The Association Between Zolpidem and Infection in Patients with Sleep Disturbance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
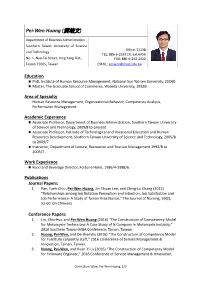
Pei-Wen Huang (黃培文)
Pei‐Wen Huang (黃培文) Department of Business Administration Southern Taiwan University of Science Office: T1138 and Technology TEL: 886‐6‐2533131 ext.6456 No. 1, Nan‐Tai Street, Yong Kang Dist., FAX: 886‐6‐242‐2420 Tainan 71005, Taiwan EMAIL: [email protected] Education PhD, Institute of Human Resource Management, National Sun Yat‐sen University, 2004/6 Master, The Graduate School of Commerce, Waseda University, 1992/3 Area of Specialty Human Resource Management, Organizational Behavior, Competency Analysis, Performance Management Academic Experience Associate Professor, Department of Business Administration, Southern Taiwan University of Science and Technology, 2009/8 to present Associate Professor, Institute of Technological and Vocational Education and Human Resources Development, Southern Taiwan University of Science and Technology, 2005/8 to 2009/7 Instructor, Department of Leisure, Recreation and Tourism Management 1992/8 to 2005/7 Work Experience Food and Beverage Director, Fortune Hotel, 1986/4‐1988/6. Publications Journal Papers: 1. Pan, Yueh‐Chiu, Pei‐Wen Huang, Jin‐Chuan Lee, and Ching‐Lu Chang (2012) “Relationships among Job Rotation Perception and Intention, Job Satisfaction and Job Performance: A Study of Tainan Area Nurses,” The Journal of Nursing, 59(2), 51‐60. (in Chinese) Conference Papers: 1. Lin, Chia‐Hui, and Pei‐Wen Huang (2016) “The Construction of Competency Model for Motorcycle Technicians‐A Case Study of N Company in Motorcycle Industry,” 2016 Southern Taiwan MBA Conference, Tainan, Taiwan. 2. Huang, Pei‐Wen, and De‐JhenWu (2016) “The Construction of Competency Model for Furniture carpentry staff,” 2016 Conference of Service Management & Innovation, Tainan, Taiwan. 3. Huang, Pei‐Wen, and Kuan‐Yi Lu (2016) “The Construction of Competency Model for Firmware Engineer,” 2016 Conference of Service Management & Innovation, Curriculum Vitae, Pei‐Wen Huang, 1/5 Tainan, Taiwan. -

Healthy Cities in Taiwan
Healthy Cities in Taiwan Content 1. Development of healthy cities in Taiwan 2 2. Promotional models for healthy cities in Taiwan 3 3. Taiwan healthy city indicators 3 4. Taiwan healthy cities network 5 5. Taiwan Healthy City A wards 6 Appendix 13 I. Themes of Awards and Awardees for the First Taiwan Healthy City Award II. Themes of Awards and Awardees for the Second Taiwan Healthy City Award III. \Contact information and websites of healthy cities in Taiwan Commission: Bureau of Health Promotion, Department of Health, Taiwan Compile and Print: Healthy City Research Center, National Cheng Kung University October 2010 1. Development of healthy cities in Taiwan The healthy cities movement began in 1986. It was first promoted by the WHO Regional Office for Europe, and primarily targeted European cities. After almost two decades of work, the results have been very good, and European healthy cities are now exemplars for the world. As a result, WHO regional offices have started to advocate healthy cities for each of their regions. In Taiwan, the Republic of China decided to participate in the healthy cities movement in the beginning of the new Millennium. The Bureau of Health Promotion (BHP), Department of Health called for a pilot proposal in 2003, a cross-disciplinary team of scholars at National Cheng Kung University won the project, and found collaboration from Tainan City, thus, pioneered the healthy city development in Taiwan. BHP has since continued to fund other local authorities to promote healthy cities, including Miaoli County, Hualien County, Kaohsiung City and Taipei County. Since the results have been excellent, some other counties and cities have also allotted budgets to commission related departments for implementation. -

Atmospheric PM2.5 and Polychlorinated Dibenzo-P-Dioxins and Dibenzofurans in Taiwan
Aerosol and Air Quality Research, 18: 762–779, 2018 Copyright © Taiwan Association for Aerosol Research ISSN: 1680-8584 print / 2071-1409 online doi: 10.4209/aaqr.2018.02.0050 Atmospheric PM2.5 and Polychlorinated Dibenzo-p-dioxins and Dibenzofurans in Taiwan Yen-Yi Lee 1, Lin-Chi Wang2*, Jinning Zhu 3**, Jhong-Lin Wu4***, Kuan-Lin Lee1 1 Department of Environmental Engineering, National Cheng Kung University, Tainan 70101, Taiwan 2 Department of Civil Engineering and Geomatics, Cheng Shiu University, Kaohsiung 83347, Taiwan 3 School of Resources and Environmental Engineering, Hefei University of Technology, Hefei 246011, China 4 Sustainable Environment Research Laboratories, National Cheng Kung University, Tainan 70101, Taiwan ABSTRACT In this study, the atmospheric PM2.5, increases/decreases of the PM2.5, the PM2.5/PM10 ratio, total PCDD/Fs-TEQ concentrations, PM2.5-bound total PCDD/Fs-TEQ content, and PCDD/F gas-particle partition in Taiwan were investigated for the period 2013 to 2017. In Taiwan, the annual average PM2.5 concentrations were found to be 28.9, 24.1, 21.4, 20.2, –3 and 19.9 µg m in 2013, 2014, 2015, 2016, and 2017, respectively, which indicated that the annual variations in PM2.5 levels were decreasing during the study period. The average increases (+)/decreases (–) of PM2.5 concentrations were –16.7%, –11.1%, –5.75%, and –1.73% from 2013 to 2014, from 2014 to 2015, from 2015 to 2016, and from 2016 to 2017, respectively. Based to the relationship between PM10 values and total PCDD/F concentrations obtained from previous studies, we estimated that in 2017, the annual average total PCDD/Fs-TEQ concentrations ranged between 0.0148 –3 –3 (Lienchiang County) and 0.0573 pg WHO2005-TEQ m (Keelung City), and averaged 0.0296 pg WHO2005-TEQ m , while –1 the PM2.5-bound total PCDD/Fs-TEQ content ranged from 0.302 (Kaohsiung City) to 0.911 ng WHO2005-TEQ g –1 (Keelung City), at an average of 0.572 ng WHO2005-TEQ g . -

Exploring Influence Range of Tainan City Using Electronic Toll Collection Big Data Chen Chou, Feng-Tyan Lin
Exploring Influence Range of Tainan City Using Electronic Toll Collection Big Data Chen Chou, Feng-Tyan Lin southernmost of Taiwan is possible, showing the present living Abstract—Big Data has been attracted a lot of attentions in many area can no longer achieve the need of spatial planning. fields for analyzing research issues based on a large number of This study substitutes “Living Area” with “Influence Range”, maternal data. Electronic Toll Collection (ETC) is one of Intelligent a certain distance changing through time period and trip Transportation System (ITS) applications in Taiwan, used to record objective. Tainan is a county in Taiwan; the study analyzes the starting point, end point, distance and travel time of vehicle on the national freeway. This study, taking advantage of ETC big data, interaction between Tainan and other counties by calculating combined with urban planning theory, attempts to explore various trip volume and visualizing through GIS. The finding not only phenomena of inter-city transportation activities. ETC, one of has a more precise outcome, but also could be applied to land government's open data, is numerous, complete and quick-update. One use arrangement. may recall that living area has been delimited with location, population, area and subjective consciousness. However, these factors cannot II. LITERATURE REVIEWS appropriately reflect what people’s movement path is in daily life. In this study, the concept of "Living Area" is replaced by "Influence A. Living Area Range" to show dynamic and variation with time and purposes of In 1995, Council for Economic Planning and Development, activities. This study uses data mining with Python and Excel, and visualizes the number of trips with GIS to explore influence range of Executive Yuan, Taiwan, proposed that the living area should Tainan city and the purpose of trips, and discuss living area delimited be defined as: The influence scope of socio-economic activities in current. -

9-Day Taiwan Exploration Taipei – Nantou – Chiayi – Tainan – Kaohsiung June 15-23, 2020
8-Day Taiwan Exploration Taipei – Nantou – Chiayi – Tainan – Kaohsiung ● Taipei 101 Tower, watch Taipei under your feet ● Various night markets will lead you to find the shopping area and the foodies ● Enjoy boat riding on Sun Moon Lake ● Visit the historic places in Tainan ● Visit the biggest Buddhist temple in Taiwan-Fogunshan Buddha Temple 9-Day Taiwan Exploration Taipei – Nantou – Chiayi – Tainan – Kaohsiung June 15-23, 2020 Taipei: It is the political, economic, cultural, industrial and commercial center of the island. Nantou: Located at the center of Taiwan Island. Nantou, the only inland county on the island is a land full of ASIA GETAWAY INC 7668 El Camino Real Ste 104-618, Carlsbad CA 92009 | Tel: (760) 635-1288 / (888) 288-1868 | Fax: (760) 635-1287 E-mail: [email protected] | www.asiagetaway.com | CST#2045443 ASIA GETAWAY INC 7668 El Camino Real Ste 104-618, Carlsbad CA 92009 | Tel: (760) 635-1288 / (888) 288-1868 | Fax: (760) 635-1287 E-mail: [email protected] | www.asiagetaway.com | CST#2045443 CHINESE IMMERSION TO TAIWAN 9 Day Taipei – Nantou – Chiayi – Tainan – Kaohsiung PROGRAM ITINERARY B – Breakfast, L – Lunch, D – Dinner DAY 1 – DEPART FROM LOS ANGELES (-) Depart from Los Angeles to Taipei. DAY 2 – ARR. TAIPEI (-) Arrive in Taipei, the capital of Taiwan. Meet your local representative and begin an orientation of Taiwan. • Chiang Kai-shek Memorial Hall is the most prominent historical landmark in Taiwan, it was erected in honor and memory of Generalissimo Chiang Kai-shek, the former President of the Republic of China. You may have an opportunity to watch the change of guards. -

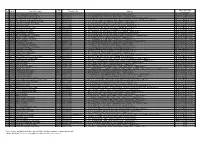
Directory of Head Office and Branches
Directory of Head Office and Branches 106 I. Domestic Business Units 120 Sec 1, Chongcing South Road, Jhongjheng District, Taipei City 10007, Taiwan (R.O.C.) P.O. Box 5 or 305 SWIFT: BKTWTWTP http://www.bot.com.tw TELEX 11201 TAIWANBK CODE OFFICE ADDRESS TELEPHONE FAX 0037 Department of 120 Sec 1, Chongcing South Road, Jhongjheng District, 02-23493399 02-23759708 Business ( I ) Taipei City 0059 Department of 120 Sec 1, Gueiyang Street, Jhongjheng District, 02-23615421 02-23751125 Public Treasury Taipei City 0071 Department of 49 Guancian Road, Jhongjheng District, Taipei City 02-23812949 02-23753800 Business ( II ) 0082 Department of 58 Sec 1, Chongcing South Road, Jhongjheng District, 02-23618030 02-23821846 Trusts Taipei City 0691 Offshore Banking 1F, 3 Baocing Road, Jhongjheng District, Taipei City 02-23493456 02-23894500 Branch 1850 Department of 4F, 120 Sec 1, Gueiyang Street, Jhongjheng District, 02-23494567 02-23893999 Electronic Banking Taipei City 1698 Department of 2F, 58 Sec 1, Chongcing South Road, Jhongjheng 02-23882188 02-23716159 Securities District, Taipei City 0093 Tainan Branch 155 Sec 1, Fucian Road, Central District, Tainan City 06-2160168 06-2160188 0107 Taichung Branch 140 Sec 1, Zihyou Road, West District, Taichung City 04-22224001 04-22224274 0118 Kaohsiung Branch 264 Jhongjheng 4th Road, Cianjin District, 07-2515131 07-2211257 Kaohsiung City 0129 Keelung Branch 16, YiYi Road, Jhongjheng District, Keelung City 02-24247113 02-24220436 0130 Chunghsin New 11 Guanghua Road, Jhongsing Village, Nantou City, 049-2332101 -

2018-IASP-In Research of Mental Health
In research of Mental Health advocacy and Preventing Suicide of the elderly in Taiwan Tai-Fen, Chen1、Yuchia, Chen2、Chenghsiung, Lee3、Chenyu, Ho4 POWERPOINT TEMPLATE, PLEASE TEXT YOUR TITLE HERE 1*. Assistant professor, Graduate Institute of Education, Tunghai University,Taiwan Email for correspondence: [email protected] 2. Associate Professor at National Tainan Junior College of Nursing 3. Honorary President of Taiwan LifeLine International 4. Research fellow and lecturer in Department of Social Work at Tung Hai University 01 Background 02 Motivation Purpose CONTENTS 03 04 Methodology 05 Result 06 Conclusion 01 Background This study was based on the Taiwan's elderly suicide situation that reasons were melancholy tends to be the most, followed by "emotional factors in family"(Taiwan Lifeline International,2015) While major depression is the main precipitant of suicide at all ages, social isolation is an important risk factor for suicide among the elderly. And older men, more so than older women, often become socially isolated (Brody,2007). How to health one’s mind and relationship will be so important for the suicidal ideation of elderly. 3 01 Background Taiwan LifeLine International Since the hotline service was introduced in Taiwan a half century ago, it has had a great many of contributions to the suicide prevention work of Taiwan. Currently, the hotline services which are familiarized by the public are “En-Sin Line”, which is entrusted to conduct by the government; and the “Lifeline”, which is set independently by private sectors. 4 02 Motivation Interested in the theory of Mental Health advocacy--- text The Wheel of Wellness Would like to know what relationship text This paper is going to research between on the wheel of wellness theoretical the development tendency of suicide prevention mode and actual status of implementation. -
No. Area Post Office Name Zip Code Telephone No. Address Same Day
Zip Same Day Flight No. Area Post Office Name Telephone No. Address Code Cutoff Time* 1 Tainan Chiayi Wunhua Rd. Post Office 60044 (05)2259-408(05)2227-881 No. 134, Wunhua Rd., East District, Chiayi 600-44, Taiwan (R.O.C.) Next-Day-Flight Service** 2 Tainan Chiayi Jhongshan Rd. Post Office 60041 (05)2785-145 No. 107, Jhongshan Rd., East District, Chiayi 600-41, Taiwan (R.O.C.) Next-Day-Flight Service** 3 Tainan Shueishang Nanjing Post Office 60859 (05)2682-035 No. 1, Sanjhen Rd., Sanjhen Village, Shueishang, Chiayi County 608-59, Taiwan (R.O.C.) Next-Day-Flight Service** 4 Tainan Shueishang Jhongjhuang Post Office 60857 (05)2890-344 No. 61-61, Jhongjhuang, Jhongjhuang Village, Shueishang, Chiayi County 608-57, Taiwan (R.O.C.) Next-Day-Flight Service** 5 Tainan Chiayi Railway Station Front Post Office 60042 (05)2242-021 No. 647, Jhongjheng Rd., West District, Chiayi 600-42, Taiwan (R.O.C.) Next-Day-Flight Service** 6 Tainan Chiayi Mincyuan Rd. Post Office 60044 (05)2273-547 No. 467, Mincyuan Rd., West District, Chiayi 600-44, Taiwan (R.O.C.) Next-Day-Flight Service** 7 Tainan Taibao Post Office 61250 (05)3711-040 No. 439-2, Houtan Village, Taibao, Chiayi County 612-50, Taiwan (R.O.C.) Next-Day-Flight Service** 8 Tainan Chiayi Jhongsiao Post Office 60044 (05)2783-079 No. 2(08)1, Mincyuan Rd., East District, Chiayi 600-44, Taiwan (R.O.C.) Next-Day-Flight Service** 9 Tainan Chiayi Beishe Post Office 60092 (05)2320-200 No. 245, Beising St., West District, Chiayi 600-92, Taiwan (R.O.C.) Next-Day-Flight Service** 10 Tainan Shueishang Post Office 60848 (05)2682-140 No. -

Wang Shao- Gang Wang Shao- Gang (Born 1985, Taiwan) Graduated from the Graduate Institute of New Media Art in Taipei National University of the Arts
Wang Shao- Gang Wang Shao- Gang (born 1985, Taiwan) graduated from the Graduate Institute of New Media Art in Taipei National University of the Arts. Wang specializes in exploring the interrelations between the self and the external through video installation. Constantly experimenting with the possibilities of video art, he is committed to restructuring film, video, documentary and other forms of image creation, diminishing the scope of boundaries in order to probe the state of reality and construct various images of the world. Wang is currently in an ongoing attempt to research the humanistic culture and history of the locality through his creative practice. He is fascinated by his random encounters with people and the fragmented events that occur throughout space and time yet eternally in the process of facing oblivion. For him, the objects and places seen in the immediate reality are not simply as they appear, but exist before us through unseen processes; therefore, he raises many doubts to the reality that we live in and pieces together imaginary subjects and fictional perspectives in his works to liberate the obvious appearances of reality. Recent exhibitions include: "The Moment that Comes is about to Go- 6 Visions about Time" (Digital Art Center, Taipei, 2017), "Chiayi City International Art Documentary Film Festival-Enjoy Art Of All"(Chiayi Municipal Museum, Chiayi, 2017), "Taiwan Biennial -The possibility of an island" (Taipei Fine Arts Museum, Taipei, 2016), "Kaohsiung Awards"(Kaohsiung Museum of Fine Arts, Kaohsiung, 2016), "Taipei Arts Award" (Taipei Fine Arts Museum, Taipei, 2015), and "Sanchin- Wang Shao- Gang solo exhibition" (Open Contemporary Art Center, Taipei, 2015). -

Anolis Sagrei Duméril &
WWW.IRCF.ORG/REPTILESANDAMPHIBIANSJOURNALTABLE OF CONTENTS IRCF REPTILES & AMPHIBIANS IRCF REPTILES • VOL15, &NO AMPHIBIANS 4 • DEC 2008 189 • 23(1):62–67 • APR 2016 IRCF REPTILES & AMPHIBIANS CONSERVATION AND NATURAL HISTORY TABLE OF CONTENTS INTRODUCED SPECIES FEATURE ARTICLES . Chasing Bullsnakes (Pituophis catenifer sayi) in Wisconsin: The KnownOn the Road to Understanding Distribution the Ecology and Conservation of the Midwest’sof Giantan Serpent ......................Invasive Joshua M. Kapfer 190Lizard, . The Shared History of Treeboas (Corallus grenadensis) and Humans on Grenada: A Hypothetical Excursion ............................................................................................................................Robert W. Henderson 198 theRESEARCH Brown ARTICLES Anole (Anolis sagrei Duméril & . The Texas Horned Lizard in Central and Western Texas ....................... Emily Henry, Jason Brewer, Krista Mougey, and Gad Perry 204 . The Knight AnoleBibron, (Anolis equestris) in Florida 1837), in Taiwan .............................................Brian J. Camposano, Kenneth L. Krysko, Kevin M. Enge, Ellen M. Donlan, and Michael Granatosky 212 1 2 3 3 4 5 1 Gerrut NorvalCONSERVATION, Guo-Quan Wang ALERT, Jean-Jay Mao , Li-Xhan Liu , Meng-Hsien Chuang , Yi-Ju Yang , Kerry Slater , and Leslie R. Brown1 . World’s Mammals in Crisis ............................................................................................................................................................. 220 . More1Applied Than BehaviouralMammals -

Lessons Learnt from Taiwan's High Speed Rail
Proceedings of the Eastern Asia Society for Transportation Studies, Vol.8, 2011 Lessons Learnt from Taiwan’s High Speed Rail Cheng-Min FENG Professor Institute of Traffic and Transportation National Chiao Tung University 4F, 118, Sec. 1, Chung Hsiao W. Rd., Taipei 10012, Taiwan, ROC Fax: +886-2-2349-4965 E-mail: [email protected] Abstract: Taiwan takes BOT approach to build and operate its high speed rail. Several issues such as the enact of new law vs. the modification of old law, tri-party agreement vs. two-party agreement, partner or regulator, refinance vs. take-over, new town vs. old town, expropriation or zonal expropriation, and plan vs. development, occurred during the planning, construction, contracting and operation periods. Taiwan learns its lessons from the process and its outcomes, which could help others to prevent the issues or adapt their plans. Key Words: high speed rail, BOT, issues, lessons 1. INTRODUCTION There is an increasing need to build new transportation infrastructure to meet the intercity travel needs in western Taiwan. However, at the same time, there is a decreasing amount of government funds available to finance the infrastructure, and a decreasing tolerance among taxpayers or transportation user to increase taxes or user fees. One alternative solution is to build high speed rail (HSR) in Taiwan with the participation of private sector. In the planning and design stage, the most of arguments lie in the location of station, the acquisition of land, station area’s plan and design, and who will construct and operate the HSR, which were all determined by the government. -
A Report on Male Anolis Sagrei Saurophagy in Chiayi County, Taiwan
A report on male Anolis sagrei saurophagy in Chiayi County, Taiwan GERRUT NORVAL ' Applied Behavioural Ecology and Ecosystem Research Unit, Department of Nature Conservation, UNISA, Private Bag X6, Florida, 1710, Republic of South Africa. ABSTRACT — Five hundred and two Brown anoles (A nails sagrei) were collected for stomach content analysis from an area surrounding a plant nursery (23°25'51"N, 120°28'30"E) in Santzepu, Sheishan District, Chiayi County, as part of an ongoing study on this invasive species in Taiwan. The stomachs of five A. sagrei males contained vertebrate prey, which were isolated for identification to establish a basis upon which future studies can be based. These prey were identified as three hatchlings of A. sagrei, a Henzidactyhts fienatus hatchling, and a skink hatchling — most likely that of Spheitomolphus indicus. The results of this study seems to indicate that male A. sagrei saurophagy is more likely in cleared open habitats, with no ground cover, than in habitats with ground covering. s a whole, lizards exhbit a wide range of these lizards were usually only extended to the variation in what they eat; some have a class or order levels, it was decided to isolate all ..catholic diet, while others are specialists that prey the vertebrate prey from the other prey items for a only on specific types of prey (Mattison, 1997). more in-depth examination to establish a basis Only a few lizard species, such as Lialis burtonis upon which future studies on predation on (Pygopodidae), specialize in preying on other vertebrates by this species in Taiwan can be based.