Heart Surgery Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Harbin Clinic: Early Adoption of EMR Advantages and Challenges
The Harbin Clinic: Early Adoption of EMR Advantages and Challenges Introduction Dr. Ken Davis leaned back in his desk chair, one ankle hooked on his knee, and reflected on the events of his day. Once again, the decision had been made to make another big change at The Harbin Clinic in order to improve patient care. The Clinic had made the decision to move from their current electronic medical record (EMR)1 vendor and select new software, a new electronic medical record, and a new vendor. Dr. Davis, along with the Information Technology director, Angie McWhorter, had taken all things into consideration- the support staff, the size of the company, how dedicated the company would be to The Harbin Clinic, and whether the new technology would allow The Harbin Clinic to successfully comply with the federal government’s meaningful use mandate. When he accepted the position of CEO in 2002, Davis had told the board of directors that he would only do this for two years. And yet here he was, ten years later. Davis sighed to himself. He realized that while they had made many advancements in the past decade, in some ways the Harbin Clinic was about to face the same issues once again. While the physicians and staff were now accustomed to using an electronic medical record, the Clinic would still have to undergo another implementation process, one that would include many difficulties. Given the amount of pressure on him today, he could only imagine how Dr. Ferguson, his predecessor, had felt when he had made the decision to introduce electronic medical records into the daily operations of the Harbin Clinic for the first time in 1999. -

In the United States District Court for the Northern District of Alabama Southern Division
Case 2:11-cv-04099-RDP Document 12 Filed 03/20/13 Page 1 of 29 FILED 2013 Mar-20 PM 01:24 U.S. DISTRICT COURT N.D. OF ALABAMA IN THE UNITED STATES DISTRICT COURT FOR THE NORTHERN DISTRICT OF ALABAMA SOUTHERN DIVISION LAURA C. NOAH, } } Plaintiff, } } v. } Case No.: 2:11-CV-4099-RDP } MICHAEL J. ASTRUE, } COMMISSIONER OF } SOCIAL SECURITY, } } Defendant. } MEMORANDUM OF DECISION Plaintiff Laura C. Noah brings this action pursuant to Sections 205(g) and 1631(c)(3) of the Social Security Act (the “Act”) seeking review of the decision by the Commissioner of the Social Security Administration (“Commissioner”) denying her claim for Social Security Disability Insurance Benefits and Supplemental Security Income. (Doc. #1 at 1); see 42 U.S.C. §§ 405(g) and 1383(c). Based upon the court’s review of the record and the briefs submitted by the parties, the court finds that the decision of the Commissioner is due to be affirmed. I. Proceedings Below This action arises from Plaintiff’s applications for Social Security Disability Insurance Benefits (“DIB”) and Supplemental Security Income (“SSI”), filed November 18, 2008, alleging disability beginning on December 22, 2005,1 four days before she stopped working as a waitress at a Waffle House. (Tr. 131, 40). Both claims were denied on January 7, 2009. (Tr. 79). Plaintiff then requested and received a hearing before Administrative Law Judge Jill Lolley Vincent on August 12, 2010 in Birmingham, Alabama. (Tr. 34). In her decision, dated 1 This is Plaintiff’s third application alleging disability beginning on December 22, 2005. -

Fabric Mulch for Tree and Shrub Plantings, Kansas State University, August 2004
KANSAS Fabric Mulch for Tree FOREST SER VICE and Shrub Plantings KANSAS STATE UNIVERSITY What is Fabric Mulch? though most last well beyond the caution in riparian areas that flood Fabric mulch (often referred to time necessary to establish tree and periodically. Flooding can lower as Weed Barrier, one of many brand shrub plantings. Excessive durabil- the effectiveness of the mulch by names) is used to reduce vegetative ity results from inordinate specifi- dislocation and soil deposition. competition in newly planted trees cations and from shade created by Fabric mulch inhibits root sprouting and shrubs. This is accomplished by trees and shrubs that prevents dete- of shrubs. Root sprouting increases applying fabric over the top of trees rioration. New products are being stem density, providing valuable and shrubs after planting, cutting a tested to address this issue. wildlife habitat. hole in the fabric, and pulling the trees and shrubs through the hole. It When Should Fabric Fabric Mulch is made of a black, woven, perme- Mulch be Used? Specifications able, polypropylene geotextile that Fabric mulch is appropriate to Fabric mulch is available in can withstand the trampling of deer help establish windbreaks, shel- a variety of sizes and specifica- and deterioration from sunlight. terbelts, living snowfences, and tions. It can be purchased in rolls Fabric mulches conserve soil mois- other small tree and shrub plant- that can be applied by machine, or ture by reducing evaporation. Fabric ings. Fabric should be used with in squares that can be applied by mulches eventually biodegrade, hand. Rolls may contain from 300 to 750 feet of fabric and range from 4 to 10 feet wide. -

Marygold Manor DJ List
Page 1 of 143 Marygold Manor 4974 songs, 12.9 days, 31.82 GB Name Artist Time Genre Take On Me A-ah 3:52 Pop (fast) Take On Me a-Ha 3:51 Rock Twenty Years Later Aaron Lines 4:46 Country Dancing Queen Abba 3:52 Disco Dancing Queen Abba 3:51 Disco Fernando ABBA 4:15 Rock/Pop Mamma Mia ABBA 3:29 Rock/Pop You Shook Me All Night Long AC/DC 3:30 Rock You Shook Me All Night Long AC/DC 3:30 Rock You Shook Me All Night Long AC/DC 3:31 Rock AC/DC Mix AC/DC 5:35 Dirty Deeds Done Dirt Cheap ACDC 3:51 Rock/Pop Thunderstruck ACDC 4:52 Rock Jailbreak ACDC 4:42 Rock/Pop New York Groove Ace Frehley 3:04 Rock/Pop All That She Wants (start @ :08) Ace Of Base 3:27 Dance (fast) Beautiful Life Ace Of Base 3:41 Dance (fast) The Sign Ace Of Base 3:09 Pop (fast) Wonderful Adam Ant 4:23 Rock Theme from Mission Impossible Adam Clayton/Larry Mull… 3:27 Soundtrack Ghost Town Adam Lambert 3:28 Pop (slow) Mad World Adam Lambert 3:04 Pop For Your Entertainment Adam Lambert 3:35 Dance (fast) Nirvana Adam Lambert 4:23 I Wanna Grow Old With You (edit) Adam Sandler 2:05 Pop (slow) I Wanna Grow Old With You (start @ 0:28) Adam Sandler 2:44 Pop (slow) Hello Adele 4:56 Pop Make You Feel My Love Adele 3:32 Pop (slow) Chasing Pavements Adele 3:34 Make You Feel My Love Adele 3:32 Pop Make You Feel My Love Adele 3:32 Pop Rolling in the Deep Adele 3:48 Blue-eyed soul Marygold Manor Page 2 of 143 Name Artist Time Genre Someone Like You Adele 4:45 Blue-eyed soul Rumour Has It Adele 3:44 Pop (fast) Sweet Emotion Aerosmith 5:09 Rock (slow) I Don't Want To Miss A Thing (Cold Start) -

Gallbladder Removal
Patient Education Partners in Your Surgical Care AMericaN COLLege OF SUrgeoNS DIVisioN OF EDUcatioN Cholecystectomy Surgical Removal of the Gallbladder LaparoscopicLaparoscopic versus versus Open Open Cholecystectomy Cholecystectomy LLaparoscopicaparoscopic Cholecystectomy Cholecystectomy OpenOpen Cholecystectomy Cholecystectomy Patient Education This educational information is to help you be better informed about your operation and empower you with the skills and knowledge needed to actively participate in your care. Keeping You Informed Treatment Options Expectations Information that will help you further understand your operation. Surgery Before your operation— Evaluation usually Education is provided on: Laparoscopic cholecystectomy—The includes blood work, an gallbladder is removed with instruments abdominal ultrasound, Cholecystectomy Overview ............. 1 placed into 4 small slits in the abdomen. and an evaluation by your Condition, Symptoms, Tests ............ 2 Open cholecystectomy—The gallbladder surgeon and anesthesia Treatment Options ......................... 3 is removed through an incision on the provider to review your right side under the rib cage. health history and Risks and Possible Complications ..... 4 medications and to discuss Preparation and Expectations ......... 5 Nonsurgical pain control options. Your Recovery and Discharge ........... 6 Stone retrieval The day of your operation— Pain Control .................................. 7 For gallstones without symptoms You will not eat or drink for at least 4 hours -
Behind the 2017 Report to the Community Welcome Behind the Green
GreenBehind the 2017 Report to the Community Welcome Behind the Green Seventy-five years ago, Floyd Hospital opened its doors as the community hospital for Rome and Floyd County. An entire election centered on the call for a facility that would provide care to all comers in a post-Depression, World War II-wary community. That mission continues today. Seventy-five years later, the Floyd health system still maintains that mission and commitment to community leadership, even as it has grown to include multiple hospitals, a Primary Care network and a Family Medicine Residency program. Over the years Floyd has been a catalyst for growth and, today, it continues to be an economic engine for northwest Georgia as the county’s largest employer. Behind the Green is a review of the people, programs and compassionate acts over the past year that help tell the Floyd story. We are a not-for-profit community hospital, but what does that mean? It means we invest in our community by working in our schools and industries, by educating and screening our neighbors and by adding services and improving our facilities. And, we do all of that with a heart of compassion that you’ll read about in the pages that follow. You’ll also discover an important number, $72.8 million, which is the total cost of care Floyd and Polk provided to people in our community who could not afford to pay for their own care. On this page are elements that we assembled over the past two years to tell our 75-year story. -

A Roadmap for Recognizing, Evaluating, and Treating
Getting Tissue for Molecular Testing: An NSCLC Strategic Initiative Activity Summary Date: Jan, 2015 CME Credit Provider: Temple University School of Medicine Collaborators: Association of Community Cancer Centers (ACCC), Fox Chase Cancer Center, and MCM Education Grant Supporter: Pfizer Start Date: March, 2013 End Date: Jan, 2015 Table of Contents Executive Summary ....................................................................................................................................... 1 Introduction .................................................................................................................................................. 2 Planning Committee: .................................................................................................................................... 3 Learning Objectives ....................................................................................................................................... 3 Participating Cancer Centers ......................................................................................................................... 3 QI Initiative Design ........................................................................................................................................ 5 Molecular Testing Rates: Pre (Baseline) vs. Post (Follow-Up) ...................................................................... 5 QI Summary of Centers ................................................................................................................................ -

I Used to Think Reading Was "Lame" and "Boring". MTV Really Messed Us up :P Then I Read One Book
I used to think reading was "lame" and "boring". MTV really messed us up :P Then I read one book.... it changed my life... so I read another... it changed again... so I read another and then another. The process continued on until I became a whole new animal. Books have made my life better in every possible way from mental growth to physical and spiritual growth. Because of their immense effect on my life, I want to share the books I have read with people so they can start growing and taking control of their lives. I want you to become the best person you can possibly be! I figure that the books I've read, that have made my life better, can 100% make your life better! If you don't know where to start, pick a book from my list! If I have read it more than once, it was for a reason. You probably don't think you have time to read books. That's okay though, because I prove that's not true at all. You have time to read if you use the smart tricks I show you at the bottom of this page. The 48 Laws Of Power by Robert Greene *I've Read It 15+ times Mastery by Robert Greene 5+ times The 50th Law by Robert Greene 3+ Times Think and Grow Rich Napoleon Hill 4 times The Slight Edge by Jeff Olson 2 times 4 Hour Work Week by Tim Ferriss 2 Times The Power Of Now by Eckart Toll Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic Future The Master Key System To Riches Napoleon Hill Out Of Your Mind By Alan Watts 100 Ways To Motivate Yourself by Steve Chandler 5 Times The Strangest Secret by Earl Nightingale 3 times Eleven Keys To Excellence by John Maxwell The Winner's Brain. -
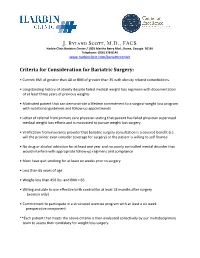
J. Ryland Scott, M.D., FACS
J. Ryland Scott, M.D., FACS Harbin Clinic Bariatric Center / 1825 Martha Berry Blvd., Rome, Georgia 30165 Telephone: (706) 378-8140 www.harbinclinic.com/bariatriccenter Criteria for Consideration for Bariatric Surgery: • Current BMI of greater than 40 or BMI of greater than 35 with obesity related comorbidities. • Longstanding history of obesity despite failed medical weight loss regimens with documentation of at least three years of previous weights • Motivated patient that can demonstrate a lifetime commitment to a surgical weight loss program with nutritional guidelines and follow-up appointments • Letter of referral from primary care physician stating that patient has failed physician supervised medical weight loss efforts and is motivated to pursue weight loss surgery • Verification from insurance provider that bariatric surgery consultation is a covered benefit (i.e. will the provider even consider coverage for surgery) or the patient is willing to self finance • No drug or alcohol addiction for at least one year and no poorly controlled mental disorder that would interfere with appropriate follow-up regimens and compliance • Must have quit smoking for at least six weeks prior to surgery • Less than 65 years of age • Weighs less than 450 lbs. and BMI < 65. • Willing and able to use effective birth control for at least 18 months after surgery (women only) • Commitment to participate in a structured exercise program with at least a six week preoperative component **Each patient that meets the above criteria is then evaluated collectively -

Official Notice
(This notice must be posted in a conspicuous place readily accessible to the employee at all times.) OFFICIAL NOTICE This business operates under the Georgia Workers' Compensation Law. WORKERS MUST REPORT ALL ACCIDENTS IMMEDIATELY TO THE EMPLOYER BY ADVISING THE EMPLOYER PERSONALLY, AN AGENT, REPRESENTATIVE, BOSS, SUPERVISOR, OR FOREMAN. If a worker is injured at work, the employer shall pay medical and rehabilitation expenses within the limits of the law. In some cases the employer will also pay a part of the worker's lost wages. Work injuries and occupational diseases should be reported in writing whenever possible. The worker may lose the right to receive compensation if an accident is not reported within 30 days (see O.C.G.A. § 34-9-80). The employer will supply free of charge, upon request, a form for reporting accidents and will also furnish, free of charge, information about workers' compensation. The employer will also furnish to the employee, upon request, copies of board forms on file with the employer pertaining to an employee's claim. A worker injured on the job must select a doctor from the list below. The minimum panel shall consist of at least six physicians, including an orthopedic surgeon with no more than two physicians from industrial clinics (see O.C.G.A. § 34-9-201). Further, this panel shall include one minority physician, whenever feasible. (See Rule 201 for definition of minority physician). The Board may grant exceptions to the required size of the panel where it is demonstrated that more than four physicians are not reasonably accessible. -

Patient Navigation Track 7:30AM Registration and Continental Breakfast
Saturday - September 7, 2013 – Patient Navigation Track 7:30AM Registration and Continental Breakfast 8:00AM Opening Remarks Co-Chairs: Lena Crooker and Gail McCray, CPNG 8:05AM Opening Plenary Session: The Importance of Patient Navigation Interventions across the Cancer Care Continuum: Survivors’ Voices Moderator: Melissa Dillmon, M.D., Harbin Clinic, Harbin Integrative Oncology Program (HIOP) Panelists: Janice Carney, Breast Cancer Patient, Harbin Clinic Moya McKoy, Ovarian Cancer Patient, Northside Hospital 9:05AM 2013 CPNG Member Survey Results and GASCO Grants Angie Patterson GASCO Update Karen Beard, Director, GASCO 9:30 AM Break- Exhibit Area 10:00AM Use of Mobile Technology & How it Can Help Patients through the Continuum of Cancer Care Presenter: Phillip Lamson, MBA – Senior Healthcare Consultant, Georgia Tech 11:00AM Breakout Sessions (two sessions occurring concurrently – conference participants will choose 1 to attend during this time) Session #1: Panel Discussion – Genetic Testing for Breast & Ovarian Cancer Panelists: Selvi Palpaniappan, MS, CGC Certified Genetic Counselor, Northside Hospital Monique Martin, MPH, CHES Health Education & Communications Specialist, Georgia CORE Victoria L. Green, M.D, JD, MBA Director, High Risk Breast Clinic & Genetic Testing Program, Grady Memorial Hospital Session #2: Advocacy Training Session for Patient Navigators Andy Lord, GASCO Lobbyist, Georgia Capitol Solutions 12:00PM Lunch Presentations - Recognition Best Poster Submission – Dr. Hillary Hahm - Matt Mumber Visionary Award for Patient -

Provider and Pharmacy Directory Provider 2017
PROVIDER 2017 PROVIDER AND PHARMACY DIRECTORY Directorio de farmacias y proveedores Cigna-HealthSpring Georgia Georgia Counties/Condados: Baldwin, Banks, Barrow, Bartow, Butts, Chattooga, Cherokee, Clarke, Clayton, Cobb, Coweta, Dawson, DeKalb, Douglas, Elbert, Fayette, Floyd, Forsyth, Franklin, Fulton, Gordon, Greene, Gwinnett, Habersham, Hall, Hart, Henry, Jackson, Jasper, Lamar, Lumpkin, Madison, Morgan, Newton, Oconee, Oglethorpe, Paulding, Pickens, Pike, Polk, Putnam, Rabun, Rockdale, Spalding, Stephens, Walton, White, Wilkes This Provider and Pharmacy Directory was updated in November 2017. For more information, please contact Cigna-HealthSpring Customer Service at 1-800-668-3813 or, for TTY users, 711, 7 days a week, 8 a.m. - 8 p.m., or visit www.cignahealthspring.com. Changes to our pharmacy network may occur during the benefit year. An updated Pharmacy Directory is located on our website at www.cignahealthspring.com. You may also call Customer Service for updated provider information. Este Directorio de proveedores y farmacias fue actualizado en noviembre de 2017. Para obtener más información, llame a Servicio al Cliente de Cigna al 1-800-668-3813 o, para los usuarios de TTY, al 711, los 7 días de la semana, de 8 a.m. a 8 p.m., o visite www.cignahealthspring.com. Es posible que, durante el año de beneficios, se realicen cambios en nuestra red de farmacias. Podrá encontrar un Directorio de farmacias actualizado en nuestro sitio web www.cignahealthspring.com. También puede llamar a Servicio al Cliente para obtener información actualizada sobre los proveedores. © 2017 Cigna 17_D_62_GA_62 INT_17_50673BL Cover Provider Pharmacy Directory GA NOV PRINT.indd 1 2/15/17 1:56 PM Cigna-HealthSpring Provider and Pharmacy Provider Directory / Directorio de farmacias y proveedores Table of Contents / Índice Provider Directory.........................................................................................................................................................................