Dopamine Transporter and Reward Anticipation in a Dimensional Perspective: a Multimodal Brain Imaging Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Direction Départementale Des Territoires De L'essonne Septembre
Les missions de la direction Direction départementale départementale des territoires (DDT) des territoires de l’Essonne Sous l'autorité du Préfet de l'Essonne, la DDT met en œuvre les politiques des ministères de la transition écologique et solidaire, de la cohésion des territoires et de l'agriculture. La DDT accompagne les collectivités dans l'élaboration DDT de l'ESSONNE de leur document de planification Boulevard de France 91012 ÉVRY-COURCOURONNES et dans tous leurs projets d'aménagement, Fax : 01 69 91 13 99 de logement et de renouvellement urbain. [email protected] En matière de droit des sols, la DDT conseille les collectivités et calcule les redevances. Elle instruit les permis de construire de compétence État. Elle contribue aux politiques d'accessibilité et de construction durable. Étampes La DDT met en œuvre les aides de l'État pour les logements sociaux, les aides de l'agence nationale pour la rénovation urbaine (ANRU), ainsi que les aides de l'agence nationale de l'habitat (ANAH) pour l'amélioration DRIEA/GAUTHIER du parc privé. La DDT promeut le développement durable des territoires, dans le respect des espaces naturels et agricoles. Elle concourt à la prévention des risques, anime la mission inter-services de l'eau et de la nature (MISEN), Boulevard de France veille à la protection des espèces et assure le suivi Accès de 9h00 à 16h00 : de la chasse. ● En transport en commun : 91012 ÉVRY-COURCOURONNES Cedex RER D (Paris-Malesherbes, Paris-Melun via Corbeil), gare d’Évry-Courcouronnes, sortie Cours Blaise Pascal (33 minutes depuis Paris gare de Lyon + 10 minutes de Tél. -

Country Report: France
Country Report: France 2020 Update 2020 Update Acknowledgements & Methodology The 2020 update of this report was written by Laurent Delbos and Claire Tripier at Forum réfugiés – Cosi and edited by ECRE. Forum réfugiés-Cosi wishes to thank all those individuals and organisations who shared their expertise to contribute or check the information gathered during the research. Particular thanks are owed to many Forum réfugiés-Cosi colleagues who have shared their practical experience on the right of asylum in France – which have been key to feed concrete reality-checks and observations into this report; to the two lawyers who have taken the time to share their views on the French system; to the staff of France terre d’asile, the Anafé and the UNHCR Paris office for their expert and constructive feedback provided for the initial report and finally to ECRE for its support throughout the drafting process. Forum réfugiés- Cosi would also like to thank the European Asylum, Migration and Integration Fund (AMIF) for co-financing its awareness-raising missions which allowed us to provide additional time to research and draft this report. The findings presented in this report stem from background desk research, interviews with field practitioners and lawyers, as well as feedback from French NGOs and the Paris-based UNHCR office and finally statistics shared by the French authorities. Caveat: In France, asylum policies – including reception procedures – are largely under prefectural execution. This review of practice is mostly based on observations in the departments of Ile de France, Rhône, Puy-de-Dôme, Haute- Garonne and Alpes-Maritimes. However, the conclusions presented in this report on the concrete implementation of asylum policies have been cross-checked and triangulated with observations of these practices in other regions and are supported by findings presented in other reports – be they official or drafted by civil society organisations. -

Groupements Ordonnes De Communes Des Yvelines (78)
Annexe page III GROUPEMENTS ORDONNES DE COMMUNES DES YVELINES (78) VERSAILLES et sa région SAINT-GERMAIN-EN-LAYE et sa région MANTES et sa région 078954 078955 078956 1 : VERSAILLES (SL, Mp, RER-C) 1 : SAINT-GERMAIN-EN-LAYE (RER-A) 1 : MANTES-LA-JOLIE (SL) 2 : LE CHESNAY (SL, RER-C) (4 km) 2 : LE PECQ (RER-A) (5 km) 2 : MANTES-LA-VILLE (SL) 3 : VIROFLAY (SL, Mp, RER-C) (4 km) 3 : MAISONS-LAFFITTE (SL, RER-A) (5 km) 3 : LIMAY (SL) (2 km) 4 : BUC (Mp, RER-C) (4 km) 4 : MONTESSON (SL, RER-A) (5 km) 4 : MAGNANVILLE (SL) (2 km) 5 : SAINT-CYR L’ECOLE (Mp, RER-C) (4 km) 5 : POISSY (SL, RER-A) (5 km) 5 : PORCHEVILLE (SL) (5 km) 6 : VELIZY-VILLACOUBLY (Mp, SL, RER-C) (5km) 6 : SARTROUVILLE (SL , RER-A) (5 km) 6 : ISSOU (SL) (5 km) 7 : GUYANCOURT (Mp, RER-C) (5 km) 7 : HOUILLES (SL, RER-A) (5 km) 7 : GARGENVILLE ( SL) (7 km) 8 : FONTENAY - LE - FLEURY (Mp) (6 km) 8 : CARRIERES-SOUS-POISSY (SL, RER-A) (5 km) 8 : ROSNY-SUR-SEINE (SL) (8 km) 9 : NOISY LE ROI (SL) (7 km) 9 : ACHERES (RER-A) (5km) 9 : EPONE (SL) (9 km) 10 : BOIS-D’ARCY (Mp, RER-C) (7km) 10 : ANDRESY (SL) (6 km) 10 : AUBERGENVILLE (SL) (11 km) 11 : MONTIGNY - LE - BRETONNEUX (Mp, RER-C) 11 : LE VESINET (RER-A, N) (6 km) 11 : BONNIERES-SUR-SEINE (SL) (11 (8 km) 12 : CHANTELOUP (SL) (7 km) km) 12 : VOISINS- LE- - BRETONNEUX (Mp, RER-C) (8 13 : CHATOU ( RER-A) (7 km) 12 : BREVAL (SL) (13 km) km) 14 : CROISSY-SUR SEINE (RER-A) (7 km) 13 : MAULE (Mp, SL) (14 km) 13 : MAGNY –LES-HAMEAUX (Mp, RER-C) (8 km) 15 : CARRIERE-SUR –SEINE (SL, RER-A) (7 km) 14 : LES MUREAUX (SL) (15 km) 14 : VILLEPREUX -

Les Antennes VAE En Ile-De-France
Les antennes VAE en Ile-de-France Antennes VAE à Paris (75) Ville Coordonnées Téléphone E-mail Paris 7 rue Beaujon 75008 PARIS 01 55 65 63 10 antenne.vae75@infovae -idf.com Antennes VAE en Seine-et-Marne (77) Ville Coordonnées Téléphone E-mail Melun 51 Avenue Thiers 77000 Melun 01 64 45 18 58 antenne.vae77@infovae -idf.com Meaux Maison de l’Emploi du Nord -Est 77 01 64 45 18 58 antenne.vae77@infovae -idf.com 12 boulevard Jean-Rose - BP 103 77105 Meaux cedex Torcy 31 avenue Jean Moulin 01 64 45 18 58 antenne.vae77@infovae -idf.com Immeuble Buropark Jean Moulin 77200 TORCY Antennes VAE dans les Yvelines (78) Ville Coordonnées Téléphone E-mail Trappes 01 30 12 16 30 antenne.vae78@infovae -idf.com Montigny le 17 rue Joël le Theule 01 30 12 16 30 antenne.vae78@infovae -idf.com Bretonneux 78180 Montigny le Bretonneux Mantes 01 30 12 16 30 antenne.vae78@infovae -idf.com Magnanville Chanteloup 01 30 12 16 30 antenne.vae78@infovae -idf.com les Vignes Antennes VAE dans l’Essonne (91) Ville Coordonnées Téléphone E-mail Etampes 4 avenue Geoffroy Saint -Hilaire 01 60 77 50 24 antenne.vae91@infovae -idf.com 91150 Etampes Evry 8 rue Montespan 01 60 77 50 24 antenne.vae91@infovae -idf.com 91000 Evry Briis - Communauté de Communes du 01 60 77 50 24 antenne.vae91@infovae -idf.com sous- Pays de Limours Forges 615 rue Fontaine de Ville 91640 Briis sous Forges Antennes VAE dans les Hauts-de-Seine (92) Ville Coordonnées Téléphone E-mail Nanterre Maison de l'Emploi et de la 01 47 29 79 79 antenne.vae92@infovae -idf.com Formation 63 avenue Georges Clemenceau -

The Member States and Regions Referred to Respectively In
No L 13/14 Official Journal of the European Communities 21 . 1 . 93 COMMISSION DECISION of 21 December 1992 recording the compliance by certain Member States or regions with the requirements relating to brucellosis (B. melitensis) and according them the status of a Member State or region officially free of the disease (93/52/EEC) THE COMMISSION OF THE EUROPEAN COMMUNITIES, HAS ADOPTED THIS DECISION : Having regard to the Treaty establishing the European Economic Community, Article 1 Having regard to Council Directive 91 /68/EEC of The Member States and regions referred to respectively in 28 January 1991 on animal health conditions governing Annexes I and II satisfy the conditions laid down in intra-Community trade on ovine and caprine animals ^), Directive 91 /68/EEC, Annex A, Chapter 1 .II ( 1 ) (b). and in particular Annex A, Chapter 1 .II thereof, Whereas, in the United Kingdom, Ireland, the Nether Article 2 lands, Belgium, Luxembourg, the Federal Republic of Germany and certain regions in France, brucellosis (B. The Member States and regions referred to respectively in melitensis) has been a notifiable disease for at least five Annexes I and II are recognized as officially free of years ; whereas no case has been confirmed officially there brucellosis (B. melitensis). for at least five years and vaccination has been banned there for at least three years ; whereas it should therefore be put on record that they comply with the conditions Article 3 laid down in Annex A, Chapter 1 .II ( 1 ) (b); This Decision is addressed to the Member States. Whereas, in addition, the Member States or regions referred to above undertake to satisfy the provisions laid down in Annex A, Chapter 1.II (2); whereas, conse quently, the Member States and regions in question Done at Brussels, 21 December 1992. -

L'essonne En Chiffres 2020
ESSONNE EN CHIFFRES La CCI Essonne et la CMA Essonne remercient leurs partenaires pour leur précieuse contribution à la réalisation de cette publication. 2020 u ACOSS u INPI u ADP u INSEE u Agence Bio u ISM u Agreste MSA u MENESR u CD 91 u ORS u DDT Essonne u Rectorat de Versailles u DGFIP u SITADEL u DREES u DSDEN 91 u HAROPA - Ports de Paris Seine Normandie Informations légales. Éditeurs : CCI Essonne et CMA Essonne - Codirecteurs de la publication : Didier Desnus, Président CCI Essonne et Laurent Munerot, Président CMA Essonne - Codirecteurs de la rédaction : Bruno Malecamp, Directeur général CCI Essonne et Florence Galiez, Secrétaire Général CMA Essonne - Mise en page : Pellicam - Impression : Willaume Egret - Dépôt légal à parution septembre 2020 2, cours Monseigneur Romero - CS 50135 29, allée Jean Rostand - CS 20543 imprimé sur papier issu de forêts gérées durablement - Ne pas jeter la voie publique Mise en page : 91004 Évry-Courcouronnes cedex 91025 Évry-Courcouronnes cedex 01 60 79 91 91 01 69 47 54 20 L’essentiel des données socio-économiques essonne.cci.fr cma-essonne.fr de l’Essonne essonne.cci.fr cma-essonne.fr CHIFFRES CLÉS 03 Le dynamisme de l’artisanat et des entreprises locales rayonne sur le territoire essonnien. Présence territoriale, emploi local, TERRITOIRE formation des jeunes et insertion INNOVATION / R&D ACTIVITÉS ÉCONOMIQUES sociale, développement durable, lien Superficie (km2) social, agilité et adaptabilité : dans ces Eectifs salariés périodes diciles, nos entreprises répondent aux attentes de la 95 995 1 804 (33 % de l'IDF) établissements Source : Insee 2017 population et endossent un rôle 13 750 économique et humain primordial. -

Middle Ages and Early Modern Times), 10-12 June 2021
Call for Papers: Forms of trade regulation 4th International Workshop The spatial implications of trade regulations (Middle Ages and Early Modern Times), 10-12 June 2021 After the three meetings in 2017, 2018, and 2019, the investigation into The forms of trade regulations in medieval and modern Europe continues with a fourth and final international conference on the spatial dimension of professional regulations. While Europe, in a broad sense, has been chosen as a starting point, papers could also consider other cultural areas or colonial experiences. As a reminder, regulations are viewed as a process, from the making of the rules to their implementation, without being restricted either to the written and stabilised forms of the statutes or to organisations of a corporative nature: royal or local orders, judicial precedents, or unwritten customs could also be part of the normative framework of trades, just as non-institutional groups could regulate themselves through the manufacture or sale of a particular product. The diffusion and spatial concentration of these different types of regulations in medieval and early modern societies can thus be investigated on various scales: from the much discussed area of influence of local trade associations to the norms that apply to larger territories or networks, such as the legislations on prices and wages adopted by several kingdoms after the end of the 13th century, the Hanseatic Leagues, the inspection of factories, journeymen’s associations, and so on. 1/- How were legal spaces established: -

Local and Regional Government* Rating Review Calendar 2021
Local and Regional Government* Rating Review Calendar 2021 Rating Reviews, by Entity. This calendar is reviewed and updated as necessary at the end of each quarter. Last updated: 30th June 2021 Entity Aix-Marseille-Provence Metropolis Friday 30 April 2021 Friday 29 October 2021 Alava, Historical Territory of Friday 30 April 2021 Friday 29 October 2021 Almaty, City of Friday 26 February 2021 Friday 20 August 2021 Altai Region Friday 14 May 2021 Friday 12 November 2021 Andalusia, Autonomous Community of Friday 19 March 2021 Friday 17 September 2021 Ankara Metropolitan Municipality Friday 04 June 2021 Friday 03 December 2021 Antalya Metropolitan Municipality Friday 04 June 2021 Friday 03 December 2021 Autonomous Region of Azores Friday 11 June 2021 Friday 03 December 2021 Barcelona, City of Friday 26 February 2021 Friday 20 August 2021 Bashkortostan Republic Friday 14 May 2021 Friday 12 November 2021 Basque Country, Autonomous Community of Friday 30 April 2021 Friday 29 October 2021 Berlin, State of Friday 16 April 2021 Friday 15 October 2021 Bialystok, City of Friday 23 April 2021 Friday 22 October 2021 Bizkaia, Historical Territory of Friday 30 April 2021 Friday 29 October 2021 Bolzano, Autonomous Province of Friday 30 April 2021 Friday 29 October 2021 Bouches du Rhone, Department of Friday 18 June 2021 Friday 17 December 2021 Brasov, City of Friday 07 May 2021 Friday 05 November 2021 Bremen, State of Friday 16 April 2021 Friday 15 October 2021 Bretagne, Region of Friday 09 April 2021 Friday 08 October 2021 Bucharest, City of Friday 07 -

Download Full Book
The French New Towns Rubenstein, James M. Published by Johns Hopkins University Press Rubenstein, James M. The French New Towns. Johns Hopkins University Press, 1978. Project MUSE. doi:10.1353/book.71471. https://muse.jhu.edu/. For additional information about this book https://muse.jhu.edu/book/71471 [ Access provided at 26 Sep 2021 01:34 GMT with no institutional affiliation ] This work is licensed under a Creative Commons Attribution 4.0 International License. HOPKINS OPEN PUBLISHING ENCORE EDITIONS James M. Rubenstein The French New Towns Open access edition supported by the National Endowment for the Humanities / Andrew W. Mellon Foundation Humanities Open Book Program. © 2019 Johns Hopkins University Press Published 2019 Johns Hopkins University Press 2715 North Charles Street Baltimore, Maryland 21218-4363 www.press.jhu.edu The text of this book is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License: https://creativecommons.org/licenses/by-nc-nd/4.0/. CC BY-NC-ND ISBN-13: 978-1-4214-3186-4 (open access) ISBN-10: 1-4214-3186-6 (open access) ISBN-13: 978-1-4214-3184-0 (pbk. : alk. paper) ISBN-10: 1-4214-3184-X (pbk. : alk. paper) ISBN-13: 978-1-4214-3185-7 (electronic) ISBN-10: 1-4214-3185-8 (electronic) This page supersedes the copyright page included in the original publication of this work. THE FRENCH NEW TOWNS JOHNS HOPKINS STUDIES IN URBAN AFFAIRS Center for Metropolitan Planning and Research The Johns Hopkins University David Harvey, Social Justice and the City Ann L. Strong, Private Property and the Public Interest: The Brandywine Experience Alan D. -

France Country Briefing April 2018
France Country Briefing April 2018 Cumulative issuance: EUR37.7bn, 25 green bond issuers in total, 3rd in global rankings 2017 issuance: EUR20.3bn (4.5 times higher than 2016), 13 issuers France boasts one of the first green bond markets. New impetus from state policy supports future growth. Green bond opportunities in France 2017 green bond issuance more than French issuers have propelled the country to an emblematic position. quadrupled from 2016 French green bond issuance commenced in 2012 with the first three 20 Sovereign French deals coming from local government entities Île-de-France, Non-Financial Corporate Provence-Alpes-Côte d'Azur and Hauts-de-France. These pioneering deals Local Government laid a solid foundation. France now boasts the largest green bond market 15 Loan in Europe and the third largest globally. Government-Backed Entity Financial Corporate A burgeoning market, fuelled by non-financial corporate and 10 Development Bank government-backed issuers since 2013, with a recent push from the ABS state. The EUR9.7bn Sovereign Green OAT, the largest green bond ever 5 issued, accounted for nearly half the green bond volume placed by French issuers in 2017. It epitomizes the driving role of France in spurring growth (see detailed analysis on pp. 3-4). 0 EURbn issued EURbn 2012 2013 2014 2015 2016 2017 2018ytd2018* The market has diversified since 2012, welcoming new issuers as well as new instruments. Mid-sized companies such as Neoen, Akuo Energy and Over 60% of proceeds allocated to energy and Foncière INEA are starting to issue green bonds, a healthy sign of evolution building assets/projects for the French market. -

Les Ateliers De Cergy Dessinent La Transition En Essonne Helio Corbeil
Le Conseil d’Architecture, d’Urbanisme et de l’Environnement 91, acteur de l’Essonne en mouvement Les Ateliers de Cergy dessinent la transition en Essonne Décollage imminent pour la BA217 ! Le sud francilien est choisi comme laboratoire de la transition énergétique Un projet de reconversion pour la base aérienne de Brétigny-sur-Orge/Plessis-Pâté Images d’Avenirs parcourt l’Essonne Les surprises du paysage pavillonnaire Une expo de 78 photos interroge l’évolution de nos territoires Quand les jardins privés participent du paysage urbain Helio Corbeil imprime solidaire L’esprit coopératif au coeur d’une entreprise essonnienne tél : 01 60 79 35 44 • [email protected] • www.caue91.asso.fr Les Ateliers de Cergy dessinent la transition en Essonne Les 15 et 16 mai, le CAUE de l’Essonne accueille les «Les ateliers du territoire en mouvement», au Ateliers de Cergy afin de préparer l’appel à candidature service des élus de notre département, le palmarès « Territorialiser la transition énergétique, écologique, d’«Essonne Aménagements Exemplaires» ainsi que urbaine et rurale : le sud francilien comme laboratoire les démarches au service d’une économie sociale et ». L’idée : explorer comment un territoire structuré par solidaire, réunies dans le cadre de «Particip’action» l’accès facile à l’énergie fossile peut inventer et mettre illustrent notre engagement au service de cette en oeuvre sa propre transition, en faisant des choix plus vision plurielle de la fabrique du territoire. sobres en énergie tout en favorisant un cadre de vie plus agréable. Evelyne Lucas, architecte-urbaniste conseiller, directrice du CAUE 91 Faire plancher des étudiants et professionnels du monde entier à un projet de territoire en En savoir plus s’affranchissant des traditionnelles barrières administratives ou institutionnelles, c’est ce que * Consulter le site des ateliers proposent les Ateliers de Cergy depuis plus de trente ans. -
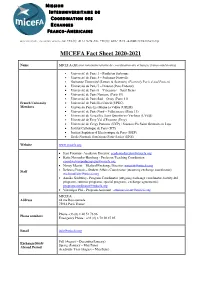
MICEFA Fact Sheet 2020-2021
M ISSION I NTERUNIVERSITAIRE DE C OORDINATION DES E CHANGES F RANCO- A MERICAINS 44 rue Boissonade - 75014 PARIS -FRANCE - Tél. +33 (0)1 40 51 76 96 -Fax. +33 (0)1 44 07 18 10 - e-mail: [email protected] MICEFA Fact Sheet 2020-2021 Name MICEFA (Mission interuniversitaire de coordination des échanges franco-américains) • Université de Paris 1 – Panthéon Sorbonne • Université de Paris 3 – Sorbonne Nouvelle • Sorbonne Université (Lettres & Sciences) (Formerly Paris 4 and Paris 6) • Université de Paris 7 – Diderot (Paris Diderot) • Université de Paris 8 – Vincennes – Saint Denis • Université de Paris Nanterre (Paris 10) • Université de Paris Sud – Orsay (Paris 11) French University • Université de Paris Est Créteil (UPEC) Members • Université Paris Est Marne la Vallée (UPEM) • Université de Paris Nord – Villetaneuse (Paris 13) • Université de Versailles Saint Quentin-en-Yvelines (UVSQ) • Université de Evry Val d’Essonne (Evry) • Université de Cergy Pontoise (UCP) / Sciences Po Saint-Germain-en-Laye • Institut Catholique de Paris (ICP) • Institut Supérieur d’Electronique de Paris (ISEP) • Ecole Normale Supérieure Paris-Saclay (ENS) Website www.micefa.org • Jean Fournier- Academic Director: [email protected] • Katia Nossenko-Hercberg - Professor/Teaching Coordinator: [email protected] • Nancy Merritt – Medical Exchange Director: [email protected] • Staff Rebecca Procak – Student Affairs Coordinator (incoming exchange coordinator): [email protected] • Annika Godefroy– Program Coordinator (outgoing exchange