Board of Commissioners Meeting March 5, 2018 4:00 Pm
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Career Academy Application
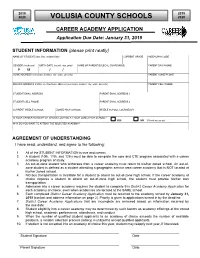
2019 2019 2020 VOLUSIA COUNTY SCHOOLS 2020 CAREER ACADEMY APPLICATION Application Due Date: January 31, 2019 STUDENT INFORMATION (please print neatly) NAME OF STUDENT (last, first, middle initial) CURRENT GRADE AIDE/ALPHA CODE GENDER (circle one) BIRTH DATE (month, day, year) NAME OF PARENT(S)/LEGAL GUARDIAN(S) PARENT DAY PHONE F M / / HOME ADDRESS (street/apt. number, city, state, zip code) PARENT HOME PHONE MAILING ADDRESS (if different than home address) (street/apt. number, city, state, zip code) PARENT CELL PHONE STUDENT EMAIL ADDRESS PARENT EMAIL ADDRESS 1 STUDENT CELL PHONE PARENT EMAIL ADDRESS 2 CURRENT MIDDLE SCHOOL ZONED HIGH SCHOOL MIDDLE SCHOOL COUNSELOR IS YOUR CAREER ACADEMY OF CHOICE LOCATED AT YOUR ZONED HIGH SCHOOL? YES NO (Check yes or no) WHY DO YOU WANT TO ATTEND THE SELECTED ACADEMY? AGREEMENT OF UNDERSTANDING I have read, understand, and agree to the following: 1. All of the STUDENT INFORMATION is true and correct. 2. A student (10th, 11th, and 12th) must be able to complete the core and CTE program associated with a career academy program of study. 3. An out-of-zone student who withdraws from a career academy must return to his/her zoned school. An out-of- zone student is defined as a student attending a geographic service area career academy that is NOT located at his/her zoned school. 4. NO bus transportation is available for a student to attend an out-of-zone high school. If the career academy of choice requires a student to attend an out-of-zone high school, the student must provide his/her own transportation. -

50 Years of NASCAR Captures All That Has Made Bill France’S Dream Into a Firm, Big-Money Reality
< mill NASCAR OF NASCAR ■ TP'S FAST, ITS FURIOUS, IT'S SPINE- I tingling, jump-out-of-youn-seat action, a sport created by a fan for the fans, it’s all part of the American dream. Conceived in a hotel room in Daytona, Florida, in 1948, NASCAR is now America’s fastest-growing sport and is fast becoming one of America’s most-watched sports. As crowds flock to see state-of-the-art, 700-horsepower cars powering their way around high-banked ovals, outmaneuvering, outpacing and outthinking each other, NASCAR has passed the half-century mark. 50 Years of NASCAR captures all that has made Bill France’s dream into a firm, big-money reality. It traces the history and the development of the sport through the faces behind the scene who have made the sport such a success and the personalities behind the helmets—the stars that the crowds flock to see. There is also a comprehensive statistics section featuring the results of the Winston Cup series and the all-time leaders in NASCAR’S driving history plus a chronology capturing the highlights of the sport. Packed throughout with dramatic color illustrations, each page is an action-packed celebration of all that has made the sport what it is today. Whether you are a die-hard fan or just an armchair follower of the sport, 50 Years of NASCAR is a must-have addition to the bookshelf of anyone with an interest in the sport. $29.95 USA/ $44.95 CAN THIS IS A CARLTON BOOK ISBN 1 85868 874 4 Copyright © Carlton Books Limited 1998 Project Editor: Chris Hawkes First published 1998 Project Art Editor: Zoe Maggs Reprinted with corrections 1999, 2000 Picture Research: Catherine Costelloe 10 9876 5 4321 Production: Sarah Corteel Design: Graham Curd, Steve Wilson All rights reserved. -

Of 217 11:45:20AM Club Information Report CUS9503 09/01/2021
Run Date: 09/22/2021 Key Club CUS9503 Run Time: 11:53:54AM Club Information Report Page 1 of 217 Class: KCCLUB Districts from H01 to H99 Admin. Start Date 10/01/2020 to 09/30/2021 Club Name State Club ID Sts Club Advisor Pd Date Mbr Cnt Pd Amount Kiwanis Sponsor Club ID Div H01 - Alabama Abbeville Christian Academy AL H90124 Debbie Barnes 12/05/2020 25 175.00 Abbeville K04677 K0106 Abbeville High School AL H87789 Valerie Roberson 07/06/2021 9 63.00 Abbeville K04677 K0106 Addison High School AL H92277 Mrs Brook Beam 02/10/2021 19 133.00 Cullman K00468 K0102 Alabama Christian Academy AL H89446 I Page Clayton 0 Montgomery K00174 K0108 Alabama School Of Mathematics And S AL H88720 Derek V Barry 11/20/2020 31 217.00 Azalea City, Mobile K10440 K0107 Alexandria High School AL H89049 Teralyn Foster 02/12/2021 29 203.00 Anniston K00277 K0104 American Christian Academy AL H94160 I 0 Andalusia High School AL H80592 I Daniel Bulger 0 Andalusia K03084 K0106 Anniston High School AL H92151 I 0 Ashford High School AL H83507 I LuAnn Whitten 0 Dothan K00306 K0106 Auburn High School AL H81645 Audra Welch 02/01/2021 54 378.00 Auburn K01720 K0105 Austin High School AL H90675 Dawn Wimberley 01/26/2021 36 252.00 Decatur K00230 K0101 B.B. Comer Memorial School AL H89769 Gavin McCartney 02/18/2021 18 126.00 Sylacauga K04178 K0104 Baker High School AL H86128 0 Mobile K00139 K0107 Baldwin County High School AL H80951 Sandra Stacey 11/02/2020 34 238.00 Bayside Academy AL H92084 Rochelle Tripp 11/01/2020 67 469.00 Daphne-Spanish Fort K13360 K0107 Beauregard High School AL H91788 I C Scott Fleming 0 Opelika K00241 K0105 Benjamin Russell High School AL H80742 I Mandi Burr 0 Alexander City K02901 K0104 Bessemer Academy AL H90624 I 0 Bob Jones High School AL H86997 I Shari Windsor 0 Booker T. -

Student First & Last School Grade Middle/High Jared Richard Kolb
Student First & Last School Grade Middle/High Jared Richard Kolb Atlantic High School 9 High Shanice Gilpin Atlantic High School 11 High Jahwain Marquel Bush-Adams Atlantic High School 12 High Terry Lorenzo Edwards, III DeLand High School 9 High Josh Strickland Toth DeLand High School 9 High Austin Edkins DeLand High School 10 High Brandon Roselle DeLand High School 10 High Alex Clark-Roberts DeLand High School 11 High Veronica Camacho DeLand High School 12 High Jordan Alvarado Deltona High School 9 High Daniel Moss Deltona High School 10 High Elizabeth Talamo Deltona High School 11 High Kaliha Griffin Deltona High School 12 High Americus Whaley Legacy Scholars Academy 9 High Verica Thomas Legacy Scholars Academy 10 High Christina Pennay Legacy Scholars Academy 11 High Christian Leavitt Legacy Scholars Academy 12 High D’Shawn McLaury Mainland High School 9 High Dana Rossi Mainland High School 10 High Arieanna Goodin Mainland High School 11 High Cataurius Mason Mainland High School 12 High Kyler Kiger New Smyrna Beach High School 9 High Cianna Perrine New Smyrna Beach High School 10 High Taylor Oliver New Smyrna Beach High School 11 High Sean Patrick New Smyrna Beach High School 12 High Nikki Eland Pine Ridge High School 9 High Joshua Colon Pine Ridge High School 10 High Celaya Sweeney Pine Ridge High School 11 High Anthony Rodriguez Pine Ridge High School 12 High Amelia Moore Seabreeze High School 9 High Thomas Ceku Seabreeze High School 10 High Twishyriah Glenn Seabreeze High School 11 High Christen Helem Seabreeze High School 12 High -
Ormond Beach Daytona Beach Holly Hill Land Lines
DAN’S INSIDE ORMOND BEACH DAYTONA BEACH HOLLY HILL LAND LINES Dean of the Halifax River remembered Page A3 Ormond Beach Dental Group Vol. 9, No. 16 Your Local News and Information Source • www.HometownNewsOL.com Friday, May 9, 2014 Need Community Walmart looks at West Volusia Dentures? notes Free Consultations & Second Opinions Crowns Closure of John while East Volusia waits $675 • Denture Full Denture Reline $175 $495 Anderson Drive By Erika Webb website. Now Owned & Operated By moves to Royal Palm [email protected] WRS is navigating the process to develop land at the corner of Saxon and Sterling Silver Kerri Graham D.M.D. A Walmart Neighborhood Market could boulevards in Deltona for a Walmart Neigh- See ad in this section for more information John Anderson Drive at replace the DeLand Flea Market at 921 S. Wood- borhood Market. Best Dentist Royal Palm Avenue will be land Blvd. and there is talk of more to follow. George Demattio, who owns The Furniture 802 Sterthaus 386-944-5002Drive, Suite A • Ormond Beach, FL closed starting at 8 a.m. (Across the street from the Imploded Florida Hospital) It’s one of three possible Walmarts in West Shoppe at 911 S. Woodland Blvd., said WRS 784192 Monday, May 12, to 5 p.m. Volusia County, while nothing is happening with first approached him over a year ago to Friday, May 16. two sites in East Volusia that Walmart already negotiate a deal to buy his land. Drivers should use desig- Prop- owns. “They wanted to buy all the way to the cor- nated detours. -

Charter Schools
Revised: June 21, 2021 REF: VCSlist Volusia County Schools Atlantic High School (9-12) - 1250 Reed Canal Road, Port Orange, FL 32129 Principal: Mr. Stephen Hinson Telephone: (386) 322-6100 Beachside Elementary School (6-8) – 100 Osceola Avenue, Ormond Beach, FL 32176 Principal: Ms. Lynn Bruner Telephone: (386) 258-4669 Blue Lake Elementary School (K-5) - 282 North Blue Lake Avenue, DeLand, FL 32724 Principal: Ms. Holly Bailey Telephone: (386) 822-4070 Campbell Middle School (6-8) - 625 South Keech Street, Daytona Beach, FL 32114 Principal: Ms. Cindy Townsend Telephone: (386) 258-4661 Champion Elementary School (K-5) – 921 Tournament Drive, Daytona Beach, FL 32124 Principal: Ms. Angela Polite Telephone: (386) 258-4664 Chisholm Elementary School (K-5) - 557 Ronnoc Lane, New Smyrna Beach, FL 32168 Principal: Ms. Melissa Marple Telephone: (386) 424-2540 Citrus Grove Elementary School (K-5) – 729 Hazen Road, DeLand, Fl 32720 Principal: Ms. Jennifer Williams Telephone: (386) 626-0053 Coronado Beach Elementary School (K-5) - 3550 Michigan Avenue, New Smyrna Beach, FL 32169 Principal: Ms. Tracy Buckner Telephone: (386) 424-2525 Creekside Middle School (6-8) - 6801 Airport Road, Port Orange, FL 32128 Principal: Mr. John Cash Telephone: (386) 322-6155 Cypress Creek Elementary School (K-5) - 6100 S. Williamson Boulevard, Port Orange, FL 32128 Principal: Mr. Eric Paul Telephone: (386) 322-6101 DeBary Elementary School (K-5) - 88 West Highbanks Road, DeBary, FL 32713 Principal: Ms. Leslie Frazee Telephone: (386) 575-4230 DeLand High School (9-12) - 800 North Hill Avenue, DeLand, FL 32724 Principal: Dr. Melissa Carr Telephone: (386) 822-6909 DeLand Middle School (6-8) - 1400 South Aquarius Avenue, DeLand, FL 32724 Principal: Mr. -

Charter Schools
Revised: August 25, 2021 REF: VCSlist Volusia County Schools Atlantic High School (9-12) - 1250 Reed Canal Road, Port Orange, FL 32129 Principal: Mr. Jason Watson Telephone: (386) 322-6100 Beachside Elementary School (6-8) – 100 Osceola Avenue, Ormond Beach, FL 32176 Principal: Ms. Lynn Bruner Telephone: (386) 258-4669 Blue Lake Elementary School (K-5) - 282 North Blue Lake Avenue, DeLand, FL 32724 Principal: Ms. Holly Bailey Telephone: (386) 822-4070 Campbell Middle School (6-8) - 625 South Keech Street, Daytona Beach, FL 32114 Principal: Ms. Kimberly Matthews Telephone: (386) 258-4661 Champion Elementary School (K-5) – 921 Tournament Drive, Daytona Beach, FL 32124 Principal: Ms. Angela Polite Telephone: (386) 258-4664 Chisholm Elementary School (K-5) - 557 Ronnoc Lane, New Smyrna Beach, FL 32168 Principal: Ms. Melissa Marple Telephone: (386) 424-2540 Citrus Grove Elementary School (K-5) – 729 Hazen Road, DeLand, Fl 32720 Principal: Ms. Jennifer Williams Telephone: (386) 626-0053 Coronado Beach Elementary School (K-5) - 3550 Michigan Avenue, New Smyrna Beach, FL 32169 Principal: TBA Telephone: (386) 424-2525 Creekside Middle School (6-8) - 6801 Airport Road, Port Orange, FL 32128 Principal: Mr. John Cash Telephone: (386) 322-6155 Cypress Creek Elementary School (K-5) - 6100 S. Williamson Boulevard, Port Orange, FL 32128 Principal: Ms. Tracy Buckner Telephone: (386) 322-6101 DeBary Elementary School (K-5) - 88 West Highbanks Road, DeBary, FL 32713 Principal: Ms. Leslie Frazee Telephone: (386) 575-4230 DeLand High School (9-12) - 800 North Hill Avenue, DeLand, FL 32724 Principal: Dr. Melissa Carr Telephone: (386) 822-6909 DeLand Middle School (6-8) - 1400 South Aquarius Avenue, DeLand, FL 32724 Principal: Mr. -

Volusia County All-State Musicians
Volusia County Schools All-State Musicians 2013-2014 School Student Name Teacher Name Performing Ensemble Cypress Creek Elementary School Phebe Rich Julia Hood/Mary Ada Kidd Elementary Chorus George Marks Elementary School Sarah Sutcliffe Caroline Hood Elementary Chorus George Marks Elementary School Madison Grant Caroline Hood Elementary Chorus George Marks Elementary School Kyla Eugenio Caroline Hood Elementary Chorus Burns Science Tech Charter Elizabeth Beard Shawna Batchelor Middle School Honors Orchestra Campbell Middle School Breanna Edwards Earnest Echols Middle School Treble Chorus Creekside Middle School Rhea Allani Amanda El Shemi Middle School Treble Chorus Creekside Middle School Ashley Benton Amanda El Shemi Middle School Treble Chorus Creekside Middle School Lavanya Durai Amanda El Shemi Middle School Mixed Chorus Creekside Middle School Autumn Rundall Amanda El Shemi Middle School Mixed Chorus Creekside Middle School Maya Henebury Amanda El Shemi Middle School Mixed Chorus Creekside Middle School Emma Murray Amanda El Shemi Middle School Mixed Chorus Creekside Middle School Matthew Turner Brittnie Curley Middle School Concert Band Creekside Middle School Ethan Avila Brittnie Curley Middle School Concert Band Heritage Middle School Rowyn Willis Elizabeth Coldiron Middle School Treble Chorus Heritage Middle School Lillian Grusz Elizabeth Coldiron Middle School Mixed Chorus Hinson Middle School Camryn Biza Kathy Finn Middle School Honors Orchestra New Smyrna Beach Middle School Gerrit Bosma Jonathan Brodie Middle School Concert -

Volusia County Schools Directory of Directions
Volusia County Schools Directory of Directions Prepared by Community Information Services Adjunct Classroom Enterprise Elementary ........................... 13 Bicentennial Youth Park .........................1 Forest Lake Elementary ........................ 14 Schools Freedom Elementary ............................ 14 Atlantic High ...........................................1 Friendship Elementary .......................... 15 Blue Lake Elementary ...........................2 Galaxy Middle ....................................... 15 Boston Avenue Charter…………………..2 Heritage Middle ..................................... 16 Burns Science & Technology Charter .....3 Highbanks Learning Center …………...16 Campbell Middle ....................................3 Hinson, Sr., David C. Middle ................. 17 Champion Elementary ...........................4 Holly Hill School .................................... 17 Chiles Academy .....................................4 Horizon Elementary ............................... 18 Chisholm Elementary ...........................5 Indian River Elementary ........................ 18 Citrus Grove Elementary ........................5 Ivy Hawn Charter …… .......................... 19 Coronado Beach Elementary .................6 Longstreet Elementary .......................... 19 Creekside Middle ...................................6 Mainland High ....................................... 20 Cypress Creek Elementary .....................7 DeBary Elementary ................................7 Manatee Cove Elementary ……………..20 -
Media Guide Cvrs.Indd 1 7/4/07 5:13:21 PM 47365-Fsu Media Guide Cvrs.Indd 2 7/4/07 5:13:27 PM 1
47365-FSu Media Guide cvrs.indd 1 7/4/07 5:13:21 PM 47365-FSu Media Guide cvrs.indd 2 7/4/07 5:13:27 PM 1 47365-FSU MG Pg 001-026 Intro 1 7/8/07, 2:41 PM 2 47365-FSU MG Pg 001-026 Intro 2 7/4/07, 5:31 PM 3 47365-FSU MG Pg 001-026 Intro 3 7/4/07, 5:32 PM 4 47365-FSU MG Pg 001-026 Intro 4 7/4/07, 5:32 PM 5 47365-FSU MG Pg 001-026 Intro 5 7/4/07, 5:32 PM 6 47365-FSU MG Pg 001-026 Intro 6 7/4/07, 5:32 PM 7 47365-FSU MG Pg 001-026 Intro 7 7/4/07, 5:32 PM 8 47365-FSU MG Pg 001-026 Intro 8 7/9/07, 6:53 PM 9 47365-FSU MG Pg 001-026 Intro 9 7/4/07, 5:32 PM 10 47365-FSU MG Pg 001-026 Intro 10 7/4/07, 5:32 PM 11 47365-FSU MG Pg 001-026 Intro 11 7/4/07, 5:32 PM 12 47365-FSU MG Pg 001-026 Intro 12 7/9/07, 6:53 PM 13 47365-FSU MG Pg 001-026 Intro 13 7/4/07, 5:32 PM 14 47365-FSU MG Pg 001-026 Intro 14 7/4/07, 5:33 PM 15 47365-FSU MG Pg 001-026 Intro 15 7/4/07, 5:33 PM 16 47365-FSU MG Pg 001-026 Intro 16 7/4/07, 5:33 PM 17 47365-FSU MG Pg 001-026 Intro 17 7/4/07, 5:33 PM 18 47365-FSU MG Pg 001-026 Intro 18 7/4/07, 5:33 PM 19 47365-FSU MG Pg 001-026 Intro 19 7/4/07, 5:33 PM 20 47365-FSU MG Pg 001-026 Intro 20 7/4/07, 5:33 PM 21 47365-FSU MG Pg 001-026 Intro 21 7/4/07, 5:33 PM Bobby Bowden Field at Doak Campbell Stadium rom a maximum capacity of 15,000 The south endzone houses the in 1953 to a record crowd of 84,347 Florida State school of hospitality Fin 2005 against Miami, Doak S. -
DAYTONA BEACH ORMOND BEACH Volusi- A7 E by Troubles Their Can Forget Children E by Healthcare Educationpartner B-CU Getsbigdonationand Mr
DAN’S INSIDE ORMOND BEACH DAYTONA BEACH HOLLY HILL LAND LINES Area will be representing at Goodwood Ormond Beach DentalPage A3 Group Vol. 9, No. 22 Your Local News and Information Source • www.HometownNewsOL.com Friday, June 20, 2014 Need Community B-CU gets big donation and Dentures? notes Free Consultations & Second Opinions Crowns $675 • Denture ERAU professor to healthcare education partner Full Denture Reline $175 $495 discuss drones By Susan L. Wright executive director of Halifax Health Founda- Now Owned & Operated By [email protected]º tion and has a long history of community From domestic surveil- involvement and philanthropy. He’s also been Kerri Graham D.M.D. See ad in this section for more information lance to the battlefields of a trustee of the university for the past eight There was plenty to celebrate at Bethune- Best Dentist Afghanistan, drones have years. Cookman University June 12 as top executives 802 Sterthaus 386-944-5002Drive, Suite A • Ormond Beach, FL flown into controversy and from the school, Halifax Health and others gath- The second important announcement was (Across the street from the Imploded Florida Hospital) the public’s imagination. ered to announce a pair of major developments that Halifax Health’s CEO Jeff Feasal signed a 785332 Learn about these that will enhance the relationship of the school “memorandum of understanding,” basically an agreement, to work together on a variety unmanned aerial vehicles and hospital. col- during a free program at 3 The first was that Joe Petrock, one of the area’s of services and programs to provide educational opportunities for B-CU students who would lege and intern or p.m. -

High School Theatre Teachers
High School Theatre Teachers FIRST NAME LAST NAME SCHOOL ADDRESS CITY STATE ZIP Pamela Vallon-Jackson AGAWAM HIGH SCHOOL 760 Cooper St Agawam MA 01001 John Bechtold AMHERST PELHAM REGIONAL HIGH SCHOOL 21 Matoon St Amherst MA 01002 Susan Comstock BELCHERTOWN HIGH SCHOOL 142 Springfield Rd Belchertown MA 01007 Denise Freisberg CHICOPEE COMPREHENSIVE HIGH SCHOOL 617 Montgomery St Chicopee MA 01020 Rebecca Fennessey CHICOPEE COMPREHENSIVE HIGH SCHOOL 617 Montgomery St Chicopee MA 01020 Deborah Sali CHICOPEE HIGH SCHOOL 820 Front St Chicopee MA 01020 Amy Davis EASTHAMPTON HIGH SCHOOL 70 Williston Ave Easthampton MA 01027 Margaret Huba EAST LONGMEADOW HIGH SCHOOL 180 Maple St East Longmeadow MA 01028 Keith Boylan GATEWAY REGIONAL HIGH SCHOOL 12 Littleville Rd Huntington MA 01050 Eric Johnson LUDLOW HIGH SCHOOL 500 Chapin St Ludlow MA 01056 Stephen Eldredge NORTHAMPTON HIGH SCHOOL 380 Elm St Northampton MA 01060 Ann Blake PATHFINDER REGIONAL VO-TECH SCHOOL 240 Sykes St Palmer MA 01069 Blaisdell SOUTH HADLEY HIGH SCHOOL 153 Newton St South Hadley MA 01075 Sean Gillane WEST SPRINGFIELD HIGH SCHOOL 425 Piper Rd West Springfield MA 01089 Rachel Buhner WEST SPRINGFIELD HIGH SCHOOL 425 Piper Rd West Springfield MA 01089 Jessica Passetto TACONIC HIGH SCHOOL 96 Valentine Rd Pittsfield MA 01201 Jolyn Unruh MONUMENT MOUNTAIN REGIONAL HIGH SCHOOL 600 Stockbridge Rd Great Barrington MA 01230 Kathy Caton DRURY HIGH SCHOOL 1130 S Church St North Adams MA 01247 Jesse Howard BERKSHIRE SCHOOL 245 N Undermountain Rd Sheffield MA 01257 Robinson ATHOL HIGH SCHOOL