Wolf-Ebook.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Search for the "Manchurian Candidate" the Cia and Mind Control
THE SEARCH FOR THE "MANCHURIAN CANDIDATE" THE CIA AND MIND CONTROL John Marks Allen Lane Allen Lane Penguin Books Ltd 17 Grosvenor Gardens London SW1 OBD First published in the U.S.A. by Times Books, a division of Quadrangle/The New York Times Book Co., Inc., and simultaneously in Canada by Fitzhenry & Whiteside Ltd, 1979 First published in Great Britain by Allen Lane 1979 Copyright <£> John Marks, 1979 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner ISBN 07139 12790 jj Printed in Great Britain by f Thomson Litho Ltd, East Kilbride, Scotland J For Barbara and Daniel AUTHOR'S NOTE This book has grown out of the 16,000 pages of documents that the CIA released to me under the Freedom of Information Act. Without these documents, the best investigative reporting in the world could not have produced a book, and the secrets of CIA mind-control work would have remained buried forever, as the men who knew them had always intended. From the documentary base, I was able to expand my knowledge through interviews and readings in the behavioral sciences. Neverthe- less, the final result is not the whole story of the CIA's attack on the mind. Only a few insiders could have written that, and they choose to remain silent. I have done the best I can to make the book as accurate as possible, but I have been hampered by the refusal of most of the principal characters to be interviewed and by the CIA's destruction in 1973 of many of the key docu- ments. -

1969 Board Room (V'
AGENDA Thirty-second Meeting of the BOARD OF REGENTS National Library of Medicine 9:00 a.m., March 2U-25, 1969 Board Room (v' I. CALL TO ORDER AND INTRODUCTORY REMARKS Dr. Stewart Wolf II. CONSIDERATION OF MINUTES OF LAST MEETING TAB I Dr. Stewart Wolf (orange book) III. DATES OF FUTURE MEETING TAB II Dr. Stewart Wolf 1969-70 Calendars in all books Next meeting - June 19-20, 1969 Subsequent Meeting - November 20-21, 1969 Selection of Meeting Date - March 1970 Date circled is one preferred -^ Possible dates: 19-20, 23-21* , (26-27J IV. REMARKS BY THE ASSISTANT SECRETARY FOR HEALTH AND SCIENTIFIC AFFAIRS V. REPORT OF THE DIRECTOR, NLM TAB III Dr. Martin Cummings •I. CONFERENCE ON COMMUNICATIONS FOR MEDICAL TAB IV Dr. Stewart Wolf EDUCATION AND RESEARCH a. History b. Purpose VII. ASSOCIATION OF AMERICAN MEDICAL COLLEGES/ Dr. Cheves Smythe COUNCIL OF ACADEMIC SOCIETIES - REPORT ON NLM CONFERENCE VIII. REPORT ON ORAL HISTORY PROGRAM TAB V Dr. Peter Olch LUNCH EXTRAMURAL PROGRAMS IX. REPORT OF THE ASSOCIATE DIRECTOR, EP Mr. David Kefauver DRG Administrative Report TAB I (gray book) CONSIDERATION OF PENDING APPLICATIONS A. RESEARCH AND PUBLICATION GRANTS TAB II B. TRAINING GRANTS TAB III REPORT OF THE TECHNICAL ADVISORY TAB VI Mr. Edward McClellan COMMITTEE, NATIONAL MEDICAL (orange book) AUDIOVISUAL CENTER XI. INTRODUCTION OF DR. MARSHALL W. NIRENBERG Dr. Martin Cummings (Nobel Laureate for 1968) Film Showing: "DNA: Blueprint for Life" Presentation of: "The Genetic Code - and How it Works" (Exhibit on display in NLM Lobby) ADJOURNMENT DINNER (DUTCH TREAT) - Ballroom of the Walter Reed Army Medical Center Officers Open Mess Bus departs Library 6:30 - stopping at three Bethesda motels enroute and for return. -

The Clinical Evaluation of New Drugs New York: Hoeber-Harper
(4) Fourteen Authors [SO Waife and AP Shapiro (eds)] (1959) The Clinical Evaluation of New Drugs New York: Hoeber-Harper Preamble There is a facsimile of the frontispiece at the James Lind Library (www.jameslindlibrary.org/waife-so-shapiro-ap-1959). The title page states simply “By Fourteen Authors” and the two editors, Waife and Shapiro, are identified only in the last sentence of the Preface. Aims This book is written for the many who participate in the search for and evaluation of better and safer drugs to treat human disease. Because more and more scientists, both medical and allied workers, find themselves planning clinical trials, administering new drugs, observing reactions, and evaluating results, dissemination of knowledge of the proper techniques for these activities has become extremely important. Interest in the methods and techniques of clinical research is high and, of course, reflects the realisation of the numerous pitfalls and problems in human experimentation. This book, then, deals with experimental method and design, in the proper evaluation of new drugs in that most unpredictable of animals – man. It is offered to both the career investigator and the part-time researcher with the objective of improving the calibre of the clinical trial in order to define more accurately and rapidly the potentials of new drugs (Preface, pages ix and x). Contents (xii+223 pages) Contributing authors Preface (SO Waife, AP Shapiro) Part I: Principles of drug evaluation 1) Statement of the problem (SO Waife) 2) Pharmacologic problems (KH -

NLM Board of Regent's Minutes, 1968
AGENDA Twenty-ninth Meeting of the BOARD OF REGENTS National Library of Medicine March 11, 1968 9:00 a.m. Board Room March 12, 1968 9:00 a.m. Atlanta, Georgia I. CALL TO ORDER AND INTRODUCTORY REMARKS Dr. Barnes Woodhall II. CONSIDERATION OF MINUTES OF LAST MEETING Dr. Barnes Woodhall TAB I (orange book) III. DATES OF FUTURE MEETINGS Dr. Barnes Woodhall 1968 Calendars in all books TAB II Next Meeting - June 20-21, 1968 Consideration of Change in Meeting Date - Nov. 7-8, 1968 Other Possible Dates: 18-19, 21-22, Selection of Meeting Date - March 1969 Possible Dates:2U-25,(27^2B} (circled dates represent first choice) IV. OPENING REMARKS FROM THE SURGEON GENERAL V. REPORT OF THE EXTRAMURAL PROGRAMS Mr. David Kefauver TAB I (gray book) VI. CONSIDERATION OF PENDING APPLICATIONS Mr. David Kefauver A. RESEARCH AND PUBLICATION GRANTS TAB II B. TRAINING GRANTS TAB III C. MEDICAL LIBRARY RESOURCE GRANTS TAB IV D. REGIONAL MEDICAL LIBRARY GRANTS TAB V E. CONSTRUCTION GRANTS (green books) LUNCH - Billings Auditorium VII. SURVEY OF HEW SCIENTIFIC INFORMATION Miss Mary Corning ACTIVITIES TAB III (orange book) VIII. REPORT ON MEDLARS EVALUATION STUDY Mr. Frederick Lancaster TAB IV IX. REPORT ON RESEARCH AND DEVELOPMENT ACTIVITIES TAB V A. Medlars II Evaluation - Status Report Mr. Davis McCarn B. The Remote Information Systems Center Mr. Ralph Simmons C. The Specialized Education Services Component Dr. Ruth Davis of the Biomedical Communications Network DEPARTURE FOR AIRPORT BY BUS - l»:30 DUTCH TREAT COCKTAIL PARTY - 8:U5 p.m., SHERATON EMORY, SEVILLE ROOM (main floor) (across the street from NMAC) March 12, 1968 National Medical Audiovisual Center National Communicable Diseases Center Building #3 - Room B19 1600 Clifton Road, N.E. -

DIAGNOSIS, TREATMENT and UNDERSTANDING C.1960–2010
MIGRAINE: DIAGNOSIS, TREATMENT AND UNDERSTANDING c.1960–2010 The transcript of a Witness Seminar held by the History of Modern Biomedicine Research Group, Queen Mary, University of London, on 28 May 2013 Edited by C Overy and E M Tansey Volume 49 2014 ©The Trustee of the Wellcome Trust, London, 2014 First published by Queen Mary, University of London, 2014 The History of Modern Biomedicine Research Group is funded by the Wellcome Trust, which is a registered charity, no. 210183. ISBN 978 0 90223 894 7 All volumes are freely available online at www.history.qmul.ac.uk/research/modbiomed/ wellcome_witnesses/ Please cite as: Overy C, Tansey E M. (eds) (2014) Migraine: Diagnosis, treatment and understanding c.1960–2010. Wellcome Witnesses to Contemporary Medicine, vol. 49. London: Queen Mary, University of London. CONTENTS What is a Witness Seminar? v Acknowledgements E M Tansey and C Overy vii Illustrations and credits ix Abbreviations and ancillary guides xi Introduction Giles Elrington xiii Transcript Edited by C Overy and E M Tansey 1 Appendix 1 Theories of migraine 1900–1960: a brief background to the Wellcome Witness Seminar Mark Weatherall 87 Appendix 2 Summary of the classification of primary headaches, adapted from the Headache Classification Committee of the International Headache Society (IHS) (2013), 636–37 91 Appendix 3 The Role of the UK Specialist Nurse in Headache Ria Bhola and Victoria Quarshie, Headache Nurse Specialists 93 Biographical notes 99 References 111 Index 125 Witness Seminars: Meetings and Publications 137 WHAT IS A WITNESS SEMINAR? The Witness Seminar is a specialized form of oral history, where several individuals associated with a particular set of circumstances or events are invited to meet together to discuss, debate, and agree or disagree about their memories. -

Serotonin (5-HT) and Its Role in the Treatment of Migraine
Molecular Mimicry of Anti-migraine Drugs with the Neurotransmitters, Dopamine (DA) & Serotonin (5-HT) and its Role in the Treatment of Migraine A thesis submitted in partial fulfilment of the requirements for the Degree of Master of Science in Biochemistry In the School of Physical and Chemical Sciences at the University of Canterbury New Zealand By Nancy Joy University of Canterbury 2019 Acknowledgements Special thanks to my supervisor Prof. Ian. C. Shaw for all the discussions to support my thesis and fun lunch outs with our research group team members, who also supported me with molecular modelling guidance especially by Sam and Hector. Special mention to Rachel for taking the extra effort in booking our team meetings online David Zehms for helping me out in reviewing my thesis documents and Parvesh for the humorous talks and making our discussions fun filled moments. Key words Molecular mimicry, serotonin receptors, dopamine receptors, serotonin, dopamine, tyramine, monoaminergic neurons, migraine, migraine treatment, G protein-coupled receptors, neurotransmission, synaptic regulatory receptors and transporters, nociception, nociceptive afferents, neurovascular disorders, brain nuclei, trigeminal nervous system, trigeminal ganglion, vasoactive biochemicals and neuropeptides, insilico molecular modelling. Dedicated to the fond memories of my past professional life which shaped me to be who I am today, to my family & loved ones who have supported me through my struggles, to my aspirations to be a successful professional, and to my dreams: -

Download Full Book
Migraine Foxhall, Katherine Published by Johns Hopkins University Press Foxhall, Katherine. Migraine: A History. Johns Hopkins University Press, 2019. Project MUSE. doi:10.1353/book.66229. https://muse.jhu.edu/. For additional information about this book https://muse.jhu.edu/book/66229 [ Access provided at 24 Sep 2021 04:55 GMT with no institutional affiliation ] This work is licensed under a Creative Commons Attribution 4.0 International License. Migraine This page intentionally left blank Migraine A HISTORY ✷ ✷ ✷ Katherine Foxhall Johns Hopkins University Press, Baltimore This book was brought to publication with the generous assistance of the Wellcome Trust. © 2019 Johns Hopkins University Press This work is also available in an Open Access edition, which is licensed under a Creative Commons Attribution–NonCommercial–NoDerivatives 4.0 International License: https://creativecommons.org/licenses/by-nc -nd/4.0/. All rights reserved. Published 2019 Printed in the United States of America on acid-free paper 9 8 7 6 5 4 3 2 1 Johns Hopkins University Press 2715 North Charles Street Baltimore, Maryland 21218-4363 www.press.jhu.edu Library of Congress Cataloging-in-Publication Data Names: Foxhall, Katherine, author. Title: Migraine : a history / Katherine Foxhall. Description: Baltimore : Johns Hopkins University Press, 2019. | Includes bibliographical references and index. Identifiers: LCCN 2018039557 | ISBN 9781421429489 (pbk. : alk. paper) | ISBN 1421429489 (pbk. : alk. paper) | ISBN 9781421429496 (electronic) | ISBN 1421429497 (electronic) | ISBN 9781421429502 (electronic open access) | ISBN 1421429500 (electronic open access) Subjects: | MESH: Migraine Disorders—history Classification: LCC RC392 | NLM WL 11.1 | DDC 616.8/4912—dc23 LC record available at https://lccn.loc.gov/2018039557 A catalog record for this book is available from the British Library. -
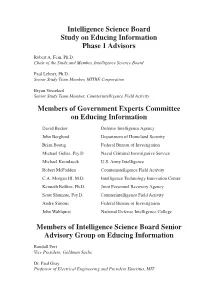
Educing Information, Interrogation: Science and Art, Which Has Four Chapters Devoted to an Overview and Analysis of U.S
Intelligence Science Board Study on Educing Information Phase 1 Advisors Robert A. Fein, Ph.D. Chair of the Study and Member, Intelligence Science Board Paul Lehner, Ph.D. Senior Study Team Member, MITRE Corporation Bryan Vossekuil Senior Study Team Member, Counterintelligence Field Activity Members of Government Experts Committee on Educing Information David Becker Defense Intelligence Agency John Berglund Department of Homeland Security Brian Boetig Federal Bureau of Investigation Michael Gelles, Psy.D Naval Criminal Investigative Service Michael Kremlacek U.S. Army Intelligence Robert McFadden Counterintelligence Field Activity C.A. Morgan III, M.D. Intelligence Technology Innovation Center Kenneth Rollins, Ph.D. Joint Personnel Recovery Agency Scott Shumate, Psy.D. Counterintelligence Field Activity Andre Simons Federal Bureau of Investigation John Wahlquist National Defense Intelligence College Members of Intelligence Science Board Senior Advisory Group on Educing Information Randall Fort Vice President, Goldman Sachs Dr. Paul Gray Professor of Electrical Engineering and President Emeritus, MIT Dr. Margaret A. Hamburg Senior Scientist, Nuclear Threat Initiative Philip B. Heymann James Barr Ames Professor for Criminal Justice, Harvard University Dr. Ernest May Charles Warren Professor of History, Harvard University Dr. Anthony G. Oettinger Chairman, Program on Information Resources Policy, Harvard University Dr. Ervin J. Rokke President, Moravian College About the Intelligence Science Board Mission The Intelligence Science Board was -

Hans Selye and the Transformation of the Postwar Medical Marketplace
City University of New York (CUNY) CUNY Academic Works All Dissertations, Theses, and Capstone Projects Dissertations, Theses, and Capstone Projects 5-2015 The Medicalization of Stress: Hans Selye and the Transformation of the Postwar Medical Marketplace Vanessa L. Burrows Graduate Center, City University of New York How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/gc_etds/877 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] THE MEDICALIZATION OF STRESS: HANS SELYE AND THE TRANSFORMATION OF THE POSTWAR MEDICAL MARKETPLACE BY VANESSA BURROWS A Dissertation submitted to the Graduate Faculty in History in partial fulfillment of the requirements for the degree of Doctor of Philosophy, The City University of New York 2015 © 2015 VANESSA BURROWS All Rights Reserved ii This manuscript has been read an accepted for the Graduate Faculty in History in satisfaction of the dissertation requirement for the degree of Doctor of Philosophy. Gerald Markowitz _______________ ____________________________________ Date Chair of Examining Committee Helena Rosenblatt _______________ ____________________________________ Date Executive Officer David Nasaw____________________________________________ Gerald Oppenheimer______________________________________ Nick Freudenberg________________________________________ David Rosner____________________________________________ -
Emotion Response Patterns to Transient Stimuli in Migraineurs and Non-Migraineurs Modulation of Affective States As a Step Towards Non-Invasive Treatment of Migraine
UNIVERSIDADE DE LISBOA FACULDADE DE CIÊNCIAS FACULDADE DE LETRAS FACULDADE DE MEDICINA FACULDADE DE PSICOLOGIA EMOTION RESPONSE PATTERNS TO TRANSIENT STIMULI IN MIGRAINEURS AND NON-MIGRAINEURS MODULATION OF AFFECTIVE STATES AS A STEP TOWARDS NON-INVASIVE TREATMENT OF MIGRAINE Ana Pesquita MASTER IN COGNITIVE SCIENCE 2010 UNIVERSIDADE DE LISBOA FACULDADE DE CIÊNCIAS FACULDADE DE LETRAS FACULDADE DE MEDICINA FACULDADE DE PSICOLOGIA EMOTION RESPONSE PATTERNS TO TRANSIENT STIMULI IN MIGRAINEURS AND NON-MIGRAINEURS MODULATION OF AFFECTIVE STATES AS A STEP TOWARDS NON-INVASIVE TREATMENT OF MIGRAINE Ana Pesquita Thesis supervised by Prof. A.M. Sebastião, PhD co-supervised by Prof. Dr. P.F.M.J. Verschure MASTER IN COGNITIVE SCIENCE 2010 ACKNOWLEDGMENTS During the making of this thesis I have encountered many people who contributed in different ways to the work and to the enrichment of the personal experience that it constituted. For their supervision, I want to thank Ana Sebastião and Paul F.M.J. Verschure. For creating a space for discussions on Cognitive Science inside Lisbon University, I want to thank the Scientific Committee of the Master in Cognitive Sci- ence and all the remarkable folks I encountered during these studies. The initial phase of this work was developed under the financial support of the INOV-Art Scholarship, an initiative of the Portuguese Ministry Of Culture. Synthetic Perceptive Emotion Cognition Systems Laboratory (SPECS), at Pompeu Fabra University, supported the development of this work and contributed deeply to the scientific insights in it ex- pressed. Aleksander Valjamae supervised the initial phase of this master thesis and, together with Paul F.M.J. -

Medical Center Archives of Newyork-Presbyterian/Weill Cornell
MEDICAL CENTER ARCHIVES OF NEWYORK-PRESBYTERIAN/WEILL CORNELL 1300 York Avenue # 34 New York, NY 10065 Finding Aid To THE HAROLD WOLFF, MD (1898-1962) PAPERS Dates of Papers: 1922-1970 178.5 Linear Inches (26 Boxes, 16 Freestanding Volumes) © 2021 Medical Center Archives of NewYork-Presbyterian/Weill Cornell 2 Abstract One of the leading neurologists of his time, Dr. Harold G. Wolff is generally considered "the father of modern headache research" as well as being a pioneer in the study of psychosomatic illness. The Harold Wolff, MD Papers consist of correspondence, reports, manuscripts and drafts of articles, research notes, lectures, patient records, reprints, and monographs from his time at the New York Hospital-Cornell Medical Center, where he spent most of his career. Provenance These papers were received by the Medical Center Archives on April 14, 1981 from Dr. Eric T. Carlson of the Department of Psychiatry of The New York Hospital-Cornell Medical Center. They had been stored at the Payne Whitney Psychiatric Clinic for an unknown period of time. Biographical Note One of the leading neurologists of his time, Dr. Harold G. Wolff is generally considered "the father of modern headache research" as well as being a pioneer in the study of psychosomatic illness. He spent most of his career at The New York Hospital-Cornell Medical Center. Dr. Wolff was born on May 26, 1898, in New York City the only child of Louis Wolff, an illustrator of Alsatian descent, and Emma Recknagel Wolff. He was educated at City College of New York and Harvard Medical School, from which he graduated in 1923. -

History of Myasthenia Gravis Revisited
154 Arch Neuropsychiatry 2021;58:154−162 REVIEW https://doi.org/10.29399/npa.27315 History of Myasthenia Gravis Revisited Feza DEYMEER İstanbul University Faculty of Medicine Retired Faculty Member, İstanbul, Turkey ABSTRACT The first description of myasthenia gravis (MG) was given by Thomas The hallmark of this period was the use of anticholinesterases and Willis in 1672. MG was the focus of attention after mid-nineteenth thymectomy in the treatment of MG. The third period (1960-1990) century and a great amount of information has been accumulated in a can probably be considered a revolutionary era for MG. Important span of 150 years. The aim of this review is to convey this information immunological mechanisms (acetylcholine receptor isolation, discovery according to a particular systematic and to briefly relate the experience of anti-acetylcholine receptor antibodies) were clarified and the of Istanbul University. MG history was examined in four periods: 1868- autoimmune nature of MG was demonstrated. Treatment modalities 1930, 1930-1960, 1960-1990, and 1990-2020. In the first period (1868- which completely changed the prognosis of MG, including positive 1930), all the clinical characteristics of MG were defined. Physiological/ pressure mechanic ventilation and corticosteroids as well as plasma pharmacological studies on the transmission at the neuromuscular exchange/IVIg and azathioprine, were put to use. In the fourth period junction were initiated, and the concept of repetitive nerve stimulation (1990-2020), more immunological progress, including the discovery of emerged. A toxic agent was believed to be the cause of MG which anti-MuSK antibodies, was achieved. Videothoracoscopic thymectomy appeared to resemble curare intoxication.