Introduction to Geriatric Anesthesia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Geriatric Medicine and Why We Need Geriatricians! by Juergen H
Geriatric Medicine and why we need Geriatricians! by Juergen H. A. Bludau, MD hat is geriatric medicine? Why is there a need for 1. Heterogeneity: As people age, they become more Wthis specialty? How does it differ from general heterogeneous, meaning that they become more and more internal medicine? What do geriatricians do differently when different, sometimes strikingly so, with respect to their they evaluate and treat an older adult? These are common health and medical needs. Imagine for a moment a group questions among patients and physicians alike. Many of 10 men and women, all 40 years old. It is probably safe internists and family practitioners argue, not unjustifiably, to say that most, if not all, have no chronic diseases, do not that they have experience in treating and caring for older see their physicians on a regular basis, and take no long- patients, especially since older adults make up almost half of term prescription medications. From a medical point of all doctors visits. So do we really need another type of view, this means that they are all very similar. Compare this physician to care for older adults? It is true that geriatricians to a group of 10 patients who are 80 years old. Most likely, may not necessarily treat older patients differently per se. But you will find an amazingly fit and active gentleman who there is a very large and important difference in that the focus may not be taking any prescription medications. On the of the treatment is different. In order to appreciate how other end of the spectrum, you may find a frail, memory- significant this is, we need to look at what makes an older impaired, and wheelchair-bound woman who lives in a adult different from a younger patient. -

Psychotropic Drug Use and Alcohol Consumption Among Older Adults in Germany: Results of the German Health Interview and Examination Survey for Adults 2008–2011
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2016-012182 on 8 October 2016. Downloaded from Psychotropic drug use and alcohol consumption among older adults in Germany: results of the German Health Interview and Examination Survey for Adults 2008–2011 Yong Du, Ingrid-Katharina Wolf, Hildtraud Knopf To cite: Du Y, Wolf I-K, ABSTRACT Strengths and limitations of this study Knopf H. Psychotropic drug Objectives: The use and combined use of use and alcohol consumption psychotropic drugs and alcohol among older adults is a ▪ among older adults in A large sample of concurrent data on medication growing public health concern and should be constantly Germany: results of the use, sociodemographic and health characteristics German Health Interview and monitored. Relevant studies are scarce in Germany. allows analyses of psychotropic drug and Examination Survey Using data of the most recent national health survey, we alcohol use on a population representative level. for Adults 2008–2011. BMJ analyse prevalence and correlates of psychotropic drug ▪ The short observation period (7 days) minimises Open 2016;6:e012182. and alcohol use among this population. recall bias concerning medication use, and doi:10.1136/bmjopen-2016- Methods: Study participants were people aged 60– quality control is ensured by checking original 012182 79 years (N=2508) of the German Health Interview and packages. Examination Survey for Adults 2008–2011. Medicines ▪ Alcohol consumption was measured by fre- ▸ Prepublication history for used during the last 7 days were documented. quency and quantity. this paper is available online. Psychotropic drugs were defined as medicines acting ▪ The use of psychotropic drugs is likely to be To view these files please on the nervous system (ATC code N00) excluding underestimated as people who are institutiona- visit the journal online anaesthetics (N01), analgesics/antipyretics (N02B), but lised and those with severe disease and psychi- (http://dx.doi.org/10.1136/ including opiate codeines used as antitussives (R05D). -

Anesthesia: the Good, the Bad, and the Elderly
ANESTHESIA: THE GOOD, THE BAD, AND THE ELDERLY Item Type Electronic Thesis; text Authors Hansen, Madeline Citation Hansen, Madeline. (2020). ANESTHESIA: THE GOOD, THE BAD, AND THE ELDERLY (Bachelor's thesis, University of Arizona, Tucson, USA). Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 25/09/2021 08:05:26 Item License http://rightsstatements.org/vocab/InC/1.0/ Link to Item http://hdl.handle.net/10150/651023 ANESTHESIA: THE GOOD, THE BAD, AND THE ELDERLY By MADELINE JOLLEEN HANSEN ____________________ A Thesis Submitted to The Honors College In Partial Fulfillment of the Bachelors degree With Honors in Physiology THE UNIVERSITY OF ARIZONA M A Y 2 0 2 0 Approved by: ____________________________ Dr. Zoe Cohen Department of Physiology Table of Contents Page number(s) Abstract……………………………………………………………………………………………………..2 General History of Anesthesia.………………………………………………………………………….3-14 Prehistoric-200AD…………………………………………………………….………………....3-5 200AD- 1846 (historical surgery)…………………….………………………………………….5-8 1847-1992……………………...…………………….……………………………………...….9-14 Physiology of General Anesthesia………………………………………………………...…………...14-16 Understanding of anesthesia mechanism…………………………………………………………14 System impacts………………………………………………………………………………..15-16 Description -

001-017-Anesthesia.Pdf
Current Fluid Therapy Topics and Recommendations During Anesthetic Procedures Andrew Claude, DVM, DACVAA Mississippi State University Mississippi State, MS • Intravenous fluid administration is recommended during general anesthesia, even during short procedures. • The traditional IV fluid rate of 10 mls/kg/hr during general anesthesia is under review. • Knowledge of a variety of IV fluids, and their applications, is essential when choosing anesthetic protocols for different medical procedures. Anesthetic drug effects on the cardiovascular system • Almost all anesthetic drugs have the potential to adversely affect the cardiovascular system. • General anesthetic vapors (isoflurane, sevoflurane) cause a dose-dependent, peripheral vasodilation. • Alpha-2 agonists initially cause peripheral hypertension with reflex bradycardia leading to a dose-dependent decreased patient cardiac index. As the drug effects wane, centrally mediated bradycardia and hypotension are common side effects. • Phenothiazine (acepromazine) tranquilizers are central dopamine and peripheral alpha receptor antagonists. This family of drugs produces dose-dependent sedation and peripheral vasodilation (hypotension). • Dissociative NMDA antagonists (ketamine, tiletamine) increase sympathetic tone soon after administration. When dissociative NMDA antagonists are used as induction agents in patients with sympathetic exhaustion or decreased cardiac reserve (morbidly ill patients), these drugs could further depress myocardial contractility. • Propofol can depress both myocardial contractility and vascular tone resulting in marked hypotension. Propofol’s negative effects on the cardiovascular system can be especially problematic in ill patients. • Potent mu agonist opioids can enhance vagally induced bradycardia. Why is IV fluid therapy important during general anesthesia? • Cardiac output (CO) equals heart rate (HR) X stroke volume (SV); IV fluids help maintain adequate fluid volume, preload, and sufficient cardiac output. -

Fundamentals of Geriatric Pharmacotherapy, 2Nd Edition
PART 1 Social, Ethical, and Economic Issues of Aging 1 Challenges in Geriatric Care REBECCA B. SLEEPER Learning Objectives 1. Evaluate the applicability of clinical literature to the elderly patient using an approach that is tailored to specific subgroups of the geriatric population. 2. Differentiate the roles of healthcare professionals and the various services and venues available in the care of geriatric patients. 3. Infer scenarios in which geriatric patients are at risk for suboptimal care and intervene when breakdowns in the continuum of care are identified. 4. Recognize the impact of caregiver burden on patient outcomes. Key Terms and Definitions ASSISTED LIVING FACILITY: Living environment that provides added services to the individual who is safe to live in the community environment but requires some assistance with various daily activities. CAREGIVER BURDEN: Psychosocial and physical stress experienced by an individual who provides care to another person. CERTIFIED GERIATRIC PHARMACIST: Pharmacist who has achieved certification from the Commission for Certification in Geriatric Pharmacy. CERTIFIED NURSE’S ASSISTANT: Individual who has earned a certificate to practice as a nurse’s assistant and who may work in a wide variety of healthcare settings ranging from long-term care facilities to private homes. GERIATRIC: Adjective generally used to refer to an older individual. GERIATRICIAN: Physician with expertise, as demonstrated by fellowship or other added qualifications, in the care of older persons. GERONTOLOGICAL NURSE: Nurse with expertise, as demonstrated by exam or other added qualifications, in the care of older persons. 4 | Fundamentals of Geriatric Pharmacotherapy INFORMAL CAREGIVER: An individual who does not have formal training as a healthcare professional but who provides daily care to another individual; usually unpaid. -

Partnership for Health in Aging
Partnership FOR HealthiN Aging Multidisciplinary Competencies in the Care of Older Adults at the Completion of the Entry-level Health Professional Degree Preface In June 2008, the American Geriatrics Society convened a A workgroup of healthcare professionals with experience meeting of 21 organizations representing healthcare pro- in competency development, certification, and accredita- fessionals who care for older adults to discuss how these tion was convened in February 2009. Workgroup mem- organizations could work together to: bers represent ten healthcare disciplines: • advance recommendations from the 2008 Institute • Dentistry of Medicine Report, Retooling for an Aging America: • Medicine Building the Health Care Workforce, and • Nursing • advocate for ways to meet the healthcare needs of the • Nutrition nation’s rapidly growing older population. • Occupational Therapy This meeting led to the development of a loose coalition – • Pharmacy the Partnership for Health in Aging (PHA) – that identi- • Physical Therapy fied as its first step the development of a set of core com- • Physician Assistants petencies in the care of older adults that are relevant to and • Psychology can be endorsed by all health professional disciplines. • Social Work The workgroup began with a comprehensive matrix of The workgroup reviewed all comments received, and competencies across these ten disciplines. (Note: These developed the final set of competencies on the following disciplines are currently at different stages in developing page. The set describes essential skills that healthcare discipline-specific geriatrics competencies). Through an professionals in the above ten disciplines should have, iterative process, the workgroup drafted a set of baseline and necessary approaches they should master, by the time competencies that were circulated among more than they complete their entry-level degree, in order to provide 25 professional organizations for review and comment. -

Do Complexity Measures of Frontal EEG Distinguish Loss of Consciousness in Geriatric Patients Under Anesthesia?
UCLA UCLA Previously Published Works Title Do Complexity Measures of Frontal EEG Distinguish Loss of Consciousness in Geriatric Patients Under Anesthesia? Permalink https://escholarship.org/uc/item/63j9k57t Authors Eagleman, Sarah L Vaughn, Don A Drover, David R et al. Publication Date 2018 DOI 10.3389/fnins.2018.00645 Peer reviewed eScholarship.org Powered by the California Digital Library University of California fnins-12-00645 September 18, 2018 Time: 16:50 # 1 ORIGINAL RESEARCH published: 20 September 2018 doi: 10.3389/fnins.2018.00645 Do Complexity Measures of Frontal EEG Distinguish Loss of Consciousness in Geriatric Patients Under Anesthesia? Sarah L. Eagleman1*†, Don A. Vaughn2,3*†, David R. Drover1, Caitlin M. Drover4, Mark S. Cohen2,5, Nicholas T. Ouellette6 and M. Bruce MacIver1 1 Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University, Palo Alto, CA, United States, 2 UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles, CA, United States, 3 Department of Psychology, University of Santa Clara, Santa Clara, CA, United States, 4 University of Washington, Seattle, WA, United States, 5 UCLA Departments of Psychiatry, Neurology, Radiology, Psychology, Biomedical Physics and Bioengineering, California Nanosystems Institute, Los Angeles, CA, United States, 6 Department of Civil and Environmental Engineering, Stanford Edited by: University, Stanford, CA, United States Kay Jann, University of Southern California, United States While geriatric patients have a high likelihood of requiring anesthesia, they carry an Reviewed by: increased risk for adverse cognitive outcomes from its use. Previous work suggests this Keiichiro Nishida, could be mitigated by better intraoperative monitoring using indexes defined by several Kansai Medical University, Japan Thomas Koenig, processed electroencephalogram (EEG) measures. -

Syllabus on Geriatric Anesthesiology Version 1/10/02 Final
Syllabus on Geriatric Anesthesiology Version 1/10/02 final Disclaimer The opinions expressed in this document represent those of the authors. The purpose of the document is to educate physicians and others about anesthetic issues pertinent to the elderly population. The document specifically does not purport to provide practice guidelines. The text is not intended to be comprehensive and any apparent anesthetic management suggestions will not apply to all patient situations. Introduction One of the goals of the ASA Committee on Geriatric Anesthesia is to promote education of residents and anesthesiologists about those aspects of aging that affect anesthetic practice. This syllabus is our attempt to provide basic information useful to all anesthesia practitioners. Chapters are deliberately short in order to force focus on the important issues. More detailed information can easily be obtained from the references at the end of each chapter. You are free to use this syllabus as you see fit for your colleagues', your residents' and your own education. You may make copies of all or part of the syllabus, so long as it is not used for commercial purposes. Please give appropriate credit to the authors whose work you use. The syllabus should be considered a work in progress. With the availability of the syllabus through the ASA Web site, all ASA members will have immediate access to the latest revision. Chapters may be added or deleted, and existing chapters will change as new information becomes available or revisions are made for clarity. Your comments and suggestions are welcome and can be addressed to me. -

GERIATRIC MEDICINE What Is Geriatric Medicine?
GERIATRIC MEDICINE What is Geriatric Medicine? Geriatrics is the branch of medicine that focuses on health promotion, prevention, and diagnosis and treatment of disease and disability in older adults. In recent surveys, geriatricians are among the most satisfied physicians in terms of their choice of specialty. Geriatrics offers a wide diversity of career options and is a clinically and intellectually rewarding discipline given the medical complexity of older adults. Geriatricians reap the rewards of making a difference in a patient’s level of independence, well- being and quality of life. With the rapid growth of the older population in the United States, there is a pressing demand for physicians with specialized training in geriatrics. ama-assn.org/specialty/geriatric-medicine The Birth of “Geriatric” Medicine • In 1909, Austrian born physician, Ignatz Leo Nascher coined the term “geriatrics” for care of the elderly, explaining, “Geriatrics, from geras, old age, and iatrikos, relating to the physician, is a term I would suggest as an addition to our vocabulary, to cover the same field in old age that is covered by the term pediatrics in childhood, to emphasize the necessity of considering senility and its disease apart from maturity and to assign it a separate place in medicine.” • Until Nascher’s time, older adults were not treated differently or in different ways than other adult patients. Social forces came into play in the period during WWI and WWII that both necessitated and facilitated long-term care for the elderly: The number of elderly people began to increase due to improvements in economic conditions and medicine. -

Perioperative Management of Geriatric Patients for Orthopedic Surgeries
International Journal of Research in Orthopaedics Krishna B et al. Int J Res Orthop. 2020 Mar;6(2):427-434 http://www.ijoro.org DOI: http://dx.doi.org/10.18203/issn.2455-4510.IntJResOrthop20200749 Review Article Perioperative management of geriatric patients for orthopedic surgeries Bhavya Krishna, Nidhi Pathak* Department of Anesthesia, VMMC and Safdarjung Hospital, New Delhi, India Received: 31 January 2020 Revised: 13 February 2020 Accepted: 15 February 2020 *Correspondence: Dr. Nidhi Pathak, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT With increasing life expectancy, the mean age of patient orthopedicians and anesthesiologists have to deal with is increasing. In this review article, we discuss the case management of three centurions aged 110, 105 and 102 years respectively who underwent lower limb orthopedic surgery under nerve block, general anesthesia and neuraxial blockade, and elaborate on the various issues faced perioperatively by the treating team. The challenges and differences faced in perioperative period in geriatric anesthesia were discussed and literature reviewed for the benefit of the operating surgeons. Keywords: Geriatric, Orthopedic, Fracture, Anesthesia INTRODUCTION hemiarthroplasty. Appropriate anesthetic assessment was done and there was no positive history of any systemic With increasing life expectancy, both orthopedicians and illness except anemia (hemoglobin (Hb) 9 gm%, anesthesiologists now have to be confident in handling hematocrit (HCT) 27%). The rest of the investigations geriatric cases. -

Parkinsons & Huntington Disease
conferenceseries.com 4th World Congress on Parkinsons & Huntington Disease August 29-30, 2018 Zurich, Switzerland SCIENTIFIC PROGRAM SCIENTIFIC PROGRAM DAY 1 Wednesday, 29th August 08:30-09:00 Registrations 09:00-09:30 Introduction 09:30-09:50 COFFEE BREAK 09:50-11:50 KEYNOTE LECTURES Meeting Hall 01 MEETING HALL 01 11:50-13:10 Talks On: Parkinson Disease Epidemiology of Parkinsons Neuromuscular Disorders 13:10-13:15 GROUP PHOTO 13:15-14:00 LUNCH BREAK MEETING HALL 01 14:00-16:00 Talks On: Huntington Disease Risk Factors of Parkinson’s disease Pathophysiology and Pharmacology Diagnosis for Parkinson’s disease 16:00-16:20 COFFEE BREAK MEETING HALL 01 (16:20-17:00) Parkinson’s disease: Complications Visit: https://parkinsons.neurologyconference.com/ SCIENTIFIC PROGRAM DAY 2 Thursday, 30th August 09:00-10:30 KEYNOTE LECTURES Meeting Hall 01 10:30-10:50 COFFEE BREAK MEETING HALL 01 10:50-12:50 Talks On: Mitochondrial Dysfunction Insights and Therapeutics: Parkinson’s Disease Managing life with Parkinson’s Disease 12:50-13:35 LUNCH BREAK MEETING HALL 01 13:35-15:55 Talks On: Neurosurgery Free Radicles and Aging in Parkinsons Novel Therapeutics Clinical Trials in Parkinsonism 15:55-16:15 COFFEE BREAK Visit: https://parkinsons.neurologyconference.com/ 4th World Congress on Parkinsons & Huntington Disease AUGUST 29-30, 2018 | ZURICH, SWITZERLAND AGENDA Title: Neuroinflammation, Microglia and Mast Cells in the Pathophysiology of Dr. Sanchez-Ramos received a Ph.D. in Pharmacology and Physiology from Juan Sanchez-Ramos the University of Chicago and a medical degree (M.D.) from the University of University of South Illinois. -
The 5Ms of Geriatrics
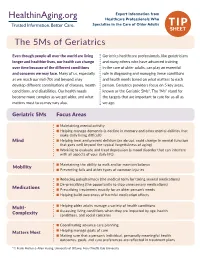
Expert Information from Healthcare Professionals Who Specialize in the Care of Older Adults TIP SHEET The 5Ms of Geriatrics Even though people all over the world are living Geriatrics healthcare professionals, like geriatricians longer and healthier lives, our health can change and many others who have advanced training over time because of the different conditions in the care of older adults, can play an essential and concerns we may face. Many of us, especially role in diagnosing and managing these conditions as we reach our mid-70s and beyond, may and health needs based on what matters to each develop different combinations of diseases, health person. Geriatrics providers focus on 5 key areas, conditions, and disabilities. Our health needs known as the Geriatric 5Ms*. The “Ms” stand for become more complex as we get older, and what the targets that are important to care for us all as matters most to us may vary also. we age. Geriatric 5Ms Focus Areas n Maintaining mental activity n Helping manage dementia (a decline in memory and other mental abilities that make daily living difficult) Mind n Helping treat and prevent delirium (an abrupt, rapid change in mental function that goes well beyond the typical forgetfulness of aging) n Working to evaluate and treat depression (a mood disorder that can interfere with all aspects of your daily life) n Maintaining the ability to walk and/or maintain balance Mobility n Preventing falls and other types of common injuries n Reducing polypharmacy (the medical term for taking several medications)