Sentinel Hospital Surveillance Week 36
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Public Service Vacancy Circular Publication No 36
PUBLIC SERVICE VACANCY CIRCULAR PUBLICATION NO 36 OF 2018 DATE ISSUED: 07 SEPTEMBER 2018 1. Introduction 1.1 This Circular is, except during December, published on a weekly basis and contains the advertisements of vacant posts and jobs in Public Service departments. 1.2 Although the Circular is issued by the Department of Public Service and Administration, the Department is not responsible for the content of the advertisements. Enquiries about an advertisement must be addressed to the relevant advertising department. 2. Directions to candidates 2.1 Applications on form Z83 with full particulars of the applicants’ training, qualifications, competencies, knowledge and experience (on a separate sheet if necessary or a CV) must be forwarded to the department in which the vacancy/vacancies exist(s). 2.2 Applicants must indicate the reference number of the vacancy in their applications. 2.3 Applicants requiring additional information regarding an advertised post must direct their enquiries to the department where the vacancy exists. The Department of Public Service and Administration must not be approached for such information. 2.4 It must be ensured that applications reach the relevant advertising departments on or before the applicable closing dates. 3. Directions to departments 3.1 The contents of this Circular must be brought to the attention of all employees. 3.2 It must be ensured that employees declared in excess are informed of the advertised vacancies. Potential candidates from the excess group must be assisted in applying timeously for vacancies and attending where applicable, interviews. 3.3 Where vacancies have been identified to promote representativeness, the provisions of sections 15 (affirmative action measures) and 20 (employment equity plan) of the Employment Equity Act, 1998 should be applied. -

13 July 2018 (Advert Is Valid for a Period of Six (6) Months up to 18 January 2019)
CLOSING DATE: 13 JULY 2018 (ADVERT IS VALID FOR A PERIOD OF SIX (6) MONTHS UP TO 18 JANUARY 2019) NOTE: Applications must be posted on the Z83 Form accompanied by copies of Qualification(s),Identity document (certified within the past three months), Proof of registration, proof of citizenship if not RSA citizen, a comprehensive CV, indicating three reference persons: Name and Contact Numbers, A relationship with reference, Reference checks will be done on nominated candidate(s). Note: Failure to submit these copies will result in the application not being considered. Please do not send any original certificates, diplomas or testimonials. Applicants must note that further Personnel Suitability checks will be conducted on short-listed and that their appointment is subject to the outcome of these checks include security clearance, security vetting, qualification verification and criminal checking. Note that correspondence will only be conducted with the short- listed candidates. If you have not been contacted by the department of Health within three (3) months of the closing date of the advertisement, please accept that your application was unsuccessful. We thank all applicants for their interest. All shortlisted candidates for SMS posts will be subjected to a technical exercise that intends to test relevant technical elements of the job, the logistics of which will be communicated by department. Following the interview and the technical exercise, the selection panel will recommend candidates to attend a generic managerial competency assessment (in compliance with the DPSA Directive on the implementation of competency based assessments). The competency assessment will be testing generic managerial competencies using the mandated DPSA SMS Competency assessments tools. -

2018 Budget Review
Budget Review 2018 Naational Treasury Republic of South Africa 21 February 2018 ISBN: 978-0-621-46020-9 RP: 03/2018 The Budget Review is compiled using the latest available information from departmental and other sources. Some of this information is unaudited or subject to revision. To obtain additional copies of this document, please contact: Communications Directorate National Treasury Private Bag X115 Pretoria 0001 South Africa Tel: +27 12 315 5944 Fax: +27 12 407 9055 The document is also available on the internet at: www.treasury.gov.za. ii iii iii iv iv v v vi Foreword The 2018 Budget arrives at a moment of opportunity for South Africa. A renewed sense of optimism has provided a much-needed boost to confidence and investment. The economic outlook has improved. And government has expressed a new resolve to strengthen policy coordination. Yet this positive turn of events should not blind us to the enormous economic and fiscal challenges facing our country. Economic growth is far too low to reduce alarmingly high unemployment and inequality. Revenue collection, on which government depends to fund social and economic spending programmes, will fall short of projections by R48.2 billion in 2017/18. The finances of several state- owned companies are in a precarious state. The 2017 Medium Term Budget Policy Statement (MTBPS) pointed out that extraordinary measures would be needed to stabilise the public finances. Without such measures, we would only delay the debt reckoning, and a growing share of spending would be absorbed by interest payments. The 2018 Budget proposals address these concerns with resolve. -

The Perceptions of General Practitioners on National Health Insurance in Chris Hani District, Eastern Cape, South Africa
South African Family Practice 2019; 61(3):102–108 https://doi.org/10.1080/20786190.2019.1596665 S Afr Fam Pract ISSN 2078-6190 EISSN 2078-6204 Open Access article distributed under the terms of the © 2019 The Authors Creative Commons License [CC BY-NC 4.0] http://creativecommons.org/licenses/by-nc/4.0 RESEARCH The perceptions of general practitioners on National Health Insurance in Chris Hani district, Eastern Cape, South Africa Mthetheleli Mbongeni Gaqavu and Robert Mash* Division of Family Medicine and Primary Care, Stellenbosch University, South Africa *Corresponding author, email: [email protected] Background: National Health Insurance (NHI) intends to provide universal health coverage to all South Africans, with equity and quality as its tenets. The participation of private general practitioners (GPs) in NHI is essential. The aim was to explore perceptions of GPs on NHI in Chris Hani district, Eastern Cape, South Africa. Methods: A descriptive phenomenological qualitative study using semi-structured individual interviews of 12 GPs from six municipalities was undertaken. Data analysis used the framework method assisted by Atlas.ti software. Results: GPs in Chris Hani district felt that NHI would improve health and benefit society and be of particular benefit to poor and rural people as it will improve access to healthcare. Lack of governmental administrative capacity and a human resource plan were seen as barriers to implementation. They believed that NHI would benefit them through a single purchaser system and support more comprehensive care. GPs were concerned about a lack of information on primary care packages, accreditation, remuneration and patient allocation. -

Public Service Vacancy Circular Publication No 21
PUBLIC SERVICE VACANCY CIRCULAR PUBLICATION NO 21 OF 2019 DATE ISSUED: 14 JUNE 2019 1. Introduction 1.1 This Circular is, except during December, published on a weekly basis and contains the advertisements of vacant posts and jobs in Public Service departments. 1.2 Although the Circular is issued by the Department of Public Service and Administration, the Department is not responsible for the content of the advertisements. Enquiries about an advertisement must be addressed to the relevant advertising department. 2. Directions to candidates 2.1 Applications on form Z83 with full particulars of the applicants’ training, qualifications, competencies, knowledge and experience (on a separate sheet if necessary or a CV) must be forwarded to the department in which the vacancy/vacancies exist(s). 2.2 Applicants must indicate the reference number of the vacancy in their applications. 2.3 Applicants requiring additional information regarding an advertised post must direct their enquiries to the department where the vacancy exists. The Department of Public Service and Administration must not be approached for such information. 2.4 It must be ensured that applications reach the relevant advertising departments on or before the applicable closing dates. 3. Directions to departments 3.1 The contents of this Circular must be brought to the attention of all employees. 3.2 It must be ensured that employees declared in excess are informed of the advertised vacancies. Potential candidates from the excess group must be assisted in applying timeously for vacancies and attending where applicable, interviews. 3.3 Where vacancies have been identified to promote representativeness, the provisions of sections 15 (affirmative action measures) and 20 (employment equity plan) of the Employment Equity Act, 1998 should be applied. -

Aliwal North: South Africa
PTC COURSE REPORT: 5-6 DECEMBER 2012: JOE GQABI DISTRICT - ALIWAL NORTH: SOUTH AFRICA. Purpose of the visit As part of the Mthatha Hospital Complex initiative for in reach-outreach programme to the Eastern Cape Province District Hospitals for 2012 -13, the Department of Surgery, Walter Sisulu University and the Primary Trauma Care - Africa region organised a 2 Day PTC course for the 5th and 6th December, 2012 at Joe Gqabi District in Aliwal North. Executive summary Aliwal North; an Eastern Cape Province boarder municipality; is located where the busy national highway N6 meets R58. The R58 connects the eastern parts of South Africa to another busy national highway N1 which runs from Johannesburg to Cape Town. The hospital is 55 bedded, recently upgraded with a bigger casualty to cope with trauma victims. Patients involved with Motor Vehicle Accidents, assaults and other trauma conditions from this part of South Africa with an estimated population of 350,000 people come first to this hospital for stabilisation prior to referral to other health facilities for definitive management. Key staff involved in planning and co-ordinating Dr Rafique Surtie; Medical Director Aliwal North Hospital approached PTC Africa Committee; organised sponsorship for this CPD accredited, 2 day PTC course for Joe Gqabi District Health providers from the Africa Health Placements - Rural Doctors Support Program (AHP-RDSP). Indeed RDSP paid for the instructors and participant’s travelling and accommodation (except those provided for by the district / the province/departments) Venue and Catering. Dr Surtie in collaboration with PTC – Africa region and Walter Sisulu University PTC Instructors together with the Joe Gqabi District Health team planned and organized the training. -

Trauma Care – the Eastern Cape Story
GUEST EDITORIAL Trauma care – the Eastern Cape story While I am writing this editorial, the bloodshed seen disciplines at the East London Hospital Complex produced a book, in the casualty, emergency and trauma units across Surgery Survival Guide. What started as a 50-page document in 2013, the Eastern Cape province still harbours fresh in my has grown to a 200-page surgical handbook in 2015, focusing purely memory. on the management of common surgical emergencies, including An estimated 48 000 South Africans are killed as trauma, general surgery, neurosurgery, urology, paediatric surgery, a result of trauma-related events annually, with a further 3.5 million orthopaedics and intensive care. With the aid of funding from the seeking healthcare as a result of trauma.[1,2] South Africa (SA)’s injury provincial department of health, the book is now widely circulated death rate is nearly twice the global average.[3] Rising levels of poverty across all health facilitates in the province. The text is very much a and unemployment, limited access to education, abuse of alcohol and work in progress and it needs to be seen whether it will stand the test drugs, widespread access to firearms and other weapons, exposure of time … but Rome was not built in a day. to violence in childhood and a weak culture of enforcement are The Guide is just one of the initiatives and changes that needs to just a few of the multiple factors contributing to this carnage. The take place to improve trauma care in the province. Emphasis needs government has implemented programmes and campaigns to address to be placed on every level of care – encouraging personnel to work these issues. -

Federal University Hospitals and Stochastic Frontier Model
Texto para Discussão 022 | 2017 Discussion Paper 022 | 2017 Federal University Hospitals and Stochastic Frontier Model Romero C. B. Rocha Instituto de Economia, Universidade Federal do Rio de Janeiro André Médici Banco Mundial This paper can be downloaded without charge from http://www.ie.ufrj.br/index.php/index-publicacoes/textos-para-discussao Federal University Hospitals and Stochastic Frontier Model July, 2017 Romero C. B. Rocha Instituto de Economia, Universidade Federal do Rio de Janeiro André Médici Banco Mundial Resumo O objetivo deste trabalho é caracterizar os Hospitais Universitários Federais (HUFs) brasileiros em termos de sua importância, suas fraquezas, suas fortalezas e suas necessidades. Além disso, o trabalho vai analisar a relação entre os HUFs e o sistema hospitalar SUS, tentando explicar como eles podem melhorar a qualidade do atendimento e racionalizar esta relação. Revisitamos alguns estudos para entender a melhor maneira dos hospitais organizarem sua governança. Finalmente, rodamos um modelo de fronteira estocástica no intuito de construir rankings de eficiência para os hospitais e analisar o quanto eles poderiam aumentar sua produção com os insumos que possuem. Os resultados encontrados nos estudos revisitados mostram que a melhor maneira de organizar a governança é através do modelo de Organizações Sociais (OS), na qual o governo contrata um operador privado sem fins lucrativos para administrar as unidades. No entanto, as unidades continuam sendo propriedade do governo e 100% financiada pelo governo sob um contrato de desempenho baseado em resultado com riscos financeiros. Os resultados encontrados no modelo de fronteira mostram que os hospitais estão mais perto da eficiência na produção ambulatorial que na produção hospitalar. -
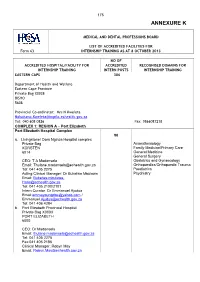
2017 in – Handbook-ANNEXURE K
175 ANNEXURE K MEDICAL AND DENTAL PROFESSIONS BOARD LIST OF ACCREDITED FACILITIES FOR Form 63 INTERNSHIP TRAINING AS AT 8 OCTOBER 2013 NO OF ACCREDITED HOSPITAL/FACILITY FOR ACCREDITED RECOGNISED DOMAINS FOR INTERNSHIP TRAINING INTERN POSTS INTERNSHIP TRAINING EASTERN CAPE 306 Department of Health and Welfare Eastern Cape Province Private Bag X0038 BISHO 5608 Provincial Co-ordinator: Mrs N Kweleta [email protected] Tel: 040 608 0826 Fax: 0866087218 COMPLEX 1: REGION A – Port Elizabeth Port Elizabeth Hospital Complex 90 a. Livingstone/ Dora Nginza Hospital complex Private Bag Anaesthesiology KORSTEN Family Medicine/Primary Care 6014 General Medicine General Surgery CEO: T A Madonsela Obstetrics and Gynaecology Email: [email protected] Orthopaedics/Orthopaedic Trauma Tel: 041 405 2275 Paediatrics Acting Clinical Manager: Dr Bukelwa Mbulawa Psychiatry Email: Bukelwa.mbulawa- [email protected] Tel: 041 405 2100/2101 Intern Curator: Dr Emmanuel Ajudua Email:[email protected] / [email protected] Tel: 041 406 4284 b. Port Elizabeth Provincial Hospital Private Bag X0003 PORT ELIZABETH 6000 CEO: Dr Madonsela Email: [email protected] Tel: 041 405 2275 Fax:041 405 2186 Clinical Manager: Robyn May Email: [email protected] 176 NO OF ACCREDITED HOSPITAL/FACILITY FOR ACCREDITED RECOGNISED DOMAINS FOR INTERNSHIP TRAINING INTERN POSTS INTERNSHIP TRAINING Uitenhage Provincial Hospital Private Bag X36 30 Anaesthesiology UITENHAGE Family Medicine/Primary Care 6630 General Medicine General Surgery CEO: Ms Klassen Obstetrics and Gynaecology Email: [email protected] Orthopaedics/Orthopaedic Trauma Tel: 041 995 1130 Paediatrics Fax: 041 9661413 Psychiatry Clinical Manager: Dr G B Walsh Email: [email protected] Tel: 041 995 1130 Intern Curator: Dr F Zietsman Email: [email protected] Tel: 041 995 1356 COMPLEX 2: REGION B – None COMPLEX 3: REGION C – East London East London Hospital Complex 108 a. -

28 July 2017
PROVINCIAL ADMINISTRATION: EASTERN CAPE DEPARMENT OF HEALTH The Department of Health is registered with the Department of Labour as a designated Employer and the filling of the following posts will be in line with the Employment Equity Act (including people with disabilities) CLOSING DATE: 28 JULY 2017 NOTE: Applications must be posted on the Z83 Form accompanied by copies of Qualification(s),Identity document (certified in the past 03 months), Proof of registration, proof of citizenship if not RSA citizen, a comprehensive CV, indicating three reference persons: Name and Contact Numbers, A relationship with reference, Reference checks will be done on nominated candidate(s). Note: Failure to submit these copies will result in the application not being considered. Please do not send any original certificates, diplomas or testimonials. Applicants must note that further checks will be conducted once they are short-listed and that their appointment is subject to the outcome of these checks include security clearance, security vetting, qualification verification and criminal checking. Note that correspondence will only be conducted with the short-listed candidates. If you have not been contacted by the dept. of Health within three (3) months of the closing date of the advertisement, please accept that your application was unsuccessful. We thank all applicants for their interest. All shortlisted candidates for SMS posts will be subjected to a technical exercise that intends to test relevant technical elements of the job, the logistics of which will be communicated by department. Following the interview and the technical exercise, the selection panel will recommend candidates to attend a generic managerial competency assessment (in compliance with the DPSA Directive on the implementation of competency based assessments). -

The Knowledge of the Registration of the Role of the Doula in the Facilitation of Natural Child Birth
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Stellenbosch University SUNScholar Repository THE KNOWLEDGE OF THE REGISTRATION OF THE ROLE OF THE DOULA IN THE FACILITATION OF NATURAL CHILD BIRTH Nonkululeko Veronica Kaibe Thesis presented in partial fulfilment of the requirements for the degree of Master of Nursing in the Faculty of Health Sciences at Stellenbosch University Supervisor: Dr ELD Boshoff March 2011 DECLARATION By submitting this thesis electronically, I declare that the entirety of the work contained therein is my own, original work, that I am the sole author thereof (save to the extent explicitly otherwise stated), that reproduction and publication thereof by Stellenbosch University will not infringe any third party rights and that I have not previously in its entirety or in part submitted it for obtaining any qualification. ___________________________ __________________________ Nonkululeko Veronica Kaibe Date Copyright © 2011 Stellenbosch University All rights reserved ii ACKNOWLEDGEMENTS My understanding of the needs of mothers’ during labour developed with my experience in teaching student nurses on training midwifery course, both the 4 year diploma and the one- year diploma. Working as a registered midwife for the past 14 years also made me realise that there was a need for ongoing support for a woman giving birth. I would like to express my thanks and gratitude to the following people: God Almighty for the strength and wisdom he gave me during this study My friends for their continuous support and encouragement My supervisor, Dr Dorothy Boshoff, for her patience, guidance and understanding; I would never have managed without her. -

Covid-19 Sentinel Hospital Surveillance for Hcws Report
COVID-19 Sentinel Hospital Surveillance Weekly Update on Hospitalized HCWs Update: Week 32, 2020 Compiled by: Epidemiology and Surveillance Division National Institute for Occupational Health 25 Hospital Street, Constitution Hill, Johannesburg This report summarises data of COVID-19 cases admitted to sentinel hospital surveillance sites in all 1 provinces. The report is based on data collected from 5 March to 8 August 2020 on the DATCOV platform. HIGHLIGHTS As of 8 August 2020, 965 (2.0%) of the 49106 COVID-19 hospital admissions recorded on the DATCOV surveillance database, were health care workers (HCWs), reported from 161 facilities (47 public-sector and 114 private-sector) in all nine provinces of South Africa. Among 565/965 (58.5%) HCWs with available data on type of work, 262/565 (46.4%) were nurses, 175/565 (31.0%) were categorized as other HCWs, 30/565 (5.3%) porters or administrators, 29/565 (5.1%) allied HCWs, 24/565 (4.2%) doctors, 13/565 (2.3%) paramedics, and 6/565 (1.1%) laboratory scientists. There was an increase of 82 new HCW admissions since week 31. There were 214 (22.2%) and 751 (77.8%) admissions reported in the public and private sector, respectively. The majority of HCW admissions were reported in Gauteng (289, 29.9%), KwaZulu-Natal (267, 27.7%), Western Cape (115, 11.9%), Free State (99, 10.3%) and Eastern Cape (93, 9.6%). The median age of COVID-19 HCW admissions was 45 years, there were 92 (9.5%) admissions in HCWs aged 60 years and older. A total of 765 (79.3%) were female.