The Relevance of Adhesion G Protein-Coupled Receptors In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Strategies to Increase ß-Cell Mass Expansion
This electronic thesis or dissertation has been downloaded from the King’s Research Portal at https://kclpure.kcl.ac.uk/portal/ Strategies to increase -cell mass expansion Drynda, Robert Lech Awarding institution: King's College London The copyright of this thesis rests with the author and no quotation from it or information derived from it may be published without proper acknowledgement. END USER LICENCE AGREEMENT Unless another licence is stated on the immediately following page this work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International licence. https://creativecommons.org/licenses/by-nc-nd/4.0/ You are free to copy, distribute and transmit the work Under the following conditions: Attribution: You must attribute the work in the manner specified by the author (but not in any way that suggests that they endorse you or your use of the work). Non Commercial: You may not use this work for commercial purposes. No Derivative Works - You may not alter, transform, or build upon this work. Any of these conditions can be waived if you receive permission from the author. Your fair dealings and other rights are in no way affected by the above. Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 02. Oct. 2021 Strategies to increase β-cell mass expansion A thesis submitted by Robert Drynda For the degree of Doctor of Philosophy from King’s College London Diabetes Research Group Division of Diabetes & Nutritional Sciences Faculty of Life Sciences & Medicine King’s College London 2017 Table of contents Table of contents ................................................................................................. -

G Protein-Coupled Receptors As New Therapeutic Targets for Type 2 Diabetes
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Diabetologia (2016) 59:229–233 DOI 10.1007/s00125-015-3825-z MINI-REVIEW G protein-coupled receptors as new therapeutic targets for type 2 diabetes Frank Reimann1 & Fiona M. Gribble 1 Received: 31 October 2015 /Accepted: 9 November 2015 /Published online: 12 December 2015 # The Author(s) 2015. This article is published with open access at Springerlink.com Abstract G protein-coupled receptors (GPCRs) in the gut– GLP1R Glucagon-like peptide 1 receptor brain–pancreatic axis are key players in the postprandial con- GPBAR1 G protein-coupled bile acid receptor trol of metabolism and food intake. A number of intestinally GPCR G protein-coupled receptor located receptors have been implicated in the chemo-detection of ingested nutrients, and in the pancreatic islets and nervous system GPCRs play essential roles in the detection of many Therapeutics that promote insulin secretion have been a main- hormones and neurotransmitters. Because of the diversity, stay of type 2 diabetes treatment for many years. However, cell-specific expression and ‘druggability’ of the GPCR su- with the rising impact of obesity on the incidence of type 2 perfamily, these receptors are popular targets for therapeutic diabetes comes an increasing need to target body weight as development. This review will outline current and potential well as blood glucose control. Recent years have witnessed an future approaches to develop GPCR agonists for the treatment increasing interest in the gut endocrine system as a source of of type 2 diabetes. -
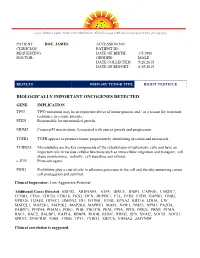
Sample Lab Report
3030 Venture Lane, Suite 108 ● Melbourne, Florida 32934 ● Phone 321-253-5197 ● Fax 321-253-5199 PATIENT: DOE, JAMES ACCESSION NO: CLINICIAN/ PATIENT ID: REQUESTING DATE OF BIRTH: 1/5/1986 DOCTOR: GENDER: MALE DATE COLLECTED: 5/26/2015 DATE OF REPORT: 6/15/2015 RESULTS PRIMARY TUMOR TYPE RIGHT TESTICLE BIOLOGICALLY IMPORTANT ONCOGENES DETECTED GENE IMPLICATION TP53 TP53 mutations may be an important driver of tumorigenesis and / or a reason for treatment resistance in a some patients. PTEN Responsible for uncontrolled growth. MDM2 Causes p53 inactivation. Associated with cancer growth and progression. TGFB1 TGFB appears to promote tumor progession by stimulating invasion and metastasis. TUBB2A Microtubules are the key components of the cytoskeleton of eukaryotic cells and have an important role in various cellular functions such as intracellular migration and transport, cell shape maintenance, polarity, cell signaling and mitosis. c-JUN Proto-oncogene PHB2 Prohibitins play a crucial role in adhesion processes in the cell and thereby sustaining cancer cell propagation and survival. Clinical Impression: Low Aggressive Potential Additional Genes Detected: ABCG2, ARHGAP5, ATF4, BIRC5, BNIP3, CAPNS1, CARD17, CCNB1, CD24, CDC20, CDK18, CKS2, DCN, DEPDC1, FTL, FZD5, FZD9, GAPDH, GNB2, GPR126, H2AFZ, HDAC1, HMGN2, ID1, IFITM1, JUNB, KPNA2, KRT18, LDHA, LTF, MAD2L1, MAP2K1, MAP2K2, MAP2K4, MAPRE1, MAS1, NME1, NME3, NPM1, PA2G4, PABPC1, PFDN4, PGAM1, PGK1, PHB, PIK3CB, PKM, PPIA, PPIH, PRKX, PRNP, PTMA, RAC1, RAC2, RALBP1, RAP1A, RBBP4, RHOB, RHOC, -

Gastrointestinal Defense Mechanisms
REVIEW CURRENT OPINION Gastrointestinal defense mechanisms Hyder Said a,b and Jonathan D. Kaunitzb,c Purpose of review To summarize and illuminate the recent findings regarding gastroduodenal mucosal defense mechanisms and the specific biomolecules involved in regulating this process, such as glucagon-like peptides (GLPs). Recent findings There has been a growing interest in luminal nutrient chemosensing and its physiological effects throughout the digestive system. From the ingestion of food in the oral cavity to the processing and absorption of nutrients in the intestines, nutrient chemosensing receptors signal the production and release of numerous bioactive peptides from enteroendocrine cells, such as the proglucagon-derived peptides. There has been a major emphasis on two proglucagon-derived peptides, namely GLP-1 and GLP-2, due to their apparent beneficial effect on gut structure, function, and on metabolic processes. As an incretin, GLP-1 not only enhances the effect and release of insulin on pancreatic bcells but also has been implicated in having trophic effects on the intestinal epithelium. In addition, GLP-2, the other major proglucagon-derived peptide, has potent intestinotrophic effects, such as increasing the rate of mucosal stem cell proliferation, mucosal blood flow, and fluid absorption, as well as augmenting the rate of duodenal bicarbonate secretion to improve gastric mucosal health and longevity. Summary Understanding the mechanisms underlying nutrient chemosensing and how it relates to GLP release can further elucidate how the gut functions in response to cellular changes and disturbances. Furthermore, a more in-depth comprehension of GLP release and its tissue-specific effects will help improve the utility of GLP-1 and GLP-2 receptor agonists in clinical settings. -

Edinburgh Research Explorer
Edinburgh Research Explorer International Union of Basic and Clinical Pharmacology. LXXXVIII. G protein-coupled receptor list Citation for published version: Davenport, AP, Alexander, SPH, Sharman, JL, Pawson, AJ, Benson, HE, Monaghan, AE, Liew, WC, Mpamhanga, CP, Bonner, TI, Neubig, RR, Pin, JP, Spedding, M & Harmar, AJ 2013, 'International Union of Basic and Clinical Pharmacology. LXXXVIII. G protein-coupled receptor list: recommendations for new pairings with cognate ligands', Pharmacological reviews, vol. 65, no. 3, pp. 967-86. https://doi.org/10.1124/pr.112.007179 Digital Object Identifier (DOI): 10.1124/pr.112.007179 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: Pharmacological reviews Publisher Rights Statement: U.S. Government work not protected by U.S. copyright General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 02. Oct. 2021 1521-0081/65/3/967–986$25.00 http://dx.doi.org/10.1124/pr.112.007179 PHARMACOLOGICAL REVIEWS Pharmacol Rev 65:967–986, July 2013 U.S. -

General Discussion
UvA-DARE (Digital Academic Repository) EGF-TM7 receptors: A diverse and still evolving family of receptors on the leukocyte surface Matmati, M. Publication date 2008 Link to publication Citation for published version (APA): Matmati, M. (2008). EGF-TM7 receptors: A diverse and still evolving family of receptors on the leukocyte surface. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:23 Sep 2021 Chapter 6 General Discussion GENERAL DISCUSSION Since their identification, starting about 15 years ago, a growing amount of data has accumulated about the structure, the expression, the ligands and, more recently, also the functional implications of EGF-TM7 receptors. Studies with antibody treatment and gene targeting in mice and antibody treatment of human cells in vitro, led to the implication of EGF-TM7 receptors in the trafficking of granulocytes, the generation of efferent antigen specific regulatory T cells and the potentiation of different granulocyte effector functions [1-4]. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Reck and Gpr124 Activate Canonical Wnt Signaling To
RECK AND GPR124 ACTIVATE CANONICAL WNT SIGNALING TO CONTROL MAMMALIAN CENTRAL NERVOUS SYSTEM ANGIOGENESIS AND BLOOD-BRAIN BARRIER REGULATION by Chris Moonho Cho A dissertation submitted to Johns Hopkins University in conformity with the requirements for the degree of Doctor of Philosophy Baltimore, Maryland July 2018 © Chris Moonho Cho 2018 All rights reserved Abstract Canonical Wnt signaling plays a pivotal role in promoting central nervous system (CNS) angiogenesis and blood-brain barrier (BBB) formation and maintenance. Specifically, Wnt7a and Wnt7b are required for vascular development in the forebrain and ventral spinal cord. Yet, how these two ligands – among the 19 mammalian Wnts – are selectively communicated to Frizzled receptors expressed on endothelial cells (ECs) remains largely unclear. In this thesis, we propose a novel paradigm for Wnt specificity. We have identified two EC surface proteins – orphan receptor Gpr124, and more recently, GPI-anchored Reck (reversion-inducing cysteine-rich protein with Kazal motifs) – as essential receptor co-factors that assemble into a multi-protein complex with Wnt7a/7b and Frizzled for the development of the mammalian neurovasculature. Specifically, we show that EC-specific reduction in Reck impairs CNS angiogenesis and that EC-specific postnatal loss of Reck, combined with loss of Norrin, impairs BBB maintenance. We identify the critical domains of both Reck and Gpr124 that are required for Wnt activity, and demonstrate that these regions are important for ii direct binding and complex formation. Importantly, weakening this interaction by targeted mutagenesis reduces Reck-Gpr124 stimulation of Wnt7a signaling in cell culture and impairs CNS angiogenesis. Finally, a soluble Gpr124 probe binds specifically to cells expressing Frizzled (Fz), Wnt7a or Wnt7b, and Reck; and a soluble Reck probe binds specifically to cells expressing Fz, Wnt7a or Wnt7b, and Gpr124. -

Targeting Lysophosphatidic Acid in Cancer: the Issues in Moving from Bench to Bedside
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by IUPUIScholarWorks cancers Review Targeting Lysophosphatidic Acid in Cancer: The Issues in Moving from Bench to Bedside Yan Xu Department of Obstetrics and Gynecology, Indiana University School of Medicine, 950 W. Walnut Street R2-E380, Indianapolis, IN 46202, USA; [email protected]; Tel.: +1-317-274-3972 Received: 28 August 2019; Accepted: 8 October 2019; Published: 10 October 2019 Abstract: Since the clear demonstration of lysophosphatidic acid (LPA)’s pathological roles in cancer in the mid-1990s, more than 1000 papers relating LPA to various types of cancer were published. Through these studies, LPA was established as a target for cancer. Although LPA-related inhibitors entered clinical trials for fibrosis, the concept of targeting LPA is yet to be moved to clinical cancer treatment. The major challenges that we are facing in moving LPA application from bench to bedside include the intrinsic and complicated metabolic, functional, and signaling properties of LPA, as well as technical issues, which are discussed in this review. Potential strategies and perspectives to improve the translational progress are suggested. Despite these challenges, we are optimistic that LPA blockage, particularly in combination with other agents, is on the horizon to be incorporated into clinical applications. Keywords: Autotaxin (ATX); ovarian cancer (OC); cancer stem cell (CSC); electrospray ionization tandem mass spectrometry (ESI-MS/MS); G-protein coupled receptor (GPCR); lipid phosphate phosphatase enzymes (LPPs); lysophosphatidic acid (LPA); phospholipase A2 enzymes (PLA2s); nuclear receptor peroxisome proliferator-activated receptor (PPAR); sphingosine-1 phosphate (S1P) 1. -

Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Supplemental Material For
Supplemental material for Epithelial to mesenchymal transition rewires the molecular path to PI3-Kinase-dependent proliferation Megan B. Salt1,2, Sourav Bandyopadhyay1,3 and Frank McCormick1 Authors Affiliations: 1-Helen Diller Family Comprehensive Cancer Center; 2-Biomedical Sciences Graduate Program, University of California San Francisco, San Francisco, California; 3-California Institute for Quantitative Biosciences, San Francisco, California. Supplemental Figure Legends Table S1. EMT associated changes in gene expression. Significantly (A) up- and (B) down- regulated genes in comparing H358-TwistER cells to control H358-GFP expressing cells treated with 100nM 4OHT for 12 days. The four columns on the right are associated with significantly upregulated genes, while the four columns furthest left described significantly downregulated genes. The first column for the up- and downregulated genes shows the Probe ID associated with each gene from the Affymetric Human Gene 1.0 ST microarrays. The gene name are shown in the next column, followed by the log2(fold change) in expression for each gene after 4OHT treatment in the H358-TwistER cells. The final column shows the p-value for each gene adjusted for the false discovery rate. Figure S1. Akt inhibition reduces serum-independent proliferation. (A) Proliferation of H358- TwistER cells with increasing concentrations (uM) of GSK-690693 (top) or MK-2206 (bottom). (B) Lysates from H358-TwistER cells treated for 48hrs in serum free media with indicated concentrations of GSK-690693 (top), or MK-2206 (bottom). Figure S2. The effects of TGFβ1 are specific to epithelial cells and lead to reduced serum- independent proliferation. (A) Proliferation of untreated (top) or TGFβ1 pre-treated (bottom) H358 and H441 cells in the presence (10%) or absence (SS) of serum. -

GPR56 in Human Cytotoxic Lymphocytes
UvA-DARE (Digital Academic Repository) Adhesion GPCRs CD97 and GPR56: From structural regulation to cellular function Hsiao, C.-C. Publication date 2015 Document Version Final published version Link to publication Citation for published version (APA): Hsiao, C-C. (2015). Adhesion GPCRs CD97 and GPR56: From structural regulation to cellular function. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:01 Oct 2021 8 Discussion Discussion This thesis describes research done on the adhesion G protein-coupled receptors (adhesion GPCRs) CD97 and GPR56. Both receptors have been intensively studied in the past, which has resulted in knowledge about their cellular distribution, ligand specificity, signaling capacity, and (patho)physiological activities (see Introduction). This and the availability of a large set of research tools, including expression constructs, monoclonal antibodies, and (not studied here) genetically modified mice, make CD97 and GPR56 useful models for studying structure–function relationships in adhesion GPCRs.