Implementing Value-Based Health Care in Europe Handbook for Pioneers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
A Review of the Empirical Evidence of the Value of Structuring and Coding of Clinical Information Within Electronic Health Records for Direct Patient Care
Informatics in Primary Care 2012;20:171–80 # 2012 PHCSG, British Computer Society Refereed paper A review of the empirical evidence of the value of structuring and coding of clinical information within electronic health records for direct patient care Dipak Kalra PhD FRCGP FBCS Clinical Professor of Health Informatics, Centre for Health Informatics and Multiprofessional Education, University College London, UK Bernard Fernando MBBS MRCS LRCP MSc MBCS Clinical Research Fellow Zoe Morrison MSc MCIM FHEA Research Associate Aziz Sheikh MD MSc FRCGP FRCP Professor of Primary Care Research & Development eHealth Research Group, Centre for Population Health Sciences, The University of Edinburgh, UK ABSTRACT Background The case has historically been pre- improved proxy and actual clinical outcomes if a sented that structured and/or coded electronic structured and/or coded EHR was combined with health records (EHRs) benefit direct patient care, alerting or advisory systems in a focused clinical but the evidence base for this is not well docu- domain. Three studies demonstrated improvement mented. in safety outcomes. No studies were found report- Methods We searched for evidence of direct ing value in relation to patient-centredness, timeli- patient care value from the use of structured and/ ness, efficiency or equitability. or coded information within EHRs. We interro- Conclusions We conclude that, to date, there has gated nine international databases from 1990 to been patchy effort to investigate empirically the 2011. Value was defined using the Institute of value from structuring and coding EHRs for direct Medicine’s six areas for improvement for healthcare patient care. Future investments in structuring and systems: effectiveness, safety, patient-centredness, coding of EHRs should be informed by robust timeliness, efficiency and equitability. -

Improving Healthcare Quality in Europe
Cover_WHO_nr52.qxp_Mise en page 1 20/08/2019 16:31 Page 1 51 THE ROLE OF PUBLIC HEALTH ORGANIZATIONS IN ADDRESSING PUBLIC HEALTH PROBLEMS IN EUROPE PUBLIC HEALTH IN ADDRESSING ORGANIZATIONS PUBLIC HEALTH THE ROLE OF Quality improvement initiatives take many forms, from the creation of standards for health Improving healthcare 53 professionals, health technologies and health facilities, to audit and feedback, and from fostering a patient safety culture to public reporting and paying for quality. For policy- makers who struggle to decide which initiatives to prioritise for investment, understanding quality in Europe Series the potential of different quality strategies in their unique settings is key. This volume, developed by the Observatory together with OECD, provides an overall conceptual Health Policy Health Policy framework for understanding and applying strategies aimed at improving quality of care. Characteristics, effectiveness and Crucially, it summarizes available evidence on different quality strategies and provides implementation of different strategies recommendations for their implementation. This book is intended to help policy-makers to understand concepts of quality and to support them to evaluate single strategies and combinations of strategies. Edited by Quality of care is a political priority and an important contributor to population health. This Reinhard Busse book acknowledges that "quality of care" is a broadly defined concept, and that it is often Niek Klazinga unclear how quality improvement strategies fit within a health system, and what their particular contribution can be. This volume elucidates the concepts behind multiple elements Dimitra Panteli of quality in healthcare policy (including definitions of quality, its dimensions, related activities, Wilm Quentin and targets), quality measurement and governance and situates it all in the wider context of health systems research. -

Private Sector Landscape in Mixed Health Systems
Private Sector Landscape in Mixed Health Systems © WHO / Karen Reidy. Ocial WHO Logo Font: Frutiger 67 Bold Condensed Color: Black or Pantone 2925 Private Sector Landscape Private Sector Landscape in Mixed Health Systems in Mixed Health Systems ISBN TBD (electronic version) ISBN TBD (print version) © World Health Organization 2020 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence This is a conference copy (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested This publication was undertaken under the overall guidance of citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this Dr Peter Salama (WHO) and Dr Zsuzsanna Jakab (WHO). translation. The original English edition shall be the binding and authentic edition”. The editor for this publication is David Clarke (technical lead Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the for WHOs work on private sector engagement for UHC). -

Evidence from a Controlled Trial of a Healthcare System
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Copenhagen University Research Information System Know where to go Evidence from a controlled trial of a healthcare system information intervention among immigrants Jervelund, Signe Smith; Maltesen, Thomas; Wimmelmann, Camilla Lawaetz; Petersen, Jørgen Holm; Krasnik, Allan Published in: B M C Public Health DOI: 10.1186/s12889-018-5741-x Publication date: 2018 Document version Publisher's PDF, also known as Version of record Document license: CC BY Citation for published version (APA): Jervelund, S. S., Maltesen, T., Wimmelmann, C. L., Petersen, J. H., & Krasnik, A. (2018). Know where to go: Evidence from a controlled trial of a healthcare system information intervention among immigrants. B M C Public Health, 18, [863]. https://doi.org/10.1186/s12889-018-5741-x Download date: 09. apr.. 2020 Jervelund et al. BMC Public Health (2018) 18:863 https://doi.org/10.1186/s12889-018-5741-x RESEARCHARTICLE Open Access Know where to go: evidence from a controlled trial of a healthcare system information intervention among immigrants Signe Smith Jervelund1* , Thomas Maltesen2, Camilla Lawaetz Wimmelmann1, Jørgen Holm Petersen2 and Allan Krasnik1 Abstract Background: Immigrants may face problems with accessing the Danish healthcare system due to, for example, lack of knowledge of how to navigate it, which may cause inappropriate healthcare-seeking. Danish municipalities provide a mandatory introduction and language programme for newly arrived immigrants, but no information on the healthcare system is offered. This study investigated what effects information about the Danish healthcare system may have on the hypothetical healthcare-seeking behaviour of newly arrived immigrants and their actual healthcare use. -

Cross-Border Health Care in Europe (Eng)
POLICY SUMMARY 14 Cross-border health care in Europe Katharine Footman, Cécile Knai, Rita Baeten, Ketevan Glonti, Martin McKee eu Keywords: © World Health Organization 2014 (acting as the host organization for, and secretariat of, the European BURDEN OF ILLNESS Observatory on Health Systems and Policies) CHRONIC DISEASE COST EFFECTIVENESS Address requests about publications of the WHO Regional Offi ce for Europe to: DELIVERY OF HEALTH CARE, INTEGRATED Publications WHO Regional Offi ce for Europe HEALTH CARE ECONOMICS UN City, Marmorvej 51, AND ORGANIZATIONS DK-2100 Copenhagen Ø, Denmark HEALTH POLICY Alternatively, complete an online request form for documentation, health information, or for permission to quote or translate, on the Regional Offi ce web site (http://www.euro.who.int/pubrequest). All rights reserved. The Regional Offi ce for Europe of the World Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specifi c companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar This policy summary nature that are not mentioned. Errors and omissions is one of a new series excepted, the names of proprietary products are to meet the needs distinguished by initial capital letters. -

Quality Metrics for Detailed Clinical Models
i n t e r n a t i o n a l j o u r n a l o f m e d i c a l i n f o r m a t i c s 8 2 ( 2 0 1 3 ) 408–417 journa l homepage: www.ijmijournal.com Quality metrics for detailed clinical models a,b c,d a,e,∗ f,g SunJu Ahn , Stanley M. Huff , Yoon Kim , Dipak Kalra a Department of Health Policy and Management, College of Medicine in Seoul National University, 28 Yeongeon-dong, Jongno-gu, Seoul, Republic of Korea b Graduate School, Interdisciplinary Program in Biomedical Engineering, Yonsei University, 50 Yonsei-ro, Seodaemun-gu, Seoul, Republic of Korea c Intermountain Healthcare, Salt Lake City, UT, USA d Department of Biomedical Informatics, University of Utah, Salt Lake City, UT, USA e Institute of Health Policy and Management, Seoul National University Medical Research Center (SNUMRC), 28 Yeongeon-dong, Jongno-gu, Seoul, Republic of Korea f Department of Health Informatics, University College London, London, United Kingdom g Centre for Health Informatics and Multiprofessional Education, University College London, United Kingdom a r t i c l e i n f o a b s t r a c t Article history: Objective: To develop quality metrics for detailed clinical models (DCMs) and test their valid- Received 30 June 2012 ity. Received in revised form Methods: Based on existing quality criteria which did not include formal metrics, we devel- 18 September 2012 oped quality metrics by applying the ISO/IEC 9126 software quality evaluation model. -

Financing Health Care in the European Region
Financing health care in the European Union Th e European Observatory on Health Systems and Policies supports and promotes evidence- based health policy-making through comprehensive and rigorous analysis of health systems in Europe. It brings together a wide range of policy-makers, academics and practitioners to analyse trends in health reform, drawing on experience from across Europe to illuminate policy issues. Th e European Observatory on Health Systems and Policies is a partnership between the World Health Organization Regional Offi ce for Europe, the Governments of Belgium, Finland, Norway, Slovenia, Spain and Sweden, the Veneto Region of Italy, the European Investment Bank, the World Bank, the London School of Economics and Political Science and the London School of Hygiene & Tropical Medicine. Financing health care in the European Union Challenges and policy responses Sarah Thomson Thomas Foubister Elias Mossialos This study was requested and fi nanced by the European Parliament’s Committee on Employment and Social Affairs (EMPL). Keywords: FINANCING, HEALTH DELIVERY OF HEALTH CARE – economics HEALTH CARE COSTS HEALTH CARE REFORM EUROPEAN UNION © World Health Organization 2009, on behalf of the European Observatory on Health Systems and Policies All rights reserved. Th e European Observatory on Health Systems and Policies welcomes requests for permission to reproduce or translate its publications, in part or in full. Address requests about publications to: Publications, WHO Regional Offi ce for Europe, Scherfi gsvej 8, DK-2100 Copenhagen Ø, Denmark Alternatively, complete an online request form for documentation, health information, or for permission to quote or translate, on the Regional Offi ce web site (http://www.euro.who.int/pubrequest). -

Financing Sustainable Healthcare in Europe: New Approaches for New Outcomes
FINANCING SUSTAINABLE HEALTHCARE IN EUROPE: NEW APPROACHES FOR NEW OUTCOMES Conclusions from a collaborative investigation into contentious areas of healthcare February 2007 “Financing Sustainable Healthcare in Europe” presents the results of a year-long study into the sustainability of healthcare financing in Europe which was first proposed in Luxembourg in late 2004. It is endorsed by Luxembourg's Ministry of Health and by Sitra, the Finnish Innovation Fund, and is partnered by Pfizer, Inc. The views expressed in this work are those of the authors and do not necessarily represent the views and policies of the organisations to which they belong. The independence of the authors, and of all other parties who contributed to this work, is absolute. Pfizer’s intention in partnering this initiative was to stimulate novel thinking and to contribute to finding solutions for sustainable healthcare financing in Europe. TABLE OF CONTENTS Steering Committee 4 Rapporteurs 5 Contributors 5 Introduction to the report 7 Dr. Otto Graf Lambsdorff Setting the Scene 9 Pat Cox 1 Protecting equity while improving efficiency: Some possibilities for expanding the role of competition and choice in health care delivery 13 Jacques Cremer, Jean-Marie Lozachmeur (IDEI, University of Toulouse) Stephen Wright (European Investment Bank) 2 Ensuring value for money in health care: The role of HTA in the European Union 45 Corinna Sorenson, Panos Kanavos (LSE Health and Social Care) Michael Drummond (University of York) 3 Patient empowerment and efficient health outcomes 139 Reinhard Angelmar (INSEAD) Philip C. Berman (European Health Management Association) 4 Issues affecting the sustainability of health financing in several countries of south east Europe 163 Pia Schneider (The World Bank) FINANCING SUSTAINABLE HEALTHCARE IN EUROPE STEERING COMMITTEE The Steering Group had the role of guiding and overseeing the progress of the investigation. -

Health Professional Mobility in a Changing Europe
Cover_WHO_Health Professional Mobility_DRAFT_Mise en page 1 22/04/14 19:47 Page 1 32 HEALTH PROFESSIONAL MOBILITY HEALTH IN A CHANGING EUROPE Health professional mobility in Europe has become a fast moving target for policy AND DIVERSE RESPONSES MOBILE INDIVIDUALS NEW DYNAMICS, makers. It is evolving rapidly in direction and magnitude as a consequence of funda- Health Professional 32 mental change caused by EU enlargement and the financial and economic crisis. Health professional mobility changes the numbers of health professionals in countries and the skill-mix of the workforce, with consequences for health system performance. Mobility in Countries must factor-in mobility if they are forecasting and planning their workforce requirements. To this end they need clarity on mobility trends and the mobile Observatory workforce, and effective interventions for retaining domestic and integrating foreign- Studies Series trained health workers. Health professional mobility remains an unfinished agenda in a Changing Europe Europe, at a time when the repercussions of the financial crisis continue to impact on the European health workforce and its patterns of mobility. This book sheds new light on health professional mobility in this changing Europe. New dynamics, mobile individuals It is the second volume of the PROMeTHEUS project, following the previously published country case study volume. The 14 thematic chapters in this book are grouped in and diverse responses three parts: • The changing dynamics of health professional mobility Edited by James Buchan • The mobile individual Matthias Wismar • Policy responses in a changing Europe Irene A. Glinos Jeni Bremner The book goes well beyond situation analysis as it presents practical tools such as a yardstick for registry methodology, a typology of mobile individuals, qualitative tools for studying the motivation of the workforce and a set of concrete policy responses at EU-, national and organizational level including bi-lateral agreements, codes and workplace responses. -

Economic Crisis' Repercussions on European Healthcare Systems
Available online at www.sciencedirect.com ScienceDirect Procedia Economics and Finance 23 ( 2015 ) 525 – 533 2nd GLOBAL CONFERENCE on BUSINESS, ECONOMICS, MANAGEMENT and TOURISM, 30-31 October 2014, Prague, Czech Republic Economic Crisis' Repercussions on European Healthcare Systems Silvia Palascaa*, Elisabeta Jabab a”Alexandru Ioan Cuza” University, Doctoral School of Economics and Business Administration, Iasi, Romania b”Alexandru Ioan Cuza” University, Faculty of Economics and Business Administration, Iasi, Romania Abstract The economic crisis of the late 2000's had numerous social and political repercussions on most European countries. In this paper we aim to study the influence of the austerity measures deemed by the economic and financial meltdown on one of the most vulnerable and important systems in any country: healthcare. The empiric approach uses panel data analysis to highlight the effects of the economic crisis on each of the 34 analyzed countries, during the time span 2006-2012. The advantage of this method resides in the ability to offer both cross-time and cross-section results, as well as interactions. Our findings show a consistent tendency of European governments to diminish the spending on healthcare during the crisis, leading to the increase of out of pocket payments is some countries, which do not have a robust health insurance policy and a decrease in the number of people accessing healthcare services in the other countries. Another notable result is that there is a consistent delay between the economic crisis and the impact on healthcare, yet, when the shock is felt it is most likely to have an influence for some time, even after the economy has recovered. -
Access to Healthcare for People Facing Multiple Vulnerabilities in Health in 31 Cities in 12 Countries
© Olmo CALVO/ Médicos del Mundo © Olmo CALVO/ Welcoming refugees in Europe Access to healthcare for people facing multiple vulnerabilities in health in 31 cities in 12 countries C : 100 M : 60 J : 0 N : 0 NovemberMédecins du monde - Identité visuelle ANGLETERRE 08/07/2009 2016 TABLE OF CONTENTS 3/ ACKNOWLEDGMENTS 27/ BARRIERS IN ACCESS TO HEALTHCARE 4/ EXECUTIVE SUMMARY Overview 27 5/ 2015 IN FIGURES Giving up seeking medical European survey results (11 countries) 5 advice or treatment 30 Key figures for Turkey 5 Denial of access to care by a health provider 30 Focus: Pregnant women 5 Discrimination in healthcare facilities 30 Focus: Children 6 Fear of being arrested 30 Focus: Violence 6 31/ SELF-PERCEIVED HEALTH STATUS 7/ EUROPEAN NETWORK AND INTERNATIONAL OBSERVATORY 32/ HEALTH STATUS 7/ THE SOCIAL, ECONOMIC Health problems 32 AND POLITICAL CONTEXT IN 2015 Contraception 32 Urgent care 32 10/ RECENT LEGAL CHANGES, Acute and chronic health conditions 33 FOR BETTER OR WORSE Necessary treatment 33 France 10 Patients had received little or Germany 10 no care before visiting our clinics 33 Greece 10 Chronic conditions: Luxembourg 10 no access, no continuity 34 Norway 10 Infectious disease screening 34 Spain 10 Sweden 11 36/ FOCUS ON PREGNANT WOMEN Switzerland 11 Geographic origin of pregnant women 37 Turkey 11 Administrative status 37 United Kingdom 11 Living conditions 37 Isolation 37 12/ 2015 INTERNATIONAL Limiting movements 37 OBSERVATORY SURVEY HIV and hepatitis screening 38 Methodology 12 Access to healthcare 38 Statistics 12 Pregnant -
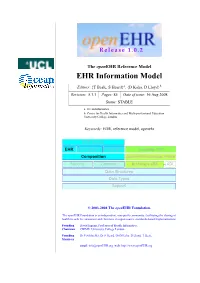
EHR Information Model
Release 1.0.2 The openEHR Reference Model EHR Information Model Editors: {T Beale, S Heard}a, {D Kalra, D Lloyd}b Revision: 5.1.1 Pages: 85 Date of issue: 16 Aug 2008 Status: STABLE a. Ocean Informatics b. Centre for Health Informatics and Multi-professional Education, University College London Keywords: EHR, reference model, openehr EHR Extract EHR Demographic Integration Template OM Composition openEHR Archetype Profile Security Common Archetype OM ADL Data Structures Data Types Support © 2003-2008 The openEHR Foundation. The openEHR Foundation is an independent, non-profit community, facilitating the sharing of health records by consumers and clinicians via open-source, standards-based implementations. Founding David Ingram, Professor of Health Informatics, Chairman CHIME, University College London Founding Dr P Schloeffel, Dr S Heard, Dr D Kalra, D Lloyd, T Beale Members email: [email protected] web: http://www.openEHR.org EHR Information Model Rev 5.1.1 Copyright Notice © Copyright openEHR Foundation 2001 - 2008 All Rights Reserved 1. This document is protected by copyright and/or database right throughout the world and is owned by the openEHR Foundation. 2. You may read and print the document for private, non-commercial use. 3. You may use this document (in whole or in part) for the purposes of making presentations and education, so long as such purposes are non-commercial and are designed to comment on, further the goals of, or inform third parties about, openEHR. 4. You must not alter, modify, add to or delete anything from the document you use (except as is permitted in paragraphs 2 and 3 above).