Treatment of Refractory Generalized Status Epilepticus with Continuous Infusion of Midazolam
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Midazolam Injection, USP
Midazolam Injection, USP 2 mg per 2 mL | NDC 70860-600-02 50 mg per 10 mL | NDC 70860-601-10 ATHENEX AccuraSEETM PACKAGING AND LABELING BIG, BOLD AND BRIGHT — TO HELP YOU SEE IT, SAY IT AND PICK IT RIGHT DIFFERENTIATION IN EVERY LABEL, DESIGNED TO HELP REDUCE MEDICATION ERRORS PLEASE SEE FULL PRESCRIBING INFORMATION, INCLUDING BOXED WARNING, FOR MIDAZOLAM INJECTION, USP, ENCLOSED. THE NEXT GENERATION OF PHARMACY INNOVATION To order, call 1-855-273-0154 or visit www.Athenexpharma.com Midazolam Injection, USP 2 5 mg NDC 70860-600-02 0 NDC 70860-601-10 2 mg per 2 mL mg 50 mg per 10 mL DESCRIPTION Glass Vial DESCRIPTION Glass Vial CONCENTRATION 1 mg per mL CONCENTRATION 5 mg per mL CLOSURE 13 mm CLOSURE 20 mm UNIT OF SALE 25 vials UNIT OF SALE 10 vials BAR CODED Yes BAR CODED Yes STORAGE Room Temp. STORAGE Room Temp. • AP RATED • PRESERVATIVE-FREE • AP RATED • NOT MADE WITH NATURAL RUBBER LATEX • NOT MADE WITH NATURAL RUBBER LATEX CHOOSE AccuraSEETM FOR YOUR PHARMACY Our proprietary, differentiated and highly-visible label designs can assist pharmacists in accurate medication selection. With a unique label design for every Athenex product, we’re offering your pharmacy added AccuraSEE. The idea is simple: “So what you see is exactly what you get.” Athenex, AccuraSEE and all label designs are copyright of Athenex. ©2020 Athenex. 000527 To order, call 1-855-273-0154 or visit www.Athenexpharma.com • Midazolam hydrochloride mufti-dose vial, is not intended for intrathecal or epidural • Anesthetic and sedation drugs are a necessary part of the care of children needing Midazolam Injection, USP administration, and is contraindicated for use in premature infants, because the formulation surgery, other procedures, or tests that cannot be delayed, and no specific medications INDICATIONS AND USAGE contains benzyl alcohol as a preservative. -

The Use of Barbital Compounds in Producing Analgesia and Amnesia in Labor
University of Nebraska Medical Center DigitalCommons@UNMC MD Theses Special Collections 5-1-1939 The Use of barbital compounds in producing analgesia and amnesia in labor Stuart K. Bush University of Nebraska Medical Center This manuscript is historical in nature and may not reflect current medical research and practice. Search PubMed for current research. Follow this and additional works at: https://digitalcommons.unmc.edu/mdtheses Part of the Medical Education Commons Recommended Citation Bush, Stuart K., "The Use of barbital compounds in producing analgesia and amnesia in labor" (1939). MD Theses. 730. https://digitalcommons.unmc.edu/mdtheses/730 This Thesis is brought to you for free and open access by the Special Collections at DigitalCommons@UNMC. It has been accepted for inclusion in MD Theses by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. THE USE OF THE BARBITAL COMPOUl~DS IN PRODUCING ANALGESIA AND .AMNESIA.IN LABOR Stuart K. Bush Senior Thesis Presented to the College of Medicine, University of Nebraska, Omaha, 1939 481021 THE USE OF THE BARBITAL COMPOUNDS IN PROLUCING ANALGESIA AND AMNESIA IN LABOR The Lord God said unto Eve, "I will greatly mul tiply thy sorrow and thJ conception; in sorrow thou shalt bring forth children." Genesis 3:lti Many a God-fearing man has held this to mean that any attempt to ease the suffering of the child bearing mother would be a direct violation of the Lord's decree. Even though the interpretation of this phrase has formed a great barrier to the advance ment of the practice of relieving labor pains, attempts to achieve this beneficent goal have been made at va rious times throughout the ages. -

The Emergence of New Psychoactive Substance (NPS) Benzodiazepines
Issue: Ir Med J; Vol 112; No. 7; P970 The Emergence of New Psychoactive Substance (NPS) Benzodiazepines. A Survey of their Prevalence in Opioid Substitution Patients using LC-MS S. Mc Namara, S. Stokes, J. Nolan HSE National Drug Treatment Centre Abstract Benzodiazepines have a wide range of clinical uses being among the most commonly prescribed medicines globally. The EU Early Warning System on new psychoactive substances (NPS) has over recent years detected new illicit benzodiazepines in Europe’s drug market1. Additional reference standards were obtained and a multi-residue LC- MS method was developed to test for 31 benzodiazepines or metabolites in urine including some new benzodiazepines which have been classified as New Psychoactive Substances (NPS) which comprise a range of substances, including synthetic cannabinoids, opioids, cathinones and benzodiazepines not covered by international drug controls. 200 urine samples from patients attending the HSE National Drug Treatment Centre (NDTC) who are monitored on a regular basis for drug and alcohol use and which tested positive for benzodiazepine class drugs by immunoassay screening were subjected to confirmatory analysis to determine what Benzodiazepine drugs were present and to see if etizolam or other new benzodiazepines are being used in the addiction population currently. Benzodiazepine prescription and use is common in the addiction population. Of significance we found evidence of consumption of an illicit new psychoactive benzodiazepine, Etizolam. Introduction Benzodiazepines are useful in the short-term treatment of anxiety and insomnia, and in managing alcohol withdrawal. 1 According to the EMCDDA report on the misuse of benzodiazepines among high-risk opioid users in Europe1, benzodiazepines, especially when injected, can prolong the intensity and duration of opioid effects. -

Comparative Enhancing Effects of Phenobarbital, Amobarbital
[CANCER RESEARCH 35,2884 2890, October 1975] Comparative Enhancing Effects of Phenobarbital, Amobarbital, Diphenylhydantoin, and Dichlorodiphenyltrichloroethane on 2-Acetylaminofluorene-induced Hepatic Tumorigenesis in the Rat Carl Peraino, R. J. Michael Fry, Everett Staffeldt, and John P. Christopher 2 Division of Biological and Medical Research, Argonne National Laboratory, Argonne, Illinois 60439 SUMMARY INTRODUCTION Earlier studies showed that phenobarbital feeding en- In earlier studies (27, 29), the prolonged feeding of hanced hepatic tumorigenesis in rats previously fed 2- phenobarbital to rats that had previously been fed AAF 3 for acetylaminofluorene for a brief period. As part of an a brief period markedly increased the subsequent incidence investigation of the mechanism of this enhancement, the of liver tumors. Using this sequential feeding regime, the present study evaluated the relative enhancing abilities of present study evaluated the relative tumorigenic enhancing amobarbital, diphenylhydantoin, and dichlorodiphenyltri- abilities of other compounds that, to varying degrees, chloroethane (DDT), agents that resemble phenobarbital to resemble phenobarbital in their effects on liver structure and varying degrees in their effects on liver structure and metabolism. The substances examined were amobarbital, metabolism. A comparison of hepatic tumor yields in rats diphenylhydantoin, and DDT. Table 1 compares relevant fed 2-acetylaminofluorene, followed by the test substance characteristics of these agents with those of phenobarbital, (sequential treatment), showed that amobarbital and di- reviewed previously (27, 29). Amobarbital is closest to phenylhydantoin had no enhancing activity, whereas the phenobarbital in structure and, like phenobarbital, alters enhancing effect of DDT was similar to that of phenobarbi- the metabolism of other drugs by the liver. Diphenylhydan- tal. -

The Waterloo Wellington Palliative Sedation Protocol
The Waterloo Wellington Palliative Sedation Protocol Waterloo Wellington Interdisciplinary HPC Education Committee; PST Task Force Chair: Dr. Deborah Robinson MD CCFP(F), Focused practice in Oncology and Palliative Care Co-chairs: Cathy Joy, Palliative Care Consultant, Waterloo Region Chris Bigelow, Palliative Care Consultant, Wellington County Revision due: November 2016 Last revised and activated: November 13, 2013 Committee responsible for revisions: WW Interdisciplinary HPC Education Committee Table of Contents Purpose and Definitions .................................................................................................................... 2 Indications for the use of PST .............................................................................................................. 3 Criteria for Initiation of PST ............................................................................................................... 4 Process ............................................................................................................................................. 4 Documentation for Initiation of PST .................................................................................................. 5 Medications ......................................................................................................................................... 6 1st Line (Initiating PST) ...................................................................................................................... 6 2nd Line (When 1st -

Midazolam Injection, USP
Midazolam Injection, USP Rx only PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION WARNING ADULTS AND PEDIATRICS: Intravenous midazolam has been associated with respiratory depression and respiratory arrest, especially when used for sedation in noncritical care settings. In some cases, where this was not recognized promptly and treated effectively, death or hypoxic encephalopathy has resulted. Intravenous midazolam should be used only in hospital or ambulatory care settings, including physicians’ and dental offices, that provide for continuous monitoring of respiratory and cardiac function, i.e., pulse oximetry. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation, and personnel trained in their use and skilled in airway management should be assured (see WARNINGS). For deeply sedated pediatric patients, a dedicated individual, other than the practitioner performing the procedure, should monitor the patient throughout the procedures. The initial intravenous dose for sedation in adult patients may be as little as 1 mg, but should not exceed 2.5 mg in a normal healthy adult. Lower doses are necessary for older (over 60 years) or debilitated patients and in patients receiving concomitant narcotics or other central nervous system (CNS) depressants. The initial dose and all subsequent doses should always be titrated slowly; administer over at least 2 minutes and 1 allow an additional 2 or more minutes to fully evaluate the sedative effect. The dilution of the 5 mg/mL formulation is recommended to facilitate slower injection. Doses of sedative medications in pediatric patients must be calculated on a mg/kg basis, and initial doses and all subsequent doses should always be titrated slowly. -
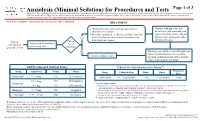
Anxiolysis (Minimal Sedation) for Procedures and Tests
Anxiolysis (Minimal Sedation) for Procedures and Tests Page 1 of 3 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. Note: Refer to UTMDACC Institutional Policy #CLN0502 for complete information. TREATMENT ● Document mental status and vital signs prior to Continue with procedure and administering sedation document mental status and vital ● Determine appropriate medication and dose based on signs after administering sedation onset of action (see chart below) of anxiolytic for and prior to beginning procedure Yes 1 desired patient response and post-procedure Patient Patient Assess need for anxiolysis scheduled for needs prior to procedure procedure or test anxiolysis? No Discharge patient when clinically stable and follow institutional processes regarding Continue with procedure discharge instructions and criteria for both inpatient and outpatient settings 2,3 Adult Recommended Anxiolysis Dosing Pediatric Recommended Anxiolysis Dosing3,5,6 Maximum Drug Adult Dose Route Onset Drug Pediatric Dose Route Onset Dose 4 Midazolam 5 – 10 mg PO 10-30 minutes Midazolam 0.5 – 1 mg/kg/dose PO 10-20 minutes 5 mg 0.5 – 2 mg PO 30-60 minutes Lorazepam 5 Pediatric considerations: 1 – 4 mg IM 20-30 minutes ● Consider lower dosing strategies for patients with cardiac or respiratory compromise, and those who received concomitant opiates, benzodiazepines or similar synergistic sedative medications. -

Barbiturates for the Treatment of Alcohol Withdrawal Syndrome: ☆ a Systematic Review of Clinical Trials
Journal of Critical Care 32 (2016) 101–107 Contents lists available at ScienceDirect Journal of Critical Care journal homepage: www.jccjournal.org Barbiturates for the treatment of alcohol withdrawal syndrome: ☆ A systematic review of clinical trials Yoonsun Mo, MS, Pharm.D., BCPS, BCCCP a,b,⁎, Michael C. Thomas, Pharm.D., BCPS, FCCP a,1, George E. Karras Jr., MD, FCCM b,2 a Department of Pharmacy Practice, Western New England University College of Pharmacy, 1215 Wilbraham Road, Springfield, MA 01119 b Mercy Medical Center, 271 Carew Street, Springfield, MA 01104 article info abstract Keywords: Purpose: To perform a systematic review of the clinical trials concerning the use of barbiturates for the treatment Barbiturates of acute alcohol withdrawal syndrome (AWS). Phenobarbital Materials and Methods: A literature search of MEDLINE, EMBASE, and the Cochrane Library, together with a man- Benzodiazepines ual citation review was conducted. We selected English-language clinical trials (controlled and observational Alcohol withdrawal syndrome studies) evaluating the efficacy and safety of barbiturates compared with benzodiazepine (BZD) therapy for Delirium tremens Systematic review the treatment of AWS in the acute care setting. Data extracted from the included trials were duration of delirium, number of seizures, length of intensive care unit and hospital stay, cumulated doses of barbiturates and BZDs, and respiratory or cardiac complications. Results: Seven studies consisting of 4 prospective controlled and 3 retrospective trials were identified. Results from all the included studies suggest that barbiturates alone or in combination with BZDs are at least as effective as BZDs in the treatment of AWS. Furthermore, barbiturates appear to have acceptable tolerability and safety pro- files, which were similar to those of BZDs in patients with AWS. -
Forensic Toxicology Scope of Testing and Detection Limits
J. RYAN MCMAHON II County Executive INDU GUPTA, MD, MPH MEDICAL EXAMINER’S OFFICE Commissioner of Health FORENSIC TOXICOLOGY LABORATORY CAROLYN H. REVERCOMB, MD, DABP ONONDAGA COUNTY HEALTH DEPARTMENT Chief Medical Examiner KRISTIE BARBA, MS, D-ABFT-FT CENTER FOR FORENSIC SCIENCES Toxicologist Forensic Toxicology Scope of Testing and Detection Limits Table of Contents QUALITATIVE ANALYSES.........................................................................................................2 Volatile Screen by GC/FID .............................................................................................................2 Carbon Monoxide by Microdiffusion..............................................................................................2 Carbon Monoxide by CO-Oximeter ................................................................................................2 Ethylene Glycol by GC/MS.............................................................................................................2 ELISA Buprenorphine by IA for Blood/Urine ................................................................................2 ELISA by IA for Blood ...................................................................................................................3 ELISA by IA for Urine....................................................................................................................4 Gamma Hydroxybutyrate (GHB) by GC/MS..................................................................................5 Gabapentin, -

Original Article Effects of Repeated High Dosage of Chloral Hydrate and Pentobarbital Sodium Anesthesia on Hepatocellular System in Rats
Int J Clin Exp Med 2015;8(7):10568-10576 www.ijcem.com /ISSN:1940-5901/IJCEM0008402 Original Article Effects of repeated high dosage of chloral hydrate and pentobarbital sodium anesthesia on hepatocellular system in rats Jianhong Yu1*, Xuehui Sun2*, Guifeng Sang3 1Department of Anesthesiology, Yuhuangding Hospital, Yantai 264000, China; 2Department of Rheumatology, Yuhuangding Hospital, Yantai 264000, China; 3Operating Room, Yuhuangding Hospital, Yantai 264000, China. *Equal contributors. Received March 24, 2015; Accepted July 2, 2015; Epub July 15, 2015; Published July 30, 2015 Abstract: This study aims to investigate the possible effects of repeated high dosage of chloral hydrate and pen- tobarbital sodium anesthesia on hepatocellular system in rats. Thirty Sprague Dawley rats were randomly divided into 3 groups: control group (group A), chloral hydrate group (group B) and pentobarbital sodium group (group C). Antioxidant enzymes superoxide dismutase (SOD), glutathione peroxidase (GSH-Px), glutathione s transferase (GST) and catalase (CAT) activities and thiobarbituric acid-reactive substances (TBARS) level as well as serum biochemi- cal parameters alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP) and total bilirubin (T-BIL) were determined. Liver histopathological examinations were performed at termination. Furthermore, Bax and Bcl-2 expression, and caspase-3 activity were also evaluated. The SOD, GSH-Px, GST and CAT activities significantly decreased but TBARS levels increased in group B and C compared with group A. Hepatic injury was evidenced by a significant increase in serum ALT, AST and ALP activities in group B and C, which also con- firmed by the histopathological alterations. Moreover, administration of chloral hydrate and pentobarbital sodium could induce certain hepatic apoptosis accompanied by the upregulated Bax expression, the downregulated Bcl-2 expression and Bcl-2/Bax ratio, and the increase of caspase-3 activity. -

Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: an American Academy of Sleep Medicine Clinical Practice Guideline Michael J
pii: jc-00382-16 http://dx.doi.org/10.5664/jcsm.6470 SPECIAL ARTICLES Clinical Practice Guideline for the Pharmacologic Treatment of Chronic Insomnia in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline Michael J. Sateia, MD1; Daniel J. Buysse, MD2; Andrew D. Krystal, MD, MS3; David N. Neubauer, MD4; Jonathan L. Heald, MA5 1Geisel School of Medicine at Dartmouth, Hanover, NH; 2University of Pittsburgh School of Medicine, Pittsburgh, PA; 3University of California, San Francisco, San Francisco, CA; 4Johns Hopkins University School of Medicine, Baltimore, MD; 5American Academy of Sleep Medicine, Darien, IL Introduction: The purpose of this guideline is to establish clinical practice recommendations for the pharmacologic treatment of chronic insomnia in adults, when such treatment is clinically indicated. Unlike previous meta-analyses, which focused on broad classes of drugs, this guideline focuses on individual drugs commonly used to treat insomnia. It includes drugs that are FDA-approved for the treatment of insomnia, as well as several drugs commonly used to treat insomnia without an FDA indication for this condition. This guideline should be used in conjunction with other AASM guidelines on the evaluation and treatment of chronic insomnia in adults. Methods: The American Academy of Sleep Medicine commissioned a task force of four experts in sleep medicine. A systematic review was conducted to identify randomized controlled trials, and the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) process was used to assess the evidence. The task force developed recommendations and assigned strengths based on the quality of evidence, the balance of benefits and harms, and patient values and preferences. -

Article on Relative Abuse Liability of Triazolam
Neuroscience & giobehaviora[Reviews. Vol. 9, pp. 133-151. 19_5. e Ankho International Inc. Printed in the U.S.A 0149-7634/85 5300 ÷ 00 Relative Abuse Liability of Triazolam: Experimental Assessment in Animals and Humans ROLAND R. GRIFFITHS,** RICHARD J. LAMB,* NANCY A. ATOR,* JOHN D. ROACHE* AND JOSEPH V. BRADY** Departments of *Psychiatry and tNeuroscience. The Johns Hopkins University School of Medicine 720 Rutland Avenue, Baltimore, MD 21205 GRIFFITHS, R. R., R. J. LAMB, N. A. ATOR, J. D. ROACHE AND J. V. BRADY. Relative abuse liability oftriazolam: Experimental assessment in animals and humans. NEUROSCI BIOBEHAV REV 9(1) 133--151. 1985.--The abuse liability of a drug is a positive, interactive function of the reinforcing and adverse effects of the drug. The relative abuse liability of the hypnotic henzodiazepine, triazoiam, has been controversial. This paper reviews animal and human studies beating on its relative abuse liability, including data on pharmacological profile, reinforcing effects, liking, speed of onset, discrimina- tive stimulus effects, subjective effects, physiological dependence, rebound and early morning insomnia, drug produced anxiety, lethality in overdose, psychomotor impairment, interactions with ethanol anterogr_e amnesia, impaired aware- ness of drug effect, and other psychiatric and behavioral disturbances. It is concluded that the abuse liability of triazolam is less than that of the intermediate duration barbiturates such as pentobarbital. Although there are considerable data indicating similarities of triazolam to other benzodiazepines, there is also substantial speculation among clinical inves- til_tors and some limited data suggesting that the abuse liability of triazolam is greater than that of a variety of other benzodiazepines, and virtually no credible data or speculation that it is less.