hate It Or Love It Living In Danger 112 & Supercat 50 Cent Feat. Eminem And Adam Levine Sign, The Na Na Na My Life (Clean) Adam Gregory 1975 50 Cent Feat. Snoop Dogg And Young Crazy Days City Jeezy Adam Lambert Love Me Major Distribution (Clean) Never Close Our Eyes Robbers 69 Boyz Adam Levine The Sound Tootsee Roll Lost Stars UGH 702 Adam Sandler 2 Pac Where My Girls At What The Hell Happened To Me California Love 8 Ball & MJG Adams Family 2 Unlimited You Don't Want Drama The Addams Family Theme Song No Limits 98 Degrees Addams Family 20 Fingers Because Of You The Addams Family Theme Short Dick Man Give Me Just One Night Adele 21 Savage Hardest Thing Chasing Pavements Bank Account I Do Cherish You Cold Shoulder 3 Degrees, The My Everything Hello Woman In Love A Chorus Line Make You Feel My Love 3 Doors Down What I Did For Love One And Only Here Without You a ha Promise This Its Not My Time Take On Me Rolling In The Deep Kryptonite A Taste Of Honey Rumour Has It Loser Boogie Oogie Oogie Set Fire To The Rain 30 Seconds To Mars Sukiyaki Skyfall Kill, The (Bury Me) Aah Someone Like You Kings & Queens Kho Meh Terri -

The Snow Miser Song 6Ix Toys - Tomorrow's Children (Feat
(Sandy) Alex G - Brite Boy 1910 Fruitgum Company - Indian Giver 2 Live Jews - Shake Your Tuchas 45 Grave - The Snow Miser Song 6ix Toys - Tomorrow's Children (feat. MC Kwasi) 99 Posse;Alborosie;Mama Marjas - Curre curre guagliò still running A Brief View of the Hudson - Wisconsin Window Smasher A Certain Ratio - Lucinda A Place To Bury Strangers - Straight A Tribe Called Quest - After Hours Édith Piaf - Paris Ab-Soul;Danny Brown;Jhene Aiko - Terrorist Threats (feat. Danny Brown & Jhene Aiko) Abbey Lincoln - Lonely House - Remastered Abbey Lincoln - Mr. Tambourine Man Abner Jay - Woke Up This Morning ACID MOTHERS TEMPLE - Are We Experimental? Adolescents - Democracy Adrian Sherwood - No Dog Jazz Afro Latin Vintage Orchestra - Ayodegi Afrob;Telly Tellz;Asmarina Abraha - 808 Walza Afroman - I Wish You Would Roll A New Blunt Afternoons in Stereo - Kalakuta Republik Afu-Ra - Whirlwind Thru Cities Against Me! - Transgender Dysphoria Blues Aim;Qnc - The Force Al Jarreau - Boogie Down Alabama Shakes - Joe - Live From Austin City Limits Albert King - Laundromat Blues Alberta Cross - Old Man Chicago Alex Chilton - Boplexity Alex Chilton;Ben Vaughn;Alan Vega - Fat City Alexia;Aquilani A. - Uh La La La AlgoRythmik - Everybody Gets Funky Alice Russell - Humankind All Good Funk Alliance - In the Rain Allen Toussaint - Yes We Can Can Alvin Cash;The Registers - Doin' the Ali Shuffle Amadou & Mariam - Mon amour, ma chérie Ananda Shankar - Jumpin' Jack Flash Andrew Gold - Thank You For Being A Friend Andrew McMahon in the Wilderness - Brooklyn, You're -
2 Column Indented
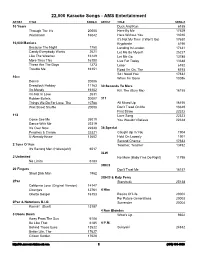
22,000 Karaoke Songs - AMS Entertainment ARTIST TITLE SONG # ARTIST TITLE SONG # 10 Years Duck And Run 6188 Through The Iris 20005 Here By Me 17629 Wasteland 16042 Here Without You 13010 It's Not My Time (I Won't Go) 17630 10,000 Maniacs Kryptonite 6190 Because The Night 1750 Landing In London 17631 Candy Everybody Wants 2621 Let Me Be Myself 25227 Like The Weather 16149 Let Me Go 13785 More Than This 16150 Live For Today 13648 These Are The Days 1273 Loser 6192 Trouble Me 16151 Road I'm On, The 6193 So I Need You 17632 10cc When I'm Gone 13086 Donna 20006 Dreadlock Holiday 11163 30 Seconds To Mars I'm Mandy 16152 Kill, The (Bury Me) 16155 I'm Not In Love 2631 Rubber Bullets 20007 311 Things We Do For Love, The 10788 All Mixed Up 16156 Wall Street Shuffle 20008 Don't Tread On Me 13649 First Straw 22322 112 Love Song 22323 Come See Me 25019 You Wouldn't Believe 22324 Dance With Me 22319 It's Over Now 22320 38 Special Peaches & Cream 22321 Caught Up In You 1904 U Already Know 13602 Hold On Loosely 1901 Second Chance 17633 2 Tons O' Fun Teacher, Teacher 13492 It's Raining Men (Hallelujah!) 6017 3LW 2 Unlimited No More (Baby I'ma Do Right) 11795 No Limits 6183 3Oh!3 20 Fingers Don't Trust Me 16157 Short Dick Man 1962 3OH!3 & Katy Perry 2Pac Starstrukk 25138 California Love (Original Version) 14147 Changes 12761 4 Him Ghetto Gospel 16153 Basics Of Life 20002 For Future Generations 20003 2Pac & Notorious B.I.G. -

The Embodiment of Asian Stereotypes in an Online Community
University of New Mexico UNM Digital Repository Sociology ETDs Electronic Theses and Dissertations 1-28-2015 "Fat for an Asian": The mbE odiment of Asian Stereotypes in an Online Community Mallory Fallin Follow this and additional works at: https://digitalrepository.unm.edu/soc_etds Recommended Citation Fallin, Mallory. ""Fat for an Asian": The mbodE iment of Asian Stereotypes in an Online Community." (2015). https://digitalrepository.unm.edu/soc_etds/14 This Thesis is brought to you for free and open access by the Electronic Theses and Dissertations at UNM Digital Repository. It has been accepted for inclusion in Sociology ETDs by an authorized administrator of UNM Digital Repository. For more information, please contact [email protected]. i Mallory Fallin Candidate Sociology Department This thesis is approved, and it is acceptable in quality and form for publication: Approved by the Thesis Committee: Dr. Kristin Barker , Chairperson Dr. Kimberly Huyser Dr. Owen Whooley ii "FAT FOR AN ASIAN":THE EMBODIMENT OF ASIAN STEREOTYPES IN AN ONLINE COMMUNITY by MALLORY FALLIN B.A., SOCIOLOGY, OREGON STATE UNIVERSITY, 2014 THESIS Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Arts Sociology The University of New Mexico Albuquerque, New Mexico December, 2014 iii “FAT FOR AN ASIAN”: THE EMBODIMENT OF ASIAN STEREOTYPES IN AN ONLINE COMMUNITY By Mallory Fallin B.A., Oregon State University, 2012 M.A., University of New Mexico, 2014 ABSTRACT Previous research has suggested that different racial groups have differing expectations of body size, but Asian Americans have largely been absent from this literature. Thick Dumpling Skin, a blog that focuses on body image issues and eating disorders in the Asian American community, provides an opportunity to study this unexplored topic.