Draft for Stakeholder Critique
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chiropractic Care of the Older Person: Developing an Evidence-Based Approach
0008-3194/2001/156–171/$2.00/©JCCA 2001 Chiropractic care Chiropractic care of the older person: developing an evidence-based approach Brian J. Gleberzon, DC* Geriatric care has assumed a more dominant position in La gériatrie prend désormais une position plus the health care delivery system. This article discusses the dominante dans le système de distribution des soins results of a literature search on geriatric chiropractic médicaux. Le présent article examine les résultats d’une care with the ultimate goal of promoting a “best recherche documentaire sur les soins chiropratiques practice” approach. Fifty nine articles were found that gériatriques, dont l’objectif final consiste à promouvoir discussed geriatric chiropractic education (N = 3), une démarche basée sur les « meilleures pratiques ». demographic and epidemiological studies (N = 9), case On a repéré 59 articles qui portent sur : la formation studies (N = 25), clinical trials (N = 4) and clinical en chiropratique gériatrique (N = 3), les études guidelines (N = 18). The literature revealed that démographiques et épidémiologiques (N = 9), les études chiropractic pedagogy has recognized the importance of de cas (N = 25), les essais cliniques (N = 4) et les guides geriatric education, and epidemiological studies de pratique clinique (N = 18). La documentation révèle reported an increase in utilization rates of chiropractic que la pédagogie chiropratique a reconnu l’importance care by older persons, along with greater acceptance d’une formation en gériatrie, et les études within the medical community. Most older persons épidémiologiques rapportent une augmentation des taux sought out chiropractic care for neuromusculoskeletal d’utilisation des soins chiropratiques par les personnes (NMS) conditions, with several studies reporting the âgées, ainsi qu’une acceptation accrue de ce type de successful resolution of these conditions with spinal soins au sein de la communauté médicale. -

Appendix J Glossary of Terms Or References
Appendix J Glossary of Terms or References ACA APA American Chiropractic Association American Psychological Association activator technique applied kinesiology A system of adjustment using a hand held, manu The dynamics of smooth and striated muscle and ally assisted, spring activated device which deliv the impact of these tissues on body structure, ers a controlled thrust. healing processes, and disease processes. In particular, applied kinesiology focuses on the acupressure/Meridian therapy identification and correction of proprioceptive The practice of applying digital pressure to stimu dysfunction of ligaments and of the muscle spindle late certain sites on the skin to affect distant cells and golgi tendons. In addition, applied functional mechanisms of the body. This therapy kinesiology is concerned with the vascular, lym is based on the belief that these sites are organized phatic, and othersystems supportingpropermuscle along meridians which carry the life force that dynamics. innervates the body. arterial aneurysm acupuncture An enlargement of one aspect of an artery caused The practice of insertion of needles into specific by weakness in the arterial wall. exterior body locations to relieve pain, to induce surgical anesthesia, and for therapeutic purposes. aseptic necrosis A condition which is not a specific disease entity adjustment but caused by disruption in normal circulation to A forceful thrust which is meticulously con the involved bone. It can result in pain, loss of trolled as to its direction, amount of force em bone density, bone collapse or fracture. Some ployed, and the quickness with which it is ap possible areas of involvement include the hip, plied. shoulder, elbow, wrist, knee, or heel. -

Throm Informed Consent
THROM HEALTH AND WELLNESS Informed Consent to Chiropractic Treatment Summary of Risks: “Chiropractic is widely recognized as one of the safest drug-free, non-invasive therapies available for the treatment of neuromusculoskeletal complaints. Although chiropractic has an excellent safety record, no health treatment is completely free of potential adverse effects. The risks associated with chiropractic, however, are very small. Many patients feel immediate relief following chiropractic treatment, but some may experience mild soreness or aching, just as they do after some forms of exercise. Current literature shows that minor discomfort or soreness following spinal manipulation typically fades within 24 hours.” - American Chiropractic Association (ACA) Website Specific Risks of Treatment: 1. Generalized Soreness: Chiropractic adjustments and trigger point therapy are occasionally associated with post-treatment soreness. Please let your doctor know if you encounter any soreness. Your doctor may provide at-home icing, heating, stretching, or other instructions; or modify your treatment plan to minimize post-treatment soreness. 2. Soft Tissue Injury: Chiropractic treatment and trigger point therapy are rarely associated with soft tissue injuries such as mild sprains, strains, or bruises. Please let your doctor know if you encounter any of these as they may modify your treatment recommendations. 3. Rib Injury/Fracture: Manual adjustments to the thoracic spine may result in rib injuries on rare occasions, most commonly in patients with low bone density. If you or the doctor feel you are at risk based your health history, x-rays may be taken of the thoracic spine and rib region to assess bone density. Patients with low density may opt for lower-force instrument adjustments (Activator Technique). -

Resolution of Constipation and Nocturnal Enuresis in a 10-Year-Old Female Following Adjustment of Vertebral Subluxations
CASE STUDY Resolution of Constipation and Nocturnal Enuresis in a 10-year-old Female Following Adjustment of Vertebral Subluxations : A Case Study Ian Shtulman, DC1 and Mia A. Cunningham, BS, DC2 Abstract Objective: The purpose of this case study is to present findings in which a 10-year-old girl received relief from acute constipation and primary nocturnal enuresis as result of chiropractic care. Clinical Features: This is a case study of a 10-year-old girl who presented to a chiropractic clinic for evaluation with a history of four-day constipation and symptoms of nocturnal enuresis. Previous attempts of fecal disimpaction with the use of probiotics, castor oil and flax seeds were unsuccessful. Intervention and Outcomes: A pediatric patient received subluxation based chiropractic care using Thompson technique protocol that resolved the symptoms of acute constipation and primary nocturnal enuresis. Thompson leg checks were used to determine the area of aberrant biomechanics. Improvement was seen within an hour of reducing cervical and ilium subluxations. On the third visit the mother of the patient revealed that a life time of nocturnal bedwetting three to four times a week had been resolved following her initial chiropractic evaluation and adjustment. Conclusion: This case study provides support that chiropractic care may be beneficial in the management of constipation and nocturnal enuresis. Keywords: Bedwetting, Constipation, Chiropractic, Enuresis, Subluxation, Thompson technique, Adjustment, Spinal manipulation Introduction There are very few benign conditions that are as distressing as constipation includes delayed colonic transit and dysfunction defecation disorders.1 Defecation disorders are a group of of the pelvic floor muscles.3 The prevalence of functional functional and anatomical abnormalities of the anorectum that constipation in children ranges from 4-36%. -

Name: Munyeong Choi
CURRICULUM VITAE Munyeong Choi, D.C., M.S., D.A.C.B.R Chiropractic Radiologist 6525 Shahab Lane, Port Orange, FL, 32128 Phone: (630) 433-0325 Email Address: [email protected] Educational Background Oct 2012 Diplomate, American Chiropractic Board of Lombard, IL Radiology (D.A.C.B.R.) Aug 2012 Master of Science in Diagnostic Imaging Lombard, IL (Summa Cum Laude) Sep 2009 – Residency in Diagnostic Imaging Lombard, IL Aug 2012 National University of Health Sciences Sep 2005 – Doctor of Chiropractic Lombard, IL Dec 2008 National University of Health Sciences (Summa Cum Laude, Salutatorian) Sep 2001 – Completed work for Master of Science in Biology Berrien Springs, MI Aug 2005 Andrews University Mar 1997 – Bachelor of Science in Biology Seoul, South Korea Feb 2001 Sahmyook University (Korean Adventist University) (Summa Cum Laude, Valedictorian) Employment Experience September 2015 – Assistant Professor – Teach X-ray physics, Palmer College of Present special imaging, X-ray positioning and soft tissue Chiropractic, radiology covering abdomen and chest radiology, Port Orange, FL and small group learning sessions. • Course Director: X-ray Physics • Course Director: X-ray Positioning • Course Director: Soft Tissue Radiology • Dourse Director: Special Imaging • Course Contributor: Cardiopulmonary Integrative diagnosis • Course Contributor: X-ray Positioning Page 1 of 9 Dr. Munyeong Choi Chiropractic Radiologist September 2013 – Adjunct Faculty – Teach anatomy and College of DuPage, May 2015 physiology lecture and lab for pre-physical Glen Ellyn, IL therapy, occupational therapy, and nursing students. Jan 2013 – Present Director of Munyeong Choi Diagnostic Imaging Port Orange, FL Consultation – Interpret musculoskeletal diagnostic images including but not limited to plain radiographs and MR studies for health care providers including chiropractic physicians and medical doctors and patients. -
Palmer College of Chiropractic 2017-2018 Catalog
2017-2018 Catalog The Trusted Leader in Chiropractic Education® 1 PALMER COLLEGE OF CHIROPRACTIC CATALOG 2017-2018* Palmer College Foundation doing business as Palmer College of Chiropractic Davenport, Iowa 1000 Brady Street Davenport, IA 52803 (800) 722-2586 (563) 884-5000 Admissions: (800) 722-3648, (563) 884-5656 Email: [email protected] Palmer College Foundation, Inc., doing business as Palmer College of Chiropractic Florida Port Orange, Florida 4777 City Center Parkway Port Orange, FL 32129 (866) 890-5498 Admissions: (866) 585-9677, (386) 763-2709 Email: [email protected] Palmer College of Chiropractic West San Jose, California 90 E. Tasman Drive San Jose, CA 95134 (408) 944-6000 Admissions: (866) 303-7939, (408) 944-6000 Email: [email protected] Palmer College of Chiropractic website www.palmer.edu *RESERVATION OF RIGHTS Palmer College of Chiropractic reserves the right, without notice, to modify its requirements for admission or graduation; to change the arrangements or content of its courses and the instructional materials used, or to alter any regulation affecting the student body; to refuse admission or readmission to any student at any time, or to dismiss any student at any time, should it be in the interest of the College, or of the student, to do so. The College also reserves the same right as to any other material in this catalog. This version of the catalog for Palmer College of Chiropractic can be found on our website: www.palmer.edu. Issued for January 1, 2017 - December 31, 2018, Volume 111. As changes occur, the most up-to-date information can be found on our website: www.palmer.edu Throughout this Catalog as a matter of convenience and consistency, the above corporate and tradenames will be more generally referred to as Palmer College of Chiropractic, Palmer College or the College unless denoting a particular campus. -

Cerebral Hemorrhage Following Chiropractic Activator Treatment – Case Report and Review of Literature
THIEME e162 Case Report Cerebral Hemorrhage Following Chiropractic Activator Treatment – Case Report and Review of Literature Fred L. Cohen1,2 1 Private Practice of Neurological Surgery, Palm Beach Gardens, Address for correspondence Fred L. Cohen, MD, JD, Gary Roberts and Florida, United States Associates, 580 Village Boulevard, Suite 300, West Palm Beach, FL 2 GaryRobertsandAssociates,WestPalmBeach,Florida,UnitedStates 33409, United States (e-mail: [email protected]). J Neurol Surg Rep 2016;77:e162–e167. Abstract Background Despite widespread utilization of chiropractic treatment for various ailments, there is a paucity of documentation regarding intracerebral hemorrhage related to chiropractic trauma. Stroke has been reported from cervical manipulation, although with a suggested low incidence. Activator treatment, an instrument that produces a high-velocity, low-amplitude impact to the spine, is considered especially safe. There are no prior reports of intracerebral hemorrhage resulting from a chiroprac- tic activator treatment. Case Description A 75-year-old woman was admitted to the hospital with a history of headaches, visual difficulties on the right, and speech disturbance of relatively acute onset. CT scan showed a brain hemorrhage in an unusual location. Extensive evaluation was undertaken because this was thought to be a spontaneous event. No cause was found on imaging. Subsequent history revealed a chiropractic activator treatment Keywords applied directly to the junction of the back of her head and the upper cervical spine ► activator immediately prior to the onset of symptoms. Her clinical course is described. ► chiropractic Conclusions This appears to be the first report linking traumatic intracerebral ► stroke hemorrhage with a chiropractic activator treatment. The use of this modality in an ► trauma elderly population, with widespread utilization of anticoagulants and platelet inhibitors, ► cerebral hemorrhage is of potential concern. -
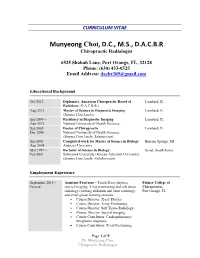
Munyeong Choi, D.C., M.S., D.A.C.B.R Chiropractic Radiologist
CURRICULUM VITAE Munyeong Choi, D.C., M.S., D.A.C.B.R Chiropractic Radiologist 6525 Shahab Lane, Port Orange, FL, 32128 Phone: (630) 433-0325 Email Address: [email protected] Educational Background Oct 2012 Diplomate, American Chiropractic Board of Lombard, IL Radiology (D.A.C.B.R.) Aug 2012 Master of Science in Diagnostic Imaging Lombard, IL (Summa Cum Laude) Sep 2009 – Residency in Diagnostic Imaging Lombard, IL Aug 2012 National University of Health Sciences Sep 2005 – Doctor of Chiropractic Lombard, IL Dec 2008 National University of Health Sciences (Summa Cum Laude, Salutatorian) Sep 2001 – Completed work for Master of Science in Biology Berrien Springs, MI Aug 2005 Andrews University Mar 1997 – Bachelor of Science in Biology Seoul, South Korea Feb 2001 Sahmyook University (Korean Adventist University) (Summa Cum Laude, Valedictorian) Employment Experience September 2015 – Assistant Professor – Teach X-ray physics, Palmer College of Present special imaging, X-ray positioning and soft tissue Chiropractic, radiology covering abdomen and chest radiology, Port Orange, FL and small group learning sessions. • Course Director: X-ray Physics • Course Director: X-ray Positioning • Course Director: Soft Tissue Radiology • Dourse Director: Special Imaging • Course Contributor: Cardiopulmonary Integrative diagnosis • Course Contributor: X-ray Positioning Page 1 of 9 Dr. Munyeong Choi Chiropractic Radiologist September 2013 – Adjunct Faculty – Teach anatomy and College of DuPage, May 2015 physiology lecture and lab for pre-physical Glen Ellyn, IL therapy, occupational therapy, and nursing students. Jan 2013 – Present Director of Munyeong Choi Diagnostic Imaging Port Orange, FL Consultation – Interpret musculoskeletal diagnostic images including but not limited to plain radiographs and MR studies for health care providers including chiropractic physicians and medical doctors and patients. -

Chiropractic “Name Techniques”: a Review of the Literature
0008-3194/2001/86–99/$2.00/©JCCA 2001 Name techniques Chiropractic “Name Techniques”: a review of the literature Brian J. Gleberzon, DC* In a previous article, the author discussed current trends Dans un article précédent, l’auteur discutait des in utilization rates of chiropractic “Name Techniques” tendances actuelles dans les taux d’utilisation des in Canada, and provided recommendations for their « techniques de nom » chiropratiques au Canada et inclusion into the curriculum at the Canadian Memorial fournissait des recommandations pour leur inclusion Chiropractic College. In this article, a review of the au programme du Canadian Memorial Chiropractic literature on “Name Techniques” was conducted, with College. Cet article fournissait un examen qualitatif interpretation and synthesis by the author. One hundred de la littérature sur les « techniques de nom », avec and eleven articles were found. These were: technique interprétation et synthèse par l’auteur. 111 articles ont discussions (N = 39), case studies (N = 25), case series été étudiés. Il s’agit de : discussions des techniques (N = 5), experimental studies (N = 25) and clinical trials (N = 39), exposés de cas (N = 25), série de cas (N = 5), (N = 17). The literature suggested that prone leg length études expérimentales (N = 25) et études cliniques testing and some x-ray mensurations may have (N = 17). La littérature suggérait que les tests de acceptable inter and intra-rater reliability. In addition, longueur de jambe en pronation et certaines there are several case studies that reported significant mensurations radiographiques pouvaient avoir une clinical benefits by patients receiving Activator, fiabilité inter et intra-évaluateur. En outre, plusieurs Alexander, and Upper Cervical treatments. -

The Epidemiology of Work-Related Musculoskeletal Injuries Among Chiropractors in the Ethekwini Municipality
The epidemiology of work-related musculoskeletal injuries among chiropractors in the eThekwini municipality A dissertation submitted in partial compliance with the requirements for a Master’s Degree in Technology, in the Department of Chiropractic and Somatology at the Durban University of Technology. By Almay Lamprecht 2017 I, Almay Lamprecht, do declare that this dissertation is representative of my own work in both conception and execution (except where acknowledgements indicate to the contrary). ______________________ __________________ Almay Lamprecht Date Approved for Final Submission: ______________________ __________________ Dr. K. Padayachy Date M.Tech: Chiropractic (SA), PhD Anatomy I DEDICATION I dedicate this work To my Heavenly Father who has given me the means to complete this degree. And To my parents who have given me their unwavering support throughout this entire process. II ACKNOWLEDGEMENTS To my parents, Jaco and Tina Lamprecht, thank you for giving me the opportunity to fulfil my dream and encouraging me with your love and support along the way. My sister, Simoné, thank you for your love, support and encouragement Sussie. Erlou, my fiancé, no words can describe what your support throughout this entire process meant to me. Thank you for all your love and encouragement. To Johmari, Carissa, Tylah, Mike and Kyle- thank you for the unlikely friendship that started six years ago. No words can describe the incredible journey we've had. My supervisor, Dr Keseri Padayachy, thank you for your input and assistance. Dr Graeme Harpham, thank you for helping out in the initial stages. To Deepak Singh, for your assistance with the statistical analysis of this study. -
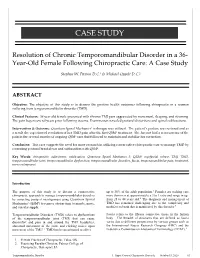
TMJ Dysfunction
CASE STUDY Resolution of Chronic Temporomandibular Disorder in a 36- Year-Old Female Following Chiropractic Care: A Case Study Stephen W. Paxton D.C.1 & Michael Oppelt D.C.2 ABSTRACT Objective: The objective of this study is to discuss the positive health outcomes following chiropractic in a woman suffering from temporomandibular disorder (TMD). Clinical Features: 36 year old female presented with chronic TMJ pain aggravated by movement, sleeping, and straining. The pain began several years prior following trauma. Examination revealed postural distortions and spinal subluxations. Intervention & Outcome: Quantum Spinal Mechanics3 technique was utilized. The patient’s posture was restored and as a result she experienced resolution of her TMD pain after the first QSM3 treatment. She has not had a reoccurrence of the pain in the several months of ongoing QSM3 care that followed to maintain and stabilize her correction. Conclusion: This case suggests the need for more research in utilizing conservative chiropractic care to manage TMD by correcting postural breakdown and subluxation with QSM3. Key Words: chiropractic, adjustment, subluxation, Quantum Spinal Mechanics 3, QSM3, myofascial release, TMJ, TMD, temporomandibular joint, temporomandibular dysfunction, temporomandibular disorders, fascia, temporomandibular pain, treatment, nerve entrapment Introduction The purpose of this study is to discuss a conservative up to 30% of the adult population.3 Females are seeking care chiropractic approach to manage temporomandibular disorders more than men at approximately a 3 to 1 ratio and range in age by correcting postural misalignment using Quantum Spinal from 25 to 44 years old.4 The diagnosis and management of Mechanics3 (QSM3) to remove obstructions to muscle, nerve, TMD has remained challenging due to the complexity and and vascular supply. -

Neurological Change According to Resting Pulse Rate Following Chiropractic Care: a Case Series J Hart
The Internet Journal of Neurology ISPUB.COM Volume 19 Number 1 Neurological Change According To Resting Pulse Rate Following Chiropractic Care: A Case Series J Hart Citation J Hart. Neurological Change According To Resting Pulse Rate Following Chiropractic Care: A Case Series. The Internet Journal of Neurology. 2016 Volume 19 Number 1. DOI: 10.5580/IJN.41669 Abstract Introduction: This report describes a method of determining what type of general neurological changes have occurred, if any, following chiropractic care according to resting pulse rate (RPR) in individual patients. The method may be of interest to chiropractors and other clinicians who have a neurological focus in their practices. Methods: Multiple pre-adjustment RPR measurements were compared to multiple post-adjustment RPR measurements on an individual patient basis using t test and effect size statistics. Results: In two of the five patients, a statistically significant decrease (improvement) was observed in mean post-adjustment RPR compared to mean pre-adjustment RPR (p < 0.02), with large effect sizes (of approximately 1.2). In the other three patients, mean post RPR was essentially unchanged according to their t test p-values. Conclusion: According to the method used in this study, general neurological function improved in two of the five patients, evidenced by the statistically significant decrease in RPR, along with large effect sizes. Further study using other chiropractic techniques, and with other patients is indicated. INTRODUCTION Another measure that is potentially useful in neurologically- Chiropractic care focused practices, e.g., in subluxation-centered chiropractic, is resting heart rate, also known as resting pulse rate when In subluxation-centered chiropractic care, the objective is to obtained by manual palpation of a peripheral artery.