Hospital Preparedness for Major Incidents and Disasters In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveilla
applyparastyle “fig//caption/p[1]” parastyle “FigCapt” View metadata, citation and similar papers at core.ac.uk brought to you by CORE Open Forum Infectious Diseases provided by Apollo MAJOR ARTICLE Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveillance System Viriya Hantrakun,1, Somkid Kongyu,2 Preeyarach Klaytong,1 Sittikorn Rongsumlee,1 Nicholas P. J. Day,1,3 Sharon J. Peacock,4 Soawapak Hinjoy,2,5 and Direk Limmathurotsakul1,3,6, 1Mahidol-Oxford Tropical Medicine Research Unit (MORU), Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand, 2 Epidemiology Division, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, 3 Centre for Tropical Medicine and Global Health, Nuffield Department of Clinical Medicine, Old Road Campus, University of Oxford, Oxford, United Kingdom, 4 Department of Medicine, University of Cambridge, Cambridge, United Kingdom, 5 Office of International Cooperation, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, and 6 Department of Tropical Hygiene, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand Background. National notifiable diseases surveillance system (NNDSS) data in developing countries are usually incomplete, yet the total number of fatal cases reported is commonly used in national priority-setting. Melioidosis, an infectious disease caused by Burkholderia pseudomallei, is largely underrecognized by policy-makers due to the underreporting of fatal cases via the NNDSS. Methods. Collaborating with the Epidemiology Division (ED), Ministry of Public Health (MoPH), we conducted a retrospec- tive study to determine the incidence and mortality of melioidosis cases already identified by clinical microbiology laboratories nationwide. A case of melioidosis was defined as a patient with any clinical specimen culture positive for B. -

September 17-11 Pp01
ANDAMAN Edition PHUKET’S LEADING NEWSPAPER... SINCE 1993 Now NATIONWIDE Model home Architect and Engineering Exhibition woos homemakers INSIDE TODAY August 4 - 10, 2012 PhuketGazette.Net In partnership with The Nation 25 Baht COMPLAINT OF LAND ENCROACHMENT LEADS TO FULL-SCALE RAID ON RESORT UNDER CONSTRUCTION Casino fears spark raid on resort island Foreign investor’s link to casino in Laos raises suspicions By Kritsada Mueanhawong MORE than 50 officers raided a resort under construction on a small island off Phuket’s east coast on Tuesday with the suspicion that the project was intended to be opened as a casino hotel. Armed with a search warrant issued by the Phuket Provincial Court, the officers Belgium’s most inspected the site on Rang Noi Island, located about six kilometers directly off- wanted caught shore from Boat Lagoon and only 2.5km from Koh Maphrao. BELGIUM’S most wanted criminal, Marc Leading the sortie was Pol Maj Gen de Schutter, is to be extradited to Belgium Norrasak Hemnithi, Commander of Natu- to face charges of murder, money laun- ral Resources and Environmental Crime Surasak Suwannachote, 26, who confessed to ‘accidentally’ killing Ms Smith during the botched dering and economic crimes after police Suppression Division (NREC) in Bangkok, bag snatch, has denied charges of murder. Photo: Gazette file raided his home in Rawai on Monday. joined by NREC Superintendent Col Mr De Schutter, 57, was arrested by Watcharin Phusit and Witoon Chalayon- over 30 officers from the Phuket Immi- navee, an expert in aerial map photography A KILLER DAY OF DENIALS gration Police and Chalong Police at a from the Courts of Justice. -

Bangkok Medical Center BANGKOK DUSIT MEDICAL SERVICES Public Company Limited "Bangkok Medical Center Is Where Advances in Medicine Meet with Compassion" Contents
ANNUAL REPORT 2005 Bangkok Medical Center BANGKOK DUSIT MEDICAL SERVICES Public Company Limited "Bangkok Medical Center is where advances in medicine meet with compassion" Contents ë Message from the Board of Directors 2 ë Board of Directors' Profile 4 ë Report of the Audit Committee 10 ë General Information 11 ë Juristic Persons in which the Company Holds 10% of Shares or Greater 12 ë Financial Overview 15 ë Nature of Business 18 ë Research and Development 29 ë Industry Outlook and Competitions 31 ë Future Projects 34 ë Risk Factors 38 ë Shareholders Structure and Management 41 ë Corporate Governance 49 ë Transactions with Related Parties 54 ë Explanation and Analysis of Operational Results and Financial Status 57 ë Responsibility of the Board of Directors to the Financial Statements 59 ë Financial Statements and Auditor Report 62 Message from the Board of Directors The Board of Directors is pleased to present our dear shareholders with the operational results of Bngkok Dusit Medical Services Public Company Limited for 2005 as follows: All countries have been affected by the gradually rising oil prices and cost of living in 2005, more serious natural disasters, political instability in many countries and new epidemics, resulting in stagnant and receding businesses. Nevertheless, people continue to have illnesses while medical advancements are still being made. People have become more concerned about their health and private hospitals need to keep themselves abreast of new medical developments. They could not afford to remain idle as before. Hospitals need the latest medical equipments which allow early diagnosis, expert clinicians in each tract for the diagnosis and the treatment of diseases involvingall systems of the body. -

No. Provider Type Status Provider Name Telephone Number Address District Province Postcode
NO. PROVIDER TYPE STATUS PROVIDER NAME TELEPHONE NUMBER ADDRESS DISTRICT PROVINCE POSTCODE BANGKOK 1 HOSPITAL PRIVATE BANGKOK GENERAL HOSPITAL 02 310 3000 2 SOI SOONVIJAI7 HUAIKHWANG BANGKOK 10320 2 HOSPITAL PRIVATE BANGKOK CHRISTIAN HOSPITAL 02 6259000 124 BANGRAK BANGKOK 10500 3 HOSPITAL GOVERNMENT WACHIRA HOSPITAL*IPD ONLY* 02 244 3000 681 DUSIT BANGKOK 10300 4 HOSPITAL PRIVATE KLUAYNAMTHAI 1 HOSPITAL 02 769 2000 80 SOI RUBIA KHLONG TOEI BANGKOK 10110 5 HOSPITAL PRIVATE KLUAYNAMTHAI2 HOSPITAL 02 399 4259 27 SOI SUKHUMVIT 68 BANGNA BANGKOK 10260 6 HOSPITAL PRIVATE KASEMRAD RAMKHAMHAENG HOSPITAL 02 339 0000 99/9 SAPHAN SUNG BANGKOK 10240 7 HOSPITAL PRIVATE KASEMRAD BANGKAE HOSPITAL 02 804 8959 240/24- 25 MOO 1 BANGKHAE BANGKOK 10160 8 HOSPITAL PRIVATE KASEMRAD PRACHACHUEN HOSPITAL 02 910 1600 950 BANGSUE BANGKOK 10800 9 HOSPITAL PRIVATE KLONGTUN HOSPITAL *IPD ONLY* 02 319 2101 3284 HUAIKHWANG BANGKOK 10320 10 HOSPITAL PRIVATE CAMILLIAN HOSPITAL 02 185 1444 423 WATTANA BANGKOK 10110 11 HOSPITAL PRIVATE CHAO PHYA HOSPITAL 02 434 1111 113/44 BANGKOK NOI BANGKOK 10700 12 HOSPITAL PRIVATE CGH PHAHOLYOTHIN HOSPITAL 02 552 8777 290 BANGKHEN BANGKOK 10220 13 HOSPITAL PRIVATE CGH SAIMAI HOSPITAL 02 991 8999 91 MOO 1 SAIMAI BANGKOK 10220 14 HOSPITAL PRIVATE SAINT LOUIS HOSPITAL 02 838 5555 215 SATHON BANGKOK 10120 15 HOSPITAL GOVERNMENT POLICE GENERAL HOSPITAL *IPD ONLY* 02 207 6000 492/1 PATHUMWAN BANGKOK 10330 16 HOSPITAL PRIVATE THEPTHARIN HOSPITAL 02 348 7000 3850 KHLONG TOEI BANGKOK 10250 17 HOSPITAL PRIVATE THAI NAKARIN HOSPITAL 02 361 2727 345 MOO 11 BANGNA BANGKOK 10260 18 HOSPITAL PRIVATE THONBURI 1 HOSPITAL 02 487 2000 34/1 BANGKOK NOI BANGKOK 10700 19 HOSPITAL PRIVATE THONBURI 2 HOSPITAL 02 487 2100 BRANCH 1 NO. -
Provider Network Nov 2020.Xlsx
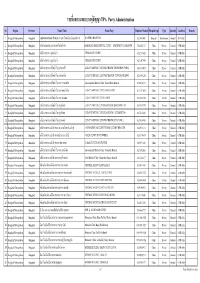
รายชื&อสถานพยาบาลค่สัญญาู TPA Party Administration No. Region Province Name (Thai) Name (Eng) Telephone Number Hospital type Type Specialty Condition Remark 1 Bangkok Metropolitan Bangkok คณะแพทยศาสตร์วชิรพยาบาล มหาวิทยาลัยนวมินทราธิราช WACHIRA HOSPITAL 02 244 3000 Hospital Government General IPD Only 2 Bangkok Metropolitan Bangkok คลินิกทันตกรรมบางกอกสไมล์(อโศก) BANGKOK SMILE DENTAL CLINIC – SUKHUMVIT 21 BRANCH 02 664 2155 Clinic Private General OPD Only 3 Bangkok Metropolitan Bangkok คลินิกเวชกรรม จุฬารัตน์ 7 CHULARAT 7 CLINIC 02 328 7653 Clinic Private General OPD Only 4 Bangkok Metropolitan Bangkok คลินิกเวชกรรม จุฬารัตน์ 8 CHULARAT 8 CLINIC 02 326 7993 Clinic Private General OPD Only 5 Bangkok Metropolitan Bangkok คลินิกเวชกรรมกล้วยนํUาไท ชุมชน70ไร่ KLUAYNAMTHAI CLINICWECHGUM (CHUMCHON 70 RAI ) 02 671 4053 Clinic Private General OPD Only 6 Bangkok Metropolitan Bangkok คลินิกเวชกรรมกล้วยนํUาไท ทุ่งสองห้อง KLUAYNUMTHAI CLINICWECHAGUM (TUNGSONGHONG) 02 500 4296 Clinic Private General OPD Only 7 Bangkok Metropolitan Bangkok คลินิกเวชกรรมกล้วยนํUาไท สาขา สวนเพลิน Kluaynamthai Medical Clinic, Suan Phloen Branch 02 042 6337 Clinic Private General OPD Only 8 Bangkok Metropolitan Bangkok คลินิกเวชกรรมกล้วยนํUาไท สาขาพหลโยธิน KLUAYNAMTHAI CLINIC PAHOLYOTIN 02 115 7638 Clinic Private General OPD Only 9 Bangkok Metropolitan Bangkok คลินิกเวชกรรมกล้วยนํUาไท สาขาอ่อนนุช KLUAYNAMTHAI CLINIC ONNUT 02 742 4398 Clinic Private General OPD Only 10 Bangkok Metropolitan Bangkok คลินิกเวชกรรมกล้วยนํUาไท สุขุมวิท56 KLUAYNAMTHAI CLINICWACHGUM (SUKUMWIT 56 -

American Fugitive Nabbed in Rawai
AV Front Eye Volume 15 Issue 8 News Desk - Tel: 076-236555February 23 - 29, 2008 Daily news at www.phuketgazette.net 25 Baht The Gazette is published in association with Heritage American fugitive plan for Andaman IN THIS ISSUE nabbed in Rawai NEWS: Yachts get tracked; Sea Sea Gypsies ask for help; By Natcha Yuttaworawit Boat blows up; PIA gets more PHUKET (Gazette, Nation, BANGKOK (Nation): The taxis. Pages 2 & 3 Kom Chad Luek): A man wanted Natural Resources and Environ- for child molestation by police in ment Ministry plans to propose the INSIDE STORY: .Smoking laws leave puffers perplexed. the US state of Missouri was Andaman Sea as a Unesco World Pages 4 & 5 arrested on the afternoon of Heritage site next year, a senior February 12 and has been turned official said on February 18. AROUND THE NATION: Tourism over to the US Federal Bureau National Park, Wildlife and minister gets straight to work. of Investigation (FBI) for extra- Plant Conservation Department Page 7 dition. Director-General Chalermsak During questioning, the sus- Vanichsombat said his office had AROUND THE REGION: Looking pect, Earl Russel Bonds, tried to back at forgotten times in assigned Dr Sakanan Plathong, a kill himself by cutting his left wrist Krabi. Page 8 lecturer on Marine Ecology at with scissors, but police seized the Prince of Songkhla University, and AROUND THE SOUTH: Girl killed scissors from him in time. Chulalongkorn University experts after hitman's suspected Bonds, 42, was handed to to make a report of Andaman blunder. Page 9 FBI agents at Phuket Interna- marine conservation areas. -

Role of Efavirenz Plasma Concentrations on Long-Term HIV Suppression and Immune Restoration in HIV-Infected Children
RESEARCH ARTICLE Role of efavirenz plasma concentrations on long-term HIV suppression and immune restoration in HIV-infected children 1,2,3,4 5,6,7 8,9 3 Nontiya HomkhamID *, Tim R. Cressey , Naim Bouazza , Lily Ingsrisawang , Pornchai Techakunakorn10, Jutarat Mekmullica11, Thitiporn Borkird12, Achara Puangsombat13, Sathaporn Na-Rajsima14, Jean Marc Treluyer8,9, Saik Urien8,9³, Gonzague Jourdain1,5,6³ a1111111111 1 Institut de recherche pour le deÂveloppement (IRD UMI 174), Marseille, France, 2 Ecole Doctorale de Sante Publique, Universite Paris Saclay, Paris, France, 3 Department of Statistics, Faculty of Science, Kasetsart a1111111111 University, Bangkok, Thailand, 4 Faculty of Public Health, Thammasat University, Bangkok, Thailand, a1111111111 5 Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand, 6 Harvard T.H. a1111111111 Chan School of Public Health, Boston, Massachusetts, United States of America, 7 Department of Molecular a1111111111 & Clinical Pharmacology, University of Liverpool, Liverpool, United Kingdom, 8 Unite de Recherche Clinique Paris Centre, Assistance Publique-HoÃpitaux de Paris, Paris, France, 9 CIC1419, INSERM & APHP, EAU08 Universite Paris Descartes Sorbonne Paris CiteÂ, Paris, France, 10 Phayao Provincial Hospital, Phayao, Thailand, 11 Bhumibol Adulyadej Hospital, Bangkok, Thailand, 12 Hat Yai Hospital, Songkla, Thailand, 13 Samutprakarn Hospital, Samutprakarn, Thailand, 14 Mahasarakam Hospital, Mahasarakam, Thailand OPEN ACCESS ³ S.U. and G.J. contributed equally as last authors to this work. * [email protected] Citation: Homkham N, Cressey TR, Bouazza N, Ingsrisawang L, Techakunakorn P, Mekmullica J, et al. (2019) Role of efavirenz plasma concentrations on long-term HIV suppression and Abstract immune restoration in HIV-infected children. PLoS ONE 14(5): e0216868. -

Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveilla
applyparastyle “fig//caption/p[1]” parastyle “FigCapt” Open Forum Infectious Diseases MAJOR ARTICLE Clinical Epidemiology of 7126 Melioidosis Patients in Thailand and the Implications for a National Notifiable Diseases Surveillance System Viriya Hantrakun,1, Somkid Kongyu,2 Preeyarach Klaytong,1 Sittikorn Rongsumlee,1 Nicholas P. J. Day,1,3 Sharon J. Peacock,4 Soawapak Hinjoy,2,5 and Direk Limmathurotsakul1,3,6, 1Mahidol-Oxford Tropical Medicine Research Unit (MORU), Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand, 2 Epidemiology Division, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, 3 Centre for Tropical Medicine and Global Health, Nuffield Department of Clinical Medicine, Old Road Campus, University of Oxford, Oxford, United Kingdom, Downloaded from https://academic.oup.com/ofid/article-abstract/6/12/ofz498/5629151 by guest on 01 June 2020 4 Department of Medicine, University of Cambridge, Cambridge, United Kingdom, 5 Office of International Cooperation, Department of Disease Control, Ministry of Public Health, Nonthaburi, Thailand, and 6 Department of Tropical Hygiene, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand Background. National notifiable diseases surveillance system (NNDSS) data in developing countries are usually incomplete, yet the total number of fatal cases reported is commonly used in national priority-setting. Melioidosis, an infectious disease caused by Burkholderia pseudomallei, is largely underrecognized by policy-makers due to the underreporting of fatal cases via the NNDSS. Methods. Collaborating with the Epidemiology Division (ED), Ministry of Public Health (MoPH), we conducted a retrospec- tive study to determine the incidence and mortality of melioidosis cases already identified by clinical microbiology laboratories nationwide. A case of melioidosis was defined as a patient with any clinical specimen culture positive for B. -

Annex 5 REPORTS of the SYSTEMATIC REVIEWS Guidelines for Treatment of Drug-Susceptible Tuberculosis and Patient Care
TREATMENT OF TUBERCULOSIS Annex 5 REPORTS OF THE SYSTEMATIC REVIEWS Guidelines for treatment of drug-susceptible tuberculosis and patient care 2017 UPDATE TREATMENT OF TUBERCULOSIS Annex 5 REPORTS OF THE SYSTEMATIC REVIEWS Guidelines for treatment of drug- susceptible tuberculosis and patient care 2017 UPDATE Guidelines for treatment of drug-susceptible tuberculosis and patient care, 2017 update ISBN 978-92-4-155000-0 © World Health Organization 2017 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Guidelines for the treatment of drug-susceptible tuberculosis and patient care, 2017 update. -

Copy of Provider Network Oct 2020.Xlsx
รายชื&อสถานพยาบาลค่สัญญาู TPA Party Administration No. Region Province Name (Thai) Name (Eng) Telephone Number Hospital type Type Specialty Condition Remark 1 กรุงเทพและปริมณฑล กรุงเทพมหานคร คณะแพทยศาสตร์วชิรพยาบาล มหาวิทยาลัยนวมินทราธิราช WACHIRA HOSPITAL 02 244 3000 Hospital Government General IPD Only 2 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกทันตกรรมบางกอกสไมล์(อโศก) BANGKOK SMILE DENTAL CLINIC – SUKHUMVIT 21 02 664 2155 Clinic Private General OPD Only BRANCH 3 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกเวชกรรม จุฬารัตน์ 7 CHULARAT 7 CLINIC 02 328 7653 Clinic Private General OPD Only 4 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกเวชกรรม จุฬารัตน์ 8 CHULARAT 8 CLINIC 02 326 7993 Clinic Private General OPD Only 5 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกเวชกรรมกล้วยนํUาไท ชุมชน70ไร่ KLUAYNAMTHAI CLINICWECHGUM (CHUMCHON 70 RAI) 02 671 4053 Clinic Private General OPD Only 6 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกเวชกรรมกล้วยนํUาไท ทุ่งสองห้อง KLUAYNUMTHAI CLINICWECHAGUM (TUNGSONGHONG) 02 500 4296 Clinic Private General OPD Only 7 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกเวชกรรมกล้วยนํUาไท สาขา สวนเพลิน Kluaynamthai Medical Clinic, Suan Phloen Branch 02 042 6337 Clinic Private General OPD Only 8 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกเวชกรรมกล้วยนํUาไท สาขาพหลโยธิน KLUAYNAMTHAI CLINIC PAHOLYOTIN 02 115 7638 Clinic Private General OPD Only 9 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกเวชกรรมกล้วยนํUาไท สาขาอ่อนนุช KLUAYNAMTHAI CLINIC ONNUT 02 742 4398 Clinic Private General OPD Only 10 กรุงเทพและปริมณฑล กรุงเทพมหานคร คลินิกเวชกรรมกล้วยนUาไทํ สุขุมวิท56 KLUAYNAMTHAI -

NEWSLETTER May 23, 2020
NEWSLETTER May 23, 2020 San Fran Dhammaram Temple and Saphanboon Foundation have joined hands to help hospitals in Thailand battle the COVID-19 pandemic by donating much needed medical-grade supplies like N95 face masks, PPE coveralls, face shields, non-surgical gowns, and protective socks. To date, “Students of Luang Por Thoon at San Fran Dhammaram Temple,” have donated ~$11,269.93 (365,822 baht) worth in supplies to twenty-nine hospitals, with $1,280 (~41,548.80 baht) from SFDT-based donations and $8,886.36 (~288,451.20 baht) from Saphanboon Foundation. watsanfran.org 1 QUANTITY (PC/PAIR) # PROVINCE HOSPITAL 3M Brand PPE Non-Surgic Protective Face shield N95 Mask Coverall al Gown Socks 1 Bangkok Taksin Hospital 40 50 2 Bangkok Prasat Neurological Institute 30 3 Bangkok Royal Thai Air Force Academy 40 4 Khon Kaen Nam Phong Hospital 30 5 Khon Kaen Ubolratana Hospital 30 6 Chiang Mai Health Promoting Hospital 50 50 7 Nakhon Rachasima Sichon Hospital 20 8 Buriram Takrong Tai Health Center 40 9 Bueng Kan Seka Hospital 40 10 Bueng Kan Bung Khla Hospital 40 11 Bueng Kan Bueang Khong Long Hospital 40 12 Prachuap Khiri Khan Air Force Hospital 5 40 20 13 Pattani Pattani Hospital 100 Phra Nakhon Si Phra Nakhon Si Ayutthaya 14 40 30 Ayutthaya Hospital Phra Nakhon Si 15 Bang Pahan Hospital 40 30 Ayutthaya Tapan Hun Crown Prince 16 Phichit 50 Hospital 17 Phrae Phrae Hospital 30 18 Phuket Vachira Phuket Hospital 40 30 30 19 Yala Yala Hospital 50 20 Lopburi Air Force Hospital 2 50 20 watsanfran.org 2 QUANTITY (PC/PAIR) # PROVINCE HOSPITAL 3M Brand -

120 Days After Tsunami
(Draft) 120 Days after Tsunami Health Technical Office and The Bureau of Policy and Strategy Office of the Permanent Secretary, the Ministry of Public Health, Thailand Preface This report was prepared by reviewing documents from various organizations both public and private agencies in Thailand that publicized after the occurrence of Tsunami Disaster. We also reviewed some documents from abroad and retrieved some data from many websites. Besides, some data were collected from in-depth interviewing with many local personnel experienced in Tsunami Disaster, e.g.; Provincial Chief Medical Officers, Directors and Deputy Directors of General Hospitals and Community Hospitals, Heads of Nursing Division, Heads of Emergency Room, Heads of Operation Room, surgeons, District Health Officers, staff of Public Charity Foundation, staff of the Thai Red Cross Society and non governmental organizations, village health volunteers, and some people who affected with this disaster. The Ministry of Public Health organized a technical conference on Tsunami Disaster in Phuket Province during February 23rd – 24th, 2005. This conference aimed at setting up a forum for experts and health care personnel to share their experiences and opinions on Tsunami Disaster. More than 300 participants from various organizations attended this conference. They were health personnel from MOPH, universities, professional societies, Royal Thai Police Bureau, the Thai Red Cross Society and private organizations. Evidence-based data and information from the conference had been presented in this report too. However, as of the April 20th, data were still updated but not significantly different from this report. We hope that this report would be much useful to readers. We are pleased to receive further information and suggestions for the completeness of this report.