Eating Behaviours and Attitudes in Narcolepsy and Their Association with Sleepiness and Mood
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Revival of Active Behavioural Devices for Measuring Sleep Latency
SMGr up Review Article SM Journal of The Revival of Active Behavioural Sleep Disorders Devices for Measuring Sleep Latency Hannah Scott1* and Leon Lack1,2 1Department of Psychology, Flinders University, Australia 2Department of Medicine, Flinders University, Australia Article Information Abstract Received date: Sep 26, 2017 The current gold standard for objectively measuring sleep latency, polysomnography (PSG), requires Accepted date: Oct 31, 2017 specialised equipment and trained individuals to administer. As such, PSG is an expensive and cumbersome procedure, particularly for use in the home environment. Actigraphy devices are a common practical alternative Published date: Nov 06, 2017 that can be used in the home environment, but they often underestimate sleep latency. For these reasons, it is difficult to accurately measure sleep latency outside of the sleep laboratory setting. *Corresponding author This problem has led to the revival of active behavioural devices for measuring sleep latency. Thim is a Hannah Scott, School of Psychology, small active behavioural device that uses behavioural responses to stimuli to measure the onset of sleep. The Flinders University, GPO Box 2100, design of Thim is based on previous research with similar devices, which were found to accurately measure sleep latency. If found to accurately measure sleep onset, Thim could be used for many potential applications, Adelaide, Australia, 5001, including facilitating 10-minute power naps and administering a novel, effective treatment for insomnia called Tel: 61 08 8201 2767; Intensive Sleep Retraining (ISR) in the home environment. This review will highlight current methods for Email: [email protected] objectively measuring sleep latency, the limits of commonly-used devices and how active behavioural devices such as Thim could allow for the accurate measurement of sleep latency in the home environment. -

The Science of Sleep
In order to have efficient and normal functioning of all systems in the body adequate and restorative sleep must be obtained. Mental and physical health is directly affected by an individual’s sleep patterns with poor sleep resulting in a reduced ability to ward off and cope with sickness, a reduced capacity for cellular healing, repair and replacement. This can directly result in altered body system functions and processes that can adversely affect overall wellbeing, particularly in those with autoimmune and other inflammatory conditions. Lack of sleep can also lead to changes in; moods, anxiety, irritability, cognitive function and concentration. Loss of adequate and restorative sleep has also been associated with reduced balance and hand eye co-ordination with the potential for increased injury and decreased capacity to complete work tasks. Sleep is considered to be a dynamic process which involves continuing brain activity which acts to produce and release hormones and proteins essential for organ system regulation as well as growth and tissue repair. The attainment of adequate sleep encourages the maintenance of emotional and social functioning while awake by giving a rest during sleep to the parts of the brain that control emotions and social interactions. Brain chemicals and hormones such as serotonin, adrenaline, melatonin and cortisol are directly involved with many signalling pathways and organ functioning in the human body. These chemicals are involved in nerve signalling processes and play an important part in controlling the sleep and wakening processes by stimulating different parts of the brain and inhibiting other parts of the brain to either promote sleep or keep a person awake. -

Fatigue and Sleep Management
EUROCONTROL EUROCONTROL Fatigue and Sleep Management Personal strategies for decreasing the effects of fatigue in Air Traffic Control 1 Fatigue and Sleep Management 2 For shift workers, fatigue and sleep debt can become a challenge and difficult to cope with. We have designed this booklet to give you knowledge and strategies that you can apply in your daily lives in order to help you better manage your sleep. When reading this booklet , bear in mind that whilst some of the ideas/suggestions may seem a little eccentric, people are different, and something that may work for one person may not work for another. Find what works for you, then you will be one step closer to getting a good night’s sleep and feeling less tired. Sweet dreams! 3 4 CONTENTS General Introduction to Fatigue, Sleep and Shift work.............................................................................................. 6 Circadian Rhythms and Sleep Patterns ........................................................................................................................................ 9 Shift work – A Better Understanding .........................................................................................................................................27 Tips and Tools for Fatigue and Sleep Management .....................................................................................................37 Bedtime Rituals ...................................................................................................................................................................................................37 -

Kicking the Bear out of the Bedroom Snoring & Sleep Apnea
Kicking the Bear Out of the Bedroom Snoring & Sleep Apnea, the Not-So-Silent Killers Steve Wick Foreword by Dr Poul Kirketerp, DDS Copyright 2016, Steven Wick All rights reserved. No part of this publication may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the publisher, except in the case of brief quotations embodied in reviews and certain other noncommercial uses permitted by copyright law. ISBN-13: 978-1539751885 ISBN-10: 1539751880 $12.99 USA / $14.99 CANADA 2 | P a g e To my wife and daughter, who each in their own way, propelled me on my journey. 3 | P a g e Forord på dansk af Tandlæge Poul Kirketerp Kære Læser, Tillykke med at du har taget en skridt i den rigtige retning til at forstå din snorken og eventuelle søvnapnø. Du er på vej til at forstå, hvor potentielt farlig disse tilstande kan være for dig. Mange studier over hele verden viser dette. Et nyligt studie i the International ”Sleep Health” Journal lavet af the Australian Sleep Health Foundation1) viste at 45% af alle voksne i Australien har søvnproblemer, som kan være medvirkende til at forringe deres generelle helbred og evnen til at fungere i en normal hverdag. Flere alvorlige medicinske sygdomme er forbundet med søvnapnø og dårlig søvn. Er du diagnosticeret med Obstruktiv Søvnapnø, er CPAP i Danmark og andre steder oftest førstevalget for behandling af sygdommen. Dette er på trods af, at rigtig mange der har fået udleveret CPAP, har store problemer med at bruge apparatet, mens en stor del af patienterne slet ikke bruger det. -

Take a Break: Increased Productivity Thanks to Axbo Power Napping
Take a break: increased productivity thanks to aXbo power napping Our society demands that we produce top performance and results quickly and consistently – all throughout the day. But if we were to listen to our natural biorhythms, this would be an impossible feat. As of November 1st, the aXbo sleep phase alarm clock is equipped with a new function, "PowerNap," for brief midday naps. Power naps have a rejuvenating effect. We spoke with Dr. Georg Dorffner, university professor and managing director of the Siesta Group Schlafanalyse, about power napping, the effects of power napping and the studies carried out on the topic. Vienna, 31 October 2007 – The lights are dimmed, telephone calls are re-routed, and no meetings are scheduled: imagine reclining in your chair and taking a short relaxing break – right in the middle of the working day, and without a guilty conscience. This is the dream of many a hard worker, yet our achievement-oriented society demands from us that we work twelve hours a day or more, every day, and remain highly concentrated and in best form all day long. However, sleep research findings show that we experience a decrease in performance levels around noon. Sleep researcher Dr. Jürgen Zulley actually discovered this phenomenon over 20 years ago when he arranged for 450 volunteers to spend 4 weeks in a subterranean bunker. Without daylight or clocks, the test candidates soon lost all feeling for the time of day. "The test persons usually took a nap of around half an hour around noon under the assumption that it was already evening. -

Drowsy Driving Behind the Wheel of the School
Drowsy Driving Awareness and Prevention 2 OUR THANKS! “This educational program was funded by the National Highway Traffic Safety Administration with a grant from the New York Governor's Traffic Safety Committee" 3 N.Y.A.P.T. The New York Association for Pupil Transportation has produced this educational program as part of a Highway Safety Grant provided through the Governor’s Traffic Safety Committee with NHTSA funding. (2017) NYAPT wishes to thank the Pupil Transportation Safety Institute (PTSI) for its collaboration in the design and development of this educational offering. 4 Today’s Training Will Address… Scope of the problem - data Risk factors of drowsy driving Warning Signs Causes of fatigue What Doesn’t work to prevent drowsiness Sleep Disorders Drowsy Driving Legislation 5 Scope of the Problem 6% of all crashes and 21% of all fatal crashes involved a fatigued driver 6,000 lives lost annually 30% of all drivers in the US have dozed off behind the wheel * 2014 National Safety Council and AAA statistics 6 Effect on Driving Fatigue = Reduced Safety Performance Driving after only 4-5 hours of sleep = similar crash risk as driving legally drunk at .08 BAC Drowsy driving is similar to drunk driving Driving after sleeping only 5-6 hours a night nearly doubles your risk of having a crash AAA Foundation 2016 statistics A Micro-sleep Can Kill You In Seconds… 7 In a 3 second micro-sleep, traveling 45 mph, your vehicle travels198 feet – 65 yards 4 average school bus lengths More than half a football field 8 9 Risk Factors -

The Effect of Power Napping on Performance
Utrecht University Applied Cognitive Psychology Master thesis The effect of power napping on performance Name: Luke Crooymans Student number: 0494992 Date: 15-08-2011 Philips Research High Tech Campus, 5656 AE, Eindhoven, the Netherlands Utrecht University: Stella Donker & Maarten van der Smagt Philips Research: Roy Raymann & Els Møst 1 Contents: Page: Abstract: 3 Introduction 4 Methods 8 Participants 8 Design & Procedure 8 Materials 10 Statistical procedure 13 Results 16 Sleep data 16 Subjective measures 19 Performance measures 21 Discussion 26 Acknowledgements 29 References 30 Appendix 33 2 Abstract Introduction Daytime (power) napping has been demonstrated to counteract feelings of fatigue and decreases in cognitive performance during the day. However, the duration and the composition of daytime naps are decisive for their restorative power. Short naps may be too brief to relieve sleep pressure, boost alertness and cognitive performance. Longer naps have an increased risk of waking up from deep sleep. As such, exaggerated feelings of fatigue can negatively impact alertness and cognitive performance, due to sleep inertia. Study objective Investigating the effect of different durations and composition (in terms of sleep stages) of daytime napping on subjective wellbeing, performance and alertness. Design 24 participants were enrolled in a counter balanced protocol containing four different nap conditions. Sleep was measured using Polysomnography. Subjective wellbeing was measured using Questionnaires and performance was measured using computerized tasks quantifying vigilance, prefrontal functioning and motor functioning Results When comparing subjective sleepiness before and after the naps, participants reported being more fatigued after the nap as compared to before the nap in condition S1, S2 and S2max. -

The Benefits of Sleep and the Power Nap by Elizabeth Scott, M.S
The Benefits of Sleep and the Power Nap By Elizabeth Scott, M.S. Why a Power Nap? Facts on Sleep: While small children typically take naps in the afternoon, our culture generally frowns upon mid-day sleep; however, even in those who get enough sleep (but particularly in those who don’t, many people experience a natural decrease in drowsiness in the afternoon, about 8 hours after waking. Research shows that you can make yourself more alert, reduce stress and improve cognitive functioning with a nap. Mid-day sleep or a “power nap, means more patience, less stress, better reaction time, increased learning, more efficiency and better health. Here’s what you need to know about the benefits of sleep and how a power nap can help you. How Much Sleep Do You Need? The body needs 7-8 hours of sleep per day; 6 hours or less triples your risk of a car accident. Interestingly, too much sleep – more than 9 hours- can actually be harmful for your health; recent studies show that those who sleep more than 9 hours a day don’t live as long as their 8-hour counterparts. The Effects of Missed Sleep: Sleep is cumulative; if you lose sleep one day, you feel it the next. If you miss adequate sleep several days in a row, you build up a “sleep deficit”, which impairs the following: • Reaction time • Judgment • Vision • Information processing • Short-term memory • Performance • Motivation • Vigilance • Patience Fatigues people also experience more moodiness, aggressive behaviors, burnout and more stress. The Benefit of a Power Nap: Studies show that 20 minutes of sleep in the afternoon provides more rest than 20 minutes more sleep in the morning ( thought the last two hours of morning sleep have special benefits of their own). -

Sleepiness & Driving
Sleepiness & Driving Facts and Tips HAVE YOU EVER DRIVEN WHILE DROWSY? Many people drive while they are drowsy. Some are able to recognise that there is a problem, but most are unaware that their driving is being affected. CONTACT US T +61 2 9114 0000 F +61 2 9114 0010 E [email protected] 431 Glebe Point Road Glebe NSW 2037 www.woolcock.org.au v1 SLEEPY DRIVING WHAT ARE THE WARNING SIGNS? DOES CAFFEINE OR SUGAR HELP? Sleepy drivers start yawning, their eyes go out of focus and Usually there are warning signs indicating that there is a high Caffeine does offer some short term help with alertness they cannot remember driving the last few kilometres. risk that an accident will occur: which may assist for an hour or two. Take the coffee or tea A survey in the US found that as many as six in ten drivers • Sleepiness before your nap so by the time you have completed your 15 drive while they are drowsy. The problem is that people are • Eyes closing or going out of focus minute nap, the caffeine will be in your body system. very bad at knowing whether it is affecting their driving and whether they are too drowsy to drive. Falling asleep happens • Trouble keeping the head up Sugar is not helpful. After 30 - 90 minutes it can make you quickly and without much warning. • Cannot stop yawning sleepier than if you had no sugar. • Wandering thoughts, difficulty concentrating on driving HOW DOES SLEEPINESS AFFECT YOUR • Cannot remember driving the past few kilometres HOW MANY ACCIDENTS ARE CAUSED BY DRIVING? • Drifting between lanes, off the road or missing signs DROWSY DRIVERS? If you drive after 17 hours without sleep, your performance • Very heavy eyelids Road accident statistics show that at least one in six crashes is as bad as driving with a blood alcohol level of 0.05% (the • Slow blinking are mainly the result of drivers not concentrating and paying equivalent of two standard drinks in the first hour for males attention to the road. -

There's a Sweet Spot for Making Your Power Nap Count
There's a Sweet Spot for Making Your Power Nap Count AO Alexandra Ossola Aug 17 2017, 1:00pm https://tonic.vice.com/ Milles Studio/Stocksy Consider this before your next mid-day snooze. It's happened to all of us: Our night selves screw over our morning selves. You stayed up too late having fun or working hard, and the next day you can barely stay awake. All you can think about is a glorious 20-minute rest to embolden you for the rest of your day. But will all those extra ZZZ's really help you concentrate better, or be more creative? The short answer is yes. But you have to be careful how you do it. Sleep varies a lot between individuals. How much you need per night, the best stage of sleep from which you should wake—all of that can vary depending on your genetics, your age, and your personality, says Rebecca Spencer, an associate professor of psychological and brain sciences at the University of Massachusetts, Amherst. Culture can play a role, too; in Spain, for example, the siesta culture means more sleep during the day but less at night. But in America, there's a trend that supersedes these individual differences: Americans are more sleep-deprived than ever. More than a third of us aren't getting enough sleep, according to a 2016 report from the Centers for Disease Control and Prevention. Over time, too little sleep has been associated with an increased risk of a number of chronic health conditions, like obesity, diabetes, heart disease, mood disorders like depression and anxiety, and alcoholism. -
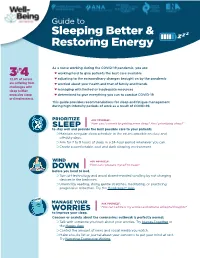
Guide to Sleeping Better & Restoring Energy
Guide to Z Sleeping Better & Z Z Restoring Energy n As a nurse working during the COVID-19 pandemic, you are: i 3 4 ❤ working hard to give patients the best care available 72.8% of nurses ❤ adjusting to the extraordinary changes brought on by the pandemic are suffering from ❤ worried about your health and that of family and friends challenges with sleep (either ❤ managing with limited or inadequate resources excessive sleep ❤ determined to give everything you can to combat COVID-19 or sleeplessness). This guide provides recommendations for sleep and fatigue management during high-intensity periods of work as a result of COVID-19. PRIORITIZE ASK YOURSELF: Z “How can I commit to getting more sleep? Am I prioritizing sleep?” Z Z SLEEP to stay well and provide the best possible care to your patients. ❍ Maintain a regular sleep schedule to the extent possible on duty and off-duty days. ❍ Aim for 7 to 9 hours of sleep in a 24-hour period whenever you can. ❍ Create a comfortable, cool and dark sleeping environment. WIND ASK YOURSELF: DOWN “How can I prepare myself to sleep? before you head to bed. ❍ Turn off technology and avoid absent-minded scrolling by not charging devices in the bedroom. ❍ Unwind by reading, doing gentle stretches, meditating, or practicing progressive relaxation. Try the Headspace® App. MANAGE YOUR ASK YOURSELF: WORRIES “How can I address my worries and reframe unhelpful thoughts? to improve your sleep. Concern or anxiety about the coronavirus outbreak is perfectly normal. ❍ Talk with someone you trust about your worries. Try Nurses Together or the Happy App. -

Power Napping for Performance Improvement in Sports and at Work FIRSTBEAT HRV SUMMIT 2019
Power napping for performance improvement in sports and at work FIRSTBEAT HRV SUMMIT 2019 KASPER JANSSEN SPORT & EXERCISE PHYSICIAN Perform 2 I am… Powernap Recreational athlete Sport & exercise physician - Specializing in sleep & recovery Researcher - PhD Sports, lifestyle & health group Nap@Work - Consultant sleep & recovery for performance Author Out now ‘Powernap paradox’ ARKO sports media Perform 2 Short Quizzz Powernap ‘I sleep during the day, in between training sessions, and I go to bed every night at 9pm.’ 3 questions think fast and respond Perform 2 1. Who is having a power nap here? Powernap WCWC 2017:2018: silvergold medal, with one arm OS 2016: he fell… A. Swimmer Pieter vd Hoogenband B. Soccer player Frenkie de Jong C. Gymnast Epke Zonderland Perform 2 2. How many hours does a Dutch Powernap elite athlete sleep? A. 7 h B. 8 h C. 9 h D. 10 h B. 8 h Thesis Knufinke et al 2018 Perform 2 3. When sleep deprived, for how Powernap many hours can a powernap of just 10 min improve fatigue and cognitive performance? A. 1 h B. 2 h C. 3 h D. 4 h C. 3 hours! Perform 2 Powernap 2 Perform: evidence in sports? Powernap Conclusion: Under certain circumstances, like sleep deprivation, power napping has a positive effect on recovery, specific physical performance, alertness, responsiveness and mood in athletes. Discussion and recommendations: The quality of studies on power napping in athletes varies widely, the number of participants is limited and the definitions used vary. Therefore, further research is needed. Janssen KW, Veldhuizen M, Abstract Dutch Sports Medicine Conference, 2018 Perform 2 POWERNAP: 10-25min Powernap Fall asleep & wake-up: only light sleep Compelling research on: Improved alertness & focus * Effective against fatigue Improved short term memory Enhances learning (cognitive + motor tasks) * Alertness management: strategic naps in operational settings.