Cutaneous Mucinoses: an Overview Aefan Ul Bari
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Discrete Papular Mucinosis: a Rare Subtype of Lichen Myxedematosus Wongsiya Viarasilpa MD, Wareeporn Disphanurat MD
198 Case report Thai J Dermatol, October-December, 2019 Discrete papular mucinosis: A rare subtype of lichen myxedematosus Wongsiya Viarasilpa MD, Wareeporn Disphanurat MD. ABSTRACT: VIARASILPA W, DISPHANURAT W. DISCRETE PAPULAR MUCINOSIS: A RARE SUBTYPE OF LICHEN MYXEDEMATOSUS. THAI J DERMATOL 2019; 35: 198-205. DIVISION OF DERMATOLOGY, DEPARTMENT OF MEDICINE, FACULTY OF MEDICINE, THAMMASAT UNIVERSITY, PATHUMTHANI, THAILAND. Lichen myxedematosus is a chronic, progressive idiopathic cutaneous mucinosis characterized by localized or generalized papular eruption of unknown etiology in which mucin deposition in the dermis is the distinctive histologic feature. The classification system was revised into three clinicopathological subsets, localized lichen myxedematosus, scleromyxedema and atypical forms of lichen myxedematosus. We report a rare subtype of lichen myxedematosus, discrete papular subtype, presented with papular eruption on the back, chest, face and neck. Histopathology showed focal mucin accumulation in upper and mid reticular dermis with scattered stellate fibroblasts among mucinous material, confirmed by Alcian blue staining. Her serum protein electrophoresis showed polyclonal immunoglobulin, serology for hepatitis C and HIV were negative and her thyroid function test was normal. She was diagnosed with localized forms of lichen myxedematosus, discrete papular subtype and was treated with an excellent response to topical corticosteroids and oral hydroxychloroquine combination therapy. Key words: lichen myxedematosus, papular mucinosis, skin-colored papules From: Division of dermatology, Department of Medicine, Faculty of Medicine, Thammasat University, Pathumthani, Thailand Corresponding author: Wareeporn Disphanurat MD, email: [email protected] Received: 2 April 2019 Revised: 23 September 2019 Accepted: 6 November 2019 Vol.35 No.4 Viarasilpa W and Disphanurat W 199 myxedematosus is a rare entity and has less prevalence than scleromyxedema4, 6-12. -

Atypical Lichen Myxedematosus with an Interstitial Granulomatous Pattern; a Difficult Case in Making Diagnosis Chanida Ungaksornpairote MD, Punkae Mahaisawariya MD
Vol.34 No.3 Case report 207 Atypical Lichen Myxedematosus with an Interstitial Granulomatous Pattern; A Difficult Case in Making Diagnosis Chanida Ungaksornpairote MD, Punkae Mahaisawariya MD. ABSTRACT: UNGAKSORNPAIROTE C, MAHAISAWARIYA P. ATYPICAL LICHEN MYXEDEMATOSUS WITH AN INTERSTITIAL GRANULOMATOUS PATTERN; A DIFFICULT CASE IN MAKING DIAGNOSIS. THAI J DERMATOL 2018; 34: 207-216. DEPARTMENT OF DERMATOLOGY, FACULTY OF MEDICINE SIRIRAJ HOSPITAL, MAHIDOL UNIVERSITY, BANGKOK, THAILAND. Lichen myxedematosus (LM) is characterized by multiple discrete papules with shiny surface and area of induration caused by mucin deposition. There are 3 subtypes including the generalized papular and sclerodermoid form or scleromyxedema, the localized papular form, and the atypical or intermediate form. Histological characteristics can be classical mucin deposition or rare interstitial granuloma annulare variant. The authors report an atypical case of LM with an interstitial granuloma histologic pattern which was rare and difficult to make a diagnosis. Key words: Atypical lichen myxedematosus, scleromyxedema, interstitial granulomatous From: Department of Dermatology, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand Corresponding author : Chanida Ungaksornpairote MD., email : [email protected] 208 Ungaksornpairote C et al Thai J Dermatol, July-September 2018 บทคัดยอ: ชนิดา อึ้งอักษรไพโรจน พรรณแข มไหสวริยะ โรคไลเคนมิกซิดีมาโตซุส ชนิดไมปกติ (ATYPICAL LICHEN MYXEDEMATOSUS) ที่มีลักษณะทางพยาธิวิทยาเปนแบบแกรนูโลมา ซึ่งยากตอการวินิจฉัย -

Mucinous Disorders of the Skin-Beyond the Dermal Mucinosis
Mucinous Disorders of the Skin- Don’t GAG me! Paul K. Shitabata, M.D. Dermatopathology Institute Thursday, May 23, 13 Thursday, May 23, 13 Thursday, May 23, 13 Thursday, May 23, 13 Glycosaminoglycans (GAGs) Unbranched polysaccharides containing a repeating disaccharide unit, either of two modified sugars--- N-acetylgalactosamine (GalNAc) or N- acetylglucosamine (GlcNAc) and a uronic acid such as glucuronate or iduronate Imparts high viscosity to the solution and allows for lubrication and structural integrity for cells Specific GAGs of physiological significance Hyaluronic acid Dermatan sulfate Chondroitin sulfate Heparin Heparan sulfate Keratan sulfate Thursday, May 23, 13 Proteoglycans (Mucopolysaccharides) Majority of GAGs in the body are linked to core proteins, forming proteoglycans GAGs extend perpendicularly from the core Linkage of GAGs to the protein core involves a specific trisaccharide composed of two galactose residues and a xylulose residue (GAG-GalGalXyl-O-CH2- protein) Trisaccharide linker is coupled to the protein core through an O- glycosidic bond to a S residue in the protein Thursday, May 23, 13 Thursday, May 23, 13 Thursday, May 23, 13 Mucinous Dermal Disorders Considered Primary Generalized myxedema Pretibial myxedema Reticular erythematous mucinosis Scleredema Scleromyxedema Papular mucinosis Acral persistent papular mucinosis Focal mucinosis Digital mucous cyst Mucocele Cutaneous myxoma Cutaneous mucinosis of infancy Nevus mucinosis Alopecia mucinosa (Follicular mucinosis) Mucopolysaccharidoses Thursday, -

UC Davis Dermatology Online Journal
UC Davis Dermatology Online Journal Title Mucin in the dermis: a case of tender tumors Permalink https://escholarship.org/uc/item/4b50f4zf Journal Dermatology Online Journal, 22(8) Authors Ferris, Gina J Spohn, Gina P Gru, Alejandro et al. Publication Date 2016 DOI 10.5070/D3228032182 License https://creativecommons.org/licenses/by-nc-nd/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California Volume 22 Number 8 August 2016 Case Presentation Mucin in the dermis: a case of tender tumors Gina J. Ferris 1 BA, Gina P. Spohn 1 MD, Alejandro Gru2 MD, Jessica Kaffenberger 1 MD Dermatology Online Journal 22 (8): 10 1 Department of Internal Medicine, Division of Dermatology, The Ohio State University Wexner Medical Center 2 Departments of Pathology and Dermatology, University of Virginia Correspondence: Jessica Kaffenberger Division of Dermatology Department of Internal Medicine The Ohio State University Wexner Medical Center 540 Officenter Place, Suite 240 Gahanna, OH 43230 Tel. 614-293-1707 Fax. 614-293-1716 Email: [email protected] Abstract We present an original case report of a 45-year-old woman with a five-month history of sporadic, tender, nodules present on the right upper abdomen, bilateral dorsal wrists, right upper arm, and left flank. Biopsy revealed a mild perivascular infiltrate, increased dermal mucin, and no significant increase in fibroblasts. Presentation and histology were most consistent with nodular lichen myxedematosus (NLM), a rare primary mucinosis. Only four previous cases are reported in the literature to our knowledge. Management of NLM and other subtypes of lichen myxedematosus is not well described. -

Adult Variant of Self-Healing Cutaneous Mucinosis in a Patient with Epilepsy
CASE REPORT Adult Variant of Self-healing Cutaneous Mucinosis in a Patient with Epilepsy Reza Yaghoobi1, Arezou Bagherzade1, Maryam Aliabdi1, Parvin Kheradmand2, Afshin Kazerouni1, Amir Feily3 1 Department of Dermatology, Ahvaz, Jundishapur University of Medical Sciences, Ahvaz, Iran. 2 Department of Pathology, ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran. 3 Skin and Stem Cell Research Center, Tehran University of Medical Sciences, Tehran, Iran. Corresponding Author: Arezou Bagherzade, MD. Department of Dermatology, Imam Khomeini Hospital, 61335, Ahvaz, Iran. email: [email protected]. ABSTRAK Seorang wanita 52 tahun memiliki riwayat periorbital edema dan bibir bengkak selama 3 minggu. Dia mengalami beberapa papula eritematosa padat subkutan dan nodul pada wajah, kulit kepala dan dua plak di punggung atas dan lengan kiri. Lesi ini berkembang pesat. Pasien memiliki riwayat serangan epilepsi sejak kecil. Pemeriksaan umum normal. Terdapat edema ringan pada tangan dan kaki, dan data laboratorium normal. Pemeriksaan histopatologi menunjukkan adanya akumulasi musin berbatas tegas pada lapisan dermis, dengan pulasan alsian biru positif. Temuan klinis dan histopatologi diikuti oleh resolusi spontan lesi dalam jangka waktu 4 bulan yang sesuai dengan diagnosis mucinosis kulit yang sembuh sendiri. Kami melaporkan pertama kalinya kasus mucinosis kulit yang berhubungan dengan epilepsi. Kata kunci: epilepsi, mucinosis, penyembuhan sendiri. ABSTRACT A 52-year-old woman was admitted with a 3 weeks history of periorbital edema and lips swelling. She developed several subcutaneous firm erythematous papules and nodules on the face, scalp and two indurated plaques on the upper back and left forearm. These lesions grew rapidly. The patient had a positive history of epileptic seizures since childhood. General examination was normal. -
Discrete Papular Lichen Myxedematosus with an Unusual Segmental Presentation
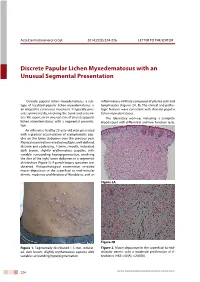
Acta Dermatovenerol Croat 2014;22(3):224-226 LETTER TO THE EDITOR Discrete Papular Lichen Myxedematosus with an Unusual Segmental Presentation Discrete papular lichen myxedematosus, a sub- inflammatory infiltrate composed of plasma cells and type of localized papular lichen myxedematosus, is lymphocytes (Figures 2A, B). The clinical and patho- an idiopathic cutaneous mucinosis. It typically pres- logic features were consistent with discrete papular ents symmetrically, involving the trunk and extremi- lichen myxedematosus. ties. We report on an unusual case of discrete papular The laboratory work-up, including a complete lichen myxedematosus with a segmental presenta- blood count with differential and liver function tests, tion. An otherwise healthy 23-year-old man presented with a gradual accumulation of asymptomatic pap- ules on the lower abdomen over the previous year. Physical examination revealed multiple, well-defined, discrete and coalescing, 1-5mm, smooth, indurated, dark brown, slightly erythematous papules, with variable surrounding hyperpigmentation, involving the skin of the right lower abdomen in a segmental distribution (Figure 1). A punch biopsy specimen was obtained. Histopathological examination revealed mucin deposition in the superficial to mid-reticular dermis, moderate proliferation of fibroblasts, and an Figure 2A. Figure 2B Figure 1. Segmentally distributed 1-5 mm, indurat- Figure 2. Mucin deposition in the superficial to mid- ed, dark brown, slightly erythematous papules with reticular dermis with a moderate proliferation of fi- variable surrounding hyperpigmentation. broblasts (H&E ×40(A), ×200(B)). 224 ACTA DERMATOVENEROLOGICA CROATICA Letter to the editor Acta Dermatovenerol Croat 2014;22(3):224-226 renal panel, and serum protein electrophoresis, was within normal limits. -

Lichen Myxedematosus: a Rare Group of Cutaneous Mucinosis*
462462Particular characteristicsSoares de Sá BC, of atopicMoredo eczema LF, Gomes in tropical EE, de environments. Araújo ESS, DupratTheREVIEW Tropical JP Environment... 462 s Lichen myxedematosus: a rare group of cutaneous mucinosis* Ramiro Eugenio Cárdenas-Gonzalez1, Maira Elizabeth Herz Ruelas1, Jorge Ocampo Candiani1 DOI: http://dx.doi.org/10.1590/abd1806-4841.20198478 Abstract: Cutaneous mucinoses are a heterogeneous group of dermatoses in which excess deposition of mucin in the dermis gives the skin a waxy appearance, with papules and plaques that can vary from self-healing mucinosis to even disrupting the normal shape of a patient’s face, conferring a leonine facies, or be part of life threatening diseases like scleromyxedema. This review will describe the most recent classification on lichen myxedematosus in the generalized (scleromyxedema) and the localized forms, as well as the different organ systems involved in scleromyxedema, diagnostic workup, current management, and prognosis. Keywords: Glycosaminoglycans; Mucinoses; Mucins; Scleromyxedema INTRODUCTION Cutaneous mucinoses are a heterogeneous group of skin di- in 1953, Montgomery and Underwood distinguished scleromyxe- sorders characterized by an abnormal dermal deposition of mucin. dema from scleroderma and generalized myxedema, describing Mucin is composed of glycosaminoglycans, hyaluronic acid, and four different clinical patterns, a generalized lichenoid eruption, a dermatan sulfate. It is a component of the extracellular matrix and discrete papular form, a localized -

Papular Mucinosis Is a Variety of Mucinosis Characterized by Excessive Production of Mucin by Fibroblasts and Deposition in the Dermis
Our Dermatology Online Original Article PPapularapular mmucinosisucinosis ((papularpapular llichenichen mmyxedematosus):yxedematosus): CClinicallinical aandnd hhistopathologicalistopathological eevaluationvaluation Khalifa Sharquie1, Raed I Jabbar2 1Department of Dermatology, College of Medicine, University of Baghdad. Medical City Teaching Hospital, Baghdad, Iraq, 2Department of Dermatology, Falluja Teaching Hospital, Al-Anbar Health Directorate, Anbar, Iraq. Corresponding author: Prof. Khalifa Sharquie, MD, PhD, FRCP Edin. E-mail: [email protected] ABSTRACT Background: Papular mucinosis is a variety of mucinosis characterized by excessive production of mucin by fibroblasts and deposition in the dermis. It manifests itself with fleshy papules or plaques in different sites of the body and taking different clinical morphological cutaneous features. Objective: The objective is to report and evaluate the different clinical and histopathological features of the disease in Iraqi patients. Patients and Methods: This is a case series and a clinical descriptive study in which ten patients with papular mucinosis were reported during the period from 2012 through 2019. The age ranged from 4 to 56 years, with seven females and three males. Clinical evaluation regarding histories of the disease and examination was carried out. General investigation was done and skin biopsy for histopathological assessment was conducted. Results: Nine patients were adults, with their age ranging from 20 to 56 years, a mean of around 35 years, and only one 4-year-old child. It is a disease with a female predominance, as observed in 7 (70%) females. The common sites of involvement were the face but the rash may extend to affect the neck and upper arms. The rash appeared in the form of skin-colored or red fleshy papules and plaques or in diffuse erythematous orange peel-like forms. -

Self-Healing Cutaneous Mucinosis in an Adult
Case Report DOI: 10.6003/jtad.1372c4 Self-healing Cutaneous Mucinosis in an Adult Göknur Kalkan,1 MD, Gülfer Akbay,2 MD, Meral Ekşioğlu,2 MD, Müzeyyen Astarcı,3 MD Address: 1Department of Dermatology, Gaziosmanpasa University School of Medicine, Tokat, Turkey, 2Departments of Dermatology and 3Pathology, Ankara Education and Research Hospital, Ministry of Health, Turkey E-mail: [email protected] * Corresponding Author: Dr.Göknur Kalkan,Department of Dermatology, Gaziosmanpaşa University School of Medicine, Tokat, Turkey Published: J Turk Acad Dermatol 2013; 7 (2): 1372c4 This article is available from: http://www.jtad.org/2013/2/jtad1372c4.pdf Key Words: Self healing, cutaneous mucinosis, adult Abstract Observations: Self-healing cutaneous mucinosis is a localized form of primary cutaneous mucinosis characterized by an early age of onset, the presence of plaques and nodules in a typical distribution, and rapid onset followed by spontaneous resolution of the lesions within a period of weeks to months. Histopathologically cutaneous mucinosis is defined by mucin deposits in the dermis. Here we present a clinically and histopathologically proven case of 25-year-old male patient with a 1-year history of papuler eruption on his elbows and dorsum of the feet. Introduction Cutaneous mucinosis includes a heteroge- neous group of diseases in which acid glyco- saminoglycans (mucin) accumulate either diffusely or locally in the skin or within the hair follicle [l]. Self-healing cutaneous muci- nosis is a localized form of primer cutaneous mucinosis and firstly described by Colomb et al. [2] in 1973. In 1980 Bonerandi et al. [3] re- ported an additional case and referred to two other reported cases with similar features. -

A Rare Variant of Connective Tissue Naevus
J Interdiscipl Histopathol 2013; 1(2): 89-92 ISSN: 2146-8362 Case Report Mucinous Naevus: A Rare Variant of Connective Tissue Naevus Bhavna Nayal1, Mary Mathew1, Pramod Kumar2, Rajesh P Nair3 Departments of Pathology1, Plastic Surgery2 and Surgery3, Kasturba Medical College, Manipal University, Manipal, India Received: January 15, 2013 Abstract Accepted: January 16, 2013 Mucinous naevus is a rare benign hamartomatous lesion which has been categorized as a variant of both cutaneous mucinosis and connective tissue neavus. These lesions commonly involve the trunk Published Online: January 28, 2013 and extremities, appearing as papulonodular or plaque-like lesions. We present a 22 year old boy with congenital mucinous nevus presenting with mole-like lesion on the face. DOI: 10.5455/jihp.20130116111804 Corresponding Author: Mary Mathew, Kasturba Medical College, Manipal University, Manipal, India [email protected] Keywords: Cutaneous mucinoses, mucin, naevus © 2013 GESDAV INTRODUCTION elongated rete ridges overlying papillary and reticular dermis containing clusters of nevus cells separated by Mucinous naevus (MN) is a type of benign widely spaced collagen fibers and increased mucin hamartomatous cutaneous mucinoses characterized by deposition (Figure 1). The mucin was positive for deposition of excessive amounts of mucin in the Alcian blue at pH 2.5 and toluidine blue (Figure 2a and superficial dermis in a diffuse pattern with absence of b) and negative for mucicarmine (Figure 2c) and collagen and elastic fibres in the mucinous areas. It periodic-acid Schiff (PAS). Van Gieson stain revealed may be associated with features of connective tissue absence of elastic fibres in the dermis (Figure 3). A naevus of proteoglycan type [1].