Obstetrics and Gynecology Text Tests 1. What Is Determined by the First Leopold Maneuver in Breech Presentation? A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Heterotopic Cervical Pregnancy
Elmer ress Case Report J Clin Gynecol Obstet. 2015;4(4):307-311 Heterotopic Cervical Pregnancy Mathangi Thangavelua, b, Ravinder Kalkata Abstract tenderness or cervical excitation. Initial hormonal investiga- tions showed BHCG levels were raised to 17,276 IU and ini- We report a rare case of heterotopic cervical pregnancy, which posed tial ultrasound was suggestive of minimal retained products diagnostic challenge. With increasing IVF treatment and raising ce- of conception (Fig. 1). However, a repeat BHCG showed an sarean section rate, there is increasing incidence for non-tubal hetero- increasing trend reaching up to 29,971 IU in 96 h. A repeat topic pregnancy. We have discussed the clinical course of our case, transvaginal scan showed the endometrial cavity had mixed diagnosis and management of cervical pregnancy and some good echoes and multiple cystic spaces, largest measuring 6 × 7 × medical practices to avoid missing atypical presentations of ectopic 8 mm with color flow suggesting a possible molar pregnancy pregnancy. (Fig. 2). Bilateral ovarian cysts were present in both adnexa. Laparoscopy and dilatation and curettage were arranged Keywords: Cervical pregnancy; Heterotopic; Ectopic in view of high BHCG levels and no clear evidence of intrau- terine pregnancy. Laparoscopy was negative for tubal ectopic pregnancy and dilatation and curettage was performed. Post- operatively BHCG levels were monitored to ensure its levels were declining. The levels initially dropped to 2,611 IU from Introduction 29,971 IU in a week after D&C. However, the subsequent BHCG levels doubled to 4,207 IU 2 weeks after D&C. With We report an extremely rare case of spontaneous heterotopic the knowledge of earlier scan findings, raising BHCG levels cervical pregnancy who needed multiple investigations before raised the concern of persistent trophoblastic disease. -

Editorial 2011.Pmd
The Journal of Obstetrics and Gynecology of India January/February 2011 pg 22 - 24 Editorial Reviving the Art of Obstetrics Science of Obstetrics is more of an art, and this art is experience and skill with forceps have become difficult being increasingly forgotten today. Young to obtain. Residents are no longer taught this technique obstetricians are shying away for practicing this art in and senior obstetricians are doing it less & less. favour of Caesarean Section (CS). It has been reported Therefore, retraining the obstetric community in this that the CS rate has increased in United States to 32% 1, traditional method is an urgent task. Canada to 22.5% 2 & United Kingdom 23.8% 3. A study by the Indian Council of Medical Research (ICMR) in The forceps should be considered as an alternative to 33 tertiary care institutions noted that the average CS when the situation, so called ‘Failure to Progress’ in caesarean section rate increased from 21.8% in 1993– the lower pelvic strait occurs. Forceps remains a valid 1994 to 25.4% in 1998-1999 including 42.4% option when problems arise during second stage of primigravidas resulting into a proportionate increase labour. The most common indications are fetal in repeat CS 4. The WHO recommends that a CS rate of compromise and failure to deliver spontaneously with more than 15% is not justified. Even though today CS maximum maternal efforts. There is a clear trend to is safer than it was 30 to 40 years ago, WHO 2005 choose vacuum extractor over forceps to assist delivery global study reported a higher rate of CS was associated but evidence supports increased neonatal injury with with greater risk of maternal and perinatal mortality & vacuum extraction and lower failure rate with forceps, morbidity compared to vaginal delivery.5 This fact is depending upon the clinical circumstances 8. -

Guide to Completing the Facility Worksheets for the Certificate of Live Birth and Report of Fetal Death (2003 Revision)
Updated March 2012 March 2003 Yellow Highlights indicate updated text. Guide to Completing The Facility Worksheets for the Certificate of Live Birth and Report of Fetal Death (2003 revision) Page 1 of 51 How To Use This Guide This guide was developed to assist in completing the facility worksheets for the revised Certificate of Live Birth and Report of Fetal Death. (Facility worksheet (FWS), Birth Certificate (BC), Facility worksheet for the Report of Fetal Death (FDFWS), Report of Fetal Death (FDR)) NOTE: All information on the mother should be for the woman who gave birth to, or delivered the infant. Definitions Instructions Sources Key Words/Abbreviations Defines the items in the order they Provides specific instructions for Identifies the sources in the Identifies alternative, usually appear on the facility worksheet completing each item medical records where information synonymous terms and common for each item can be found. The abbreviations and acronyms for specific records available will items. The keywords and differ somewhat from facility to abbreviations given in this guide are facility. The source listed first not intended as inclusive. Facilities (1st) is considered the best or and practitioners will likely add to preferred source. Please use this the lists. source whenever possible. All Example― subsequent sources are listed in Keywords/Abbreviations for order of preference. The precise prepregnancy diabetes are: location within the records where DM - diabetes mellitus an item can be found is further Type 1 diabetes identified by “under” and “or.” IDDM - Insulin dependent Example— diabetes mellitus Type 2 diabetes To determine whether gestational Non-insulin dependent diabetes diabetes is recorded as a “Risk mellitus factor in this Pregnancy” (item 14) Class B DM in the records: st Class C DM The 1 or best source is : Class D DM The prenatal care record. -

Successful Treatment of Cervical Ectopic Pregnancy with Multi Dose
Case Report iMedPub Journals Gynaecology & Obstetrics Case report 2020 www.imedpub.com ISSN 2471-8165 Vol.6 No.2:14 DOI: 10.36648/2471-8165.6.2.94 Successful Treatment of Cervical Ectopic Iqbal S1*, Iqbal J2, Nowshad N1 and Pregnancy with Multi Dose Methotrexate Mohammad K1 Therapy 1 Department of Obstetrics and Gynecology, Latifa Hospital, Dubai Health Authority Jaddaf, Dubai, UAE 2 Department of Medical Education, Dubai Abstract Medical University, Dubai, UAE Cervical ectopic pregnancies account for less than 1% of all pregnancies. Earlier, it was associated with significant hemorrhage and was treated presumptively with hysterectomy. With the advent of enhanced ultrasound techniques, early *Corresponding author: Iqbal S detection of these pregnancies has led to the development of more effective conservative management. We present a case of a cervical ectopic pregnancy successfully treated with multi-dose Methotrexate therapy. [email protected] A 37-year-old lady, G3P0+2, pregnant for 9 weeks and 4 days, presented with bleeding per vagina, mild lower abdomen and back pain. Serum Beta-hCG done Department of Obstetrics and Gynecology, 5 days ago was 950 mIU/mL. She was diagnosed as ectopic cervical pregnancy Latifa Hospital, Dubai Health Authority by clinical examination which was confirmed by transvaginal ultrasonography Jaddaf, Dubai, UAE. and subsequently managed by Methotrexate (MTX) Hybrid double dose protocol. Due to rising Beta-hCG and continuous bleeding, it was modified to Multi dose Tel: 971569400124 Methotrexate Therapy. Thereafter, the patient was asymptomatic with falling beta-hCG and she was put on a weekly follow up in the clinic. Keywords: Ectopic pregnancy; Cervical pregnancy; Methrotrexate; Gynaecology Citation: Iqbal S, Iqbal J, Nowshad N, Mohammad K (2020) Successful Treatment of Cervical Ectopic Pregnancy with Multi Received: March 31, 2020; Accepted: May 02, 2020; Published: May 06, 2020 Dose Methotrexate Therapy. -

Facility Worksheet for the Live Birth Certificate-Final
Mother’s medical record # Mother’s name_ Child’s name/medical record # Attachment of ATTACHMENT TO THE FACILITY WORKSHEET FOR THE LIVE BIRTH CERTIFICATE FOR MULTIPLE BIRTHS This attachment is to be completed when at least two infants in a multiple pregnancy are born alive.* Complete a full worksheet for the first-born infant and an attachment for each additional live-born infant. A “Facility Worksheet for the Report of Fetal Death” should be completed for any fetal loss in this pregnancy reportable under State reporting requirements. Item numbers refer to item numbers on the full worksheets * For “Delayed Interval Births,” that is, births in a multiple pregnancy delivered at least 24 hours apart, a full worksheet, not an attachment should be completed. 7. Sex (Male, Female, or Not yet determined): __________________ 8. Time of birth: __ AM / PM 9. Date of birth: __ __ __ __ __ __ __ __ M M D D Y Y Y Y 10. Infant’s medical record number: 11. Mother’s medical record number: _______________________________ NEWBORN Sources: Labor and delivery records, Newborn’s medical records, mother’s medical records 12. Birthweight: _______________ (grams) Note: Do not convert lb / oz to grams If weight in grams is not available, birthweight: _____________ (lb / oz) 13. Obstetric estimate of gestation at delivery (completed weeks): ________________ (The birth attendant’s final estimate of gestation based on all perinatal factors and assessments, but not the neonatal exam. Do not compute based on date of the last menstrual period and the date of birth.) Page 1 of 5 Rev 01/01/2010 14. -

Chapter Three ~ Ending the Man-Made Cesarean Epidemic
Chapter Three ~ Ending the Man-made Cesarean Epidemic There is an effective alternative to the default use of Cesarean as a replacement for normal birth -- a plan that safely reduces medical intervention and surgical delivery while meeting the physical, emotional and psycho-social needs of childbearing women and their unborn and newborn babies. It supplies the missing ingredient by requiring the obstetrical profession to learn, teach and utilize physiological management when providing care to healthy women with normal pregnancies. Unfortunately, there are a number of obstacles to achieving this goal. One reason that obstetricians are unprepared to provide physiologically-based care for a normal childbirth this is that medical schools do not teach the scientific principles of physiological management. The countervailing belief for the last century is that obstetrical intervention is the best way prevents complications associated with childbirth and that ‘failure’ to medicalized is negligent care. For the lay public, the problem is a strong but wrong assumption that normal birth in healthy women is inevitably dangerous for babies and damaging to the pelvic floor. Most people put their faith in the high-tech, high drama variety of obstetrics portrayed in the movies and TV shows such as ER and Gray’s Anatomy. This model is tightly focused on continuous electronic fetal monitoring (EFM -- the machine that goes ‘ping’) and ‘just in the nick of time’ C-sections to rescue babies. Whatever beliefs a pregnant woman and her close relatives may have about childbirth, all of them wants what is best for the baby and its mother. We all do. -
AUC Instructions / ૂચના
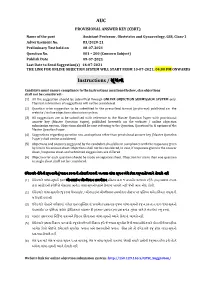
AUC PROVISIONAL ANSWER KEY (CBRT) Name of the post Assistant Professor, Obstetrics and Gynaecology, GSS, Class-1 Advertisement No. 83/2020-21 Preliminary Test held on 08-07-2021 Question No. 001 – 200 (Concern Subject) Publish Date 09-07-2021 Last Date to Send Suggestion(s) 16-07-2021 THE LINK FOR ONLINE OBJECTION SYSTEM WILL START FROM 10-07-2021; 04:00 PM ONWARDS Instructions / ૂચના Candidate must ensure compliance to the instructions mentioned below, else objections shall not be considered: - (1) All the suggestion should be submitted through ONLINE OBJECTION SUBMISSION SYSTEM only. Physical submission of suggestions will not be considered. (2) Question wise suggestion to be submitted in the prescribed format (proforma) published on the website / online objection submission system. (3) All suggestions are to be submitted with reference to the Master Question Paper with provisional answer key (Master Question Paper), published herewith on the website / online objection submission system. Objections should be sent referring to the Question, Question No. & options of the Master Question Paper. (4) Suggestions regarding question nos. and options other than provisional answer key (Master Question Paper) shall not be considered. (5) Objections and answers suggested by the candidate should be in compliance with the responses given by him in his answer sheet. Objections shall not be considered, in case, if responses given in the answer sheet /response sheet and submitted suggestions are differed. (6) Objection for each question should be made on separate sheet. Objection for more than one question in single sheet shall not be considered. ઉમેદવાર નીચેની ૂચનાઓું પાલન કરવાની તકદાર રાખવી, અયથા વાંધા- ૂચન ગે કરલ રૂઆતો યાને લેવાશે નહ (1) ઉમેદવાર વાંધાં- ૂચનો ફત ઓનલાઈન ઓશન સબમીશન સીટમ ારા જ સબમીટ કરવાના રહશે. -

The Bony Pelvis
King Khalid University Hospital Department of Obstetrics & Gynecology Course 482 ABNORMAL PRESENTATION . Occipital bone is the landmark in vertex presentation. Mentum is landmark for face presentation, . Frontal bone is land mark for brow presentation MALPRESENTATIONS . Fetal lie . This is the relationship of the longitudinal axis of the fetus to longitudinal axis of the mother. There are three lies longitudinal , oblique , and transverse lie . Fetal attitude , this is the relationship of the different parts of the baby to each others , usually flexion attitude . Presentation. It is which part of the fetus occupies the pelvis eg ,cephalic , breech , shoulder presentation . BREECH PRESENTATION . Baby is presenting with buttocks and legs and incidence is 3% at term . Types . Complete breech where the leg are flexed at hip joint and knee joint , . Frank breech flexed hip but extended knee joint . Footling breech with extended hip and knee joints and high buttocks . Fetal causes . Hydrocephalas , poly hydramnios oligohydramnios , placenta previa , short umbilical cord . Maternal causes . Uterine anomalies, fibroid uterus, small pelvis . The most important cause is preterm labor MANAGEMENT . The patient can be offered the option of either vaginal breech delivery , caesarian section or external cephalic version . External cephalic version ECV . Done after 38 weeks. Contra indications . Contracted pelvis , scar uterus, placenta previa , hypertensive patient . Complications. Membrane rupture , uterine rupture, abruptio placenta , cord prolapse . Cont. It should be done in the theater with every thing ready four c/s . If blood group is rhesus negative should receive anti D immunoglobulin . Complications of vaginal breech delivery. Cord prolaps , lower limb fracture , abdominal organs injuries , brachial plexus nerve injuries, . -

A Case of Cervical Ectopic Pregnancy JAHANARA BEGUM1, SHAMSUNNAHAR BEGUM (HENA)2, ROWSHAN ARA3, SHAMIM FATEMA NARGIS4
Bangladesh J Obstet Gynaecol, 2012; Vol. 27(1) : 31-35 A Case of Cervical Ectopic Pregnancy JAHANARA BEGUM1, SHAMSUNNAHAR BEGUM (HENA)2, ROWSHAN ARA3, SHAMIM FATEMA NARGIS4 Abstract: Cervical ectopic pregnancy is the implantation of a pregnancy in the endocervix1. Such pregnancy typically aborts within the first trimester, if it is implanted closer to the uterine cavity called cervico isthmic pregnancy it may continue longer2. Cervical pregnancy accounts for less than 1% of all ectopic pregnancies, with an estimated incidence of one in 2500 to one in 180003-5. Though the pregnancy in this area is uncommon but possibly life threatening condition due to risk of severe hemorrhage and may need hysterectomy. Early detection and conservative approach of treatment limit the morbidity and preserve fertility. A 26 years lady diagnosed as a case of cervical ectopic pregnancy and managed conservatively successfully with adjunctive techniques like cervical artery ligation and cervical temponade to control haemorrhage. The case is reported here for its relative rarity. Key Words: Cervical Ectopic, Intractable bleeding, Cervical artery ligation, cervical temponade. Introduction: and duration. She was married for 5 years, having In ectopic pregnancy the fertilized ovum becomes no issue and no history of MR or D and C. She had implanted in a site other than normal uterine cavity. It is no relevant family history. On general examination the consequence of an abnormal implantation of the she was mildly anaemic, normotensive. On per blastocyst. Worldwide incidence of ectopic pregnancy abdominal examination nothing abnormal was is 3-4% but the incidence is rising. In some studies the detected. -

Sexual and Reproductive Health
Sexual and Reproductive Health Guide for the Care of the Most Relevant Obstetric Emergencies Guide for the Care of the Most Relevant Obstetric Emergencies Fescina R*, De Mucio B*, Ortiz El**, Jarquin D**. *Latin American Center for Perinatology Women and Reproductive Health **Latin American Federation of Societies of Obstetrics and Gynecology Scientific Publication CLAP/WR N° 1594-02 Latin American Center for Perinatology Women and Reproductive Health CLAP/ WR Sexual and Reproductive Health Cataloguing-in-Publication Data Fescina R, De Mucio B, Ortiz E, Jarquin D. Guide for the care of the most relevant obstetric emergencies. Montevideo: CLAP/WR; 2013. (CLAP/WR. Scientific Publication; 1594-02) ISBN: 1. Maternal Mortality - Prevention 2. Pregnancy Complications 3. Placenta Previa 4. Pre-Eclampsia 5. Pregnancy Complications, Infectious 6. Eclampsia 7. Postnatal care 8. Postpartum Hemorrhage 9. Pregnancy, High-Risk 10.Pregnancy, Ectopic I. CLAP/WR II.Title The Pan American Health Organization welcomes requests for permission to reproduce or translate its publications, in part or in full. Applications and inquiries should be addressed to Editorial Services, Area of Knowledge Management and Communications (KMC), Pan American Health Organization, Washington, D.C., U.S.A. The Latin American Center for Perinatology, Women and Reproductive Health (CLAP/WR), Area of Family and Community Health, Pan American Health Organization, will be glad to provide the latest information on any changes made to the text, plans for new editions, and reprints and translations already available. © Pan American Health Organization, 2013 All rights reserved. Publications of the Pan American Health Organization enjoy copyright protection in accordance with the provisions of Protocol 2 of the Universal Copyright Convention. -

Board-Review-Series-Obstetrics-Gynecology-Pearls.Pdf
ObstetricsandGynecology BOARDREVIEW Third Edition Stephen G. Somkuti, MD, PhD Associate Professor Department of Obstetrics and Gynecology and Reproductive Sciences Temple University School of Medicine School Philadelphia, Pennsylvania Director, The Toll Center for Reproductive Sciences Division of Reproductive Endocrinology Department of Obstetrics and Gynecology Abington Memorial Hospital Abington Reproductive Medicine Abington, Pennsylvania New York Chicago San Francisco Lisbon London Madrid Mexico City Milan New Delhi San Juan Seoul Singapore Sydney Toronto Copyright © 2008 by the McGraw-Hill Companies, Inc. All rights reserved. Manufactured in the United States of America. Except as permitted under the United States Copyright Act of 1976, no part of this publication may be reproduced or distributed in any form or by any means, or stored in a database or retrieval system, without the prior written permission of the publisher. 0-07-164298-6 The material in this eBook also appears in the print version of this title: 0-07-149703-X. All trademarks are trademarks of their respective owners. Rather than put a trademark symbol after every occurrence of a trademarked name, we use names in an editorial fashion only, and to the benefit of the trademark owner, with no intention of infringement of the trademark. Where such designations appear in this book, they have been printed with initial caps. McGraw-Hill eBooks are available at special quantity discounts to use as premiums and sales promotions, or for use in corporate training programs. For more information, please contact George Hoare, Special Sales, at [email protected] or (212) 904-4069. TERMS OF USE This is a copyrighted work and The McGraw-Hill Companies, Inc. -

Ectopic Pregnancy
Ectopic pregnancy Reviewed By Peter Chen MD, Department of Obstetrics & Gynecology, University of Pennsylvania Medical «more » Definition An ectopic pregnancy is an abnormal pregnancy that occurs outside the womb (uterus). The baby cannot survive. Alternative Names Tubal pregnancy; Cervical pregnancy; Abdominal pregnancy Causes, incidence, and risk factors An ectopic pregnancy occurs when the baby starts to develop outside the womb (uterus). The most common site for an ectopic pregnancy is within one of the tubes through which the egg passes from the ovary to the uterus (fallopian tube). However, in rare cases, ectopic pregnancies can occur in the ovary, stomach area, or cervix. An ectopic pregnancy is usually caused by a condition that blocks or slows the movement of a fertilized egg through the fallopian tube to the uterus. This may be caused by a physical blockage in the tube. Most cases are a result of scarring caused by: y Past ectopic pregnancy y Past infection in the fallopian tubes y Surgery of the fallopian tubes Up to 50% of women who have ectopic pregnancies have had swelling (inflammation) of the fallopian tubes (salpingitis) or pelvic inflammatory disease (PID). Some ectopic pregnancies can be due to: y Birth defects of the fallopian tubes y Complications of a ruptured appendix y Endometriosis y Scarring caused by previous pelvic surgery In a few cases, the cause is unknown. Sometimes, a woman will become pregnant after having her tubes tied (tubal sterilization). Ectopic pregnancies are more likely to occur 2 or more years after the procedure, rather than right after it. In the first year after sterilization, only about 6% of pregnancies will be ectopic, but most pregnancies that occur 2 - 3 years after tubal sterilization will be ectopic.