Borders Director of Public Health Report 2015 Contents Borders Director of Public Health Report 2015
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix-2019-89-Child-Poverty-Action-Plan.Pdf
Appendix-2019-89 Borders NHS Board Meeting Date: 27 June 2019 Approved by: Tim Patterson, Director of Public Health Author: Allyson McCollam, Associate Director of Public Health CHILD POVERTY ACTION PLAN Purpose of Report: The purpose of this report is to update the NHS Board on the development of the Scottish Borders Child Poverty Action Plan in response to the Child Poverty (Scotland) Act 2017. Recommendations: The Board is asked to note and approve Child Poverty Action Plan. Approval Pathways: This report has been prepared in consultation with the key members of the CPP Reducing Inequalities Delivery Group. This Plan has been approved by the Community Planning Partnership on 13th June 2019 for submission to the Scottish Government in June 2019. Executive Summary: This is the first such annual Local Action Plan report for Scottish Borders. It describes the challenges faced in measuring child poverty locally, how this plan links to existing activity, what we have delivered in the reporting period 2018 /19 and what we are committed to delivering over the 2019/20 financial year. This will form the basis for identifying areas that we would like to develop further in the future. It is recognised that partnership is key to the achievement of the outcomes we want for our children, young people and families in Scottish Borders, and this will mean working collaboratively to tackle the drivers of child poverty: income from employment, income from social security and cost of living. The areas for action are as follows: Employability Housing Customer services including welfare benefits advice Education Health and wellbeing The health and wellbeing workstream includes the NHS duty to provide financial inclusion pathways for families with children from the antenatal stage and beyond. -

Download [262.49
SCOTTISH GOVERNMENT Issued on behalf of The Local Government Boundary Commission for Scotland Not for Publication, Broadcast or use on Club Tapes before 0001 Hours on 26 May 2016 Recommendations for councillor numbers and wards submitted to Scottish Ministers The Local Government Boundary Commission for Scotland has submitted its recommendations on councillor numbers and wards for each of Scotland's 32 council areas to Scottish Ministers. These recommendations arise from the 5th Reviews of Local Government Electoral Arrangements which began in February 2014. The recommendations provide for 351 wards and 1219 councillors across Scotland, an overall decrease of 2 wards and 4 councillors relative to existing arrangements. Under the recommendations, representation of the electorate within council areas will be more evenly shared between councillors and across Scotland there will be greater equity in electoral representation. Ronnie Hinds, Chair of the Commission, said: "Today we have submitted to Scottish Ministers our recommendations for electoral arrangements which we believe are in the interests of effective and convenient local government across Scotland. These recommendations set out the number of councillors for each council area and the boundaries of the wards they will represent. We are grateful to councils and to the public who responded to our consultations over the last two years. Their input has been invaluable in shaping our proposals and while we must take account of our obligations under the legislation and consider the interests of the whole council area, we have been able to take on board many of the views expressed. The legislation which governs our reviews places equality of representation at the heart of what we do and we have delivered a set of recommendations that significantly improves electoral parity across Scotland and so provides for fairer local democracy and more effective local government ." 1 A summary of the recommendations for each council area is contained in the appendix to this release. -

Local Government Electors on the Electoral Register, by Council Area and Electoral Ward, 2007 to 2010
Table 6: Local Government electors on the Electoral Register, by Council area and Electoral Ward, 2007 to 2010 No of 2007 2008 2009 2010 Ward elected Total Total Total Total Council area Code Electoral Ward members Electorate Attainers Electorate Attainers Electorate Attainers Electorate Attainers Aberdeen City 155,666 1,693 156,732 1,577 156,597 1,717 158,087 1,650 0111 Airyhall/ Broomhill/ Garthdee 3 11,842 107 11,729 94 11,534 91 11,631 102 0102 Bridge of Don 4 14,411 168 14,221 162 14,138 195 14,165 190 0101 Dyce/ Bucksburn/ Danestone 4 14,008 134 13,851 130 13,786 129 13,931 141 0108 George St/ Harbour 3 11,154 138 12,081 137 12,420 110 12,396 119 0110 Hazlehead/ Ashley/ Queens Cross 4 13,493 165 13,279 123 13,333 168 13,512 131 0105 Hilton/ Stockethill 3 10,273 78 10,294 49 10,247 67 10,477 89 0113 Kincorth/ Loirston 3 12,043 135 11,949 117 11,848 151 11,926 141 0103 Kingswells/ Sheddocksley 3 10,493 102 10,385 98 10,408 109 10,395 79 0109 Lower Deeside 3 11,019 190 11,109 188 11,140 187 11,324 161 0107 Midstocket/ Rosemount 3 10,514 83 10,755 90 10,991 90 10,949 71 0104 Northfield 3 11,450 110 11,311 119 11,133 143 11,358 149 0106 Tillydrone/ Seaton/ Old Aberdeen 3 11,150 172 12,161 185 12,278 192 12,280 200 0112 Torry/ Ferryhill 4 13,816 111 13,607 85 13,341 85 13,743 77 Aberdeenshire 182,576 2,483 182,790 2,487 182,953 2,401 185,454 2,669 0215 Aboyne, Upper Deeside and Donside 3 8,448 110 8,458 124 8,376 112 8,489 126 0216 Banchory and Mid Deeside 3 8,030 135 8,018 142 8,063 131 8,152 142 0201 Banff and District 3 8,798 97 8,661 -

Council Results 2007
Aberdeen 2007 Elected Councillors Ward 1: Dyce, Bucksburn & Danestone Ron Clark (SLD) Barney Crockett (Lab) Mark McDonald (SNP) George Penny (SLD) Ward 2: Bridge of Don Muriel Jaffrey (SNP) Gordon Leslie (SLD) John Reynolds (SLD) Willie Young (Lab) Ward 3 Kingswells & Sheddocksley Len Ironside (Lab) Peter Stephen (SLD) Wendy Stuart (SNP) Ward 4 Northfield Jackie Dunbar (SNP) Gordon Graham (Lab) Kevin Stewart (SNP) Ward 5 Hilton / Stockethill George Adam (Lab) Neil Fletcher (SLD) Kirsty West (SNP) Ward 6 Tillydrone, Seatonand Old Aberdeen Norman Collie (Lab) Jim Noble (SNP) Richard Robertson (SLD) Ward 7 Midstocket & Rosemount BIll Cormie (SNP) Jenny Laing (Lab) John Porter (Con) Ward 8 George St & Harbour Andrew May (SNP) Jim Hunter (Lab) John Stewart (SLD) Ward 9 Lower Deeside Marie Boulton (Ind) Aileen Malone (SLD) Alan Milne (Con) Ward 10 Hazelhead, Ashley and Queens Cross Jim Farquharson (Con) Martin Grieg (SLD) Jennifer Stewart (SLD) John West (SNP) Ward 11 Airyhall, Broomhill and Garthdee Scott Cassie (SLD) Jill Wisely (Con) Ian Yuill (SLD) Ward 12 Torry & Ferryhill Yvonne Allan (Lab) Irene Cormack (SLD) Alan Donnelly (Con) Jim Kiddie (SNP) Ward 13 Kincorth & Loirston Neil Cooney (Lab) Katherine Dean (SLD) Callum McCaig (SNP) ELECTORATE: 160,500 2003 RESULT: SLD 20: Lab 14: SNP 6: Con 3 Aberdeenshire 2007 Elected Councillors Ward 1 Banff and District John B Cox (Ind) Ian Winton Gray (SNP) Jack Mair (SLD) Ward 2 Troup Mitchell Burnett (SNP) John Duncan (Con) Sydney Mair (Ind) Ward 3 Fraserburgh and District Andy Ritchie (SNP) Ian -

Leaderdale and Melrose – Overview of Population, Deprivation, Unemployment and Schools
Leaderdale and Melrose – Overview of Population, Deprivation, Unemployment and Schools Leaderdale and Melrose ward has a population of 10,779. The main settlements (population of 500 or more) in the ward are Earlston, Lauder, Melrose and Tweedbank. The 2015 population estimates were produced by the National Records of Scotland. The percent of children in low income families is produced by HMRC. Children Working Age Pension Age Total Population Datazone Name (2011) DZ2011 Code Population 2015 Population 2015 Population 2015 2015 Blainslie and Legerwood S01012297 113 352 129 594 Earlston - East S01012270 165 452 143 760 Earlston - West S01012269 153 531 284 968 Earlston and Melrose Landward S01012268 100 413 114 627 Gattonside - Darnick - Chiefswood S01012289 118 472 285 875 Lauder - North S01012298 163 494 203 860 Lauder - South S01012296 265 571 107 943 Melrose - Dingleton Hill S01012291 247 683 158 1,088 Melrose - High Street S01012292 134 371 268 773 Melrose - Newstead S01012290 90 342 165 597 Oxton and Area S01012299 108 438 106 652 Tweedbank - East S01012295 185 520 70 775 Tweedbank - North S01012294 126 541 143 810 Tweedbank - West S01012293 79 259 119 457 Leaderdale and Melrose Total 2,046 6,439 2,294 10,779 Scottish Borders 18,975 68,307 26,748 114,030 Scotland 912,262 3,477,740 982,998 5,373,000 Earlston 318 983 427 1,728 Lauder 428 1,065 310 1,803 Melrose 471 1,396 591 2,458 Tweedbank 390 1,320 332 2,042 % Children % Working Age % Pension Age % Children in Low Datazone Name (2011) Population 2015 Population 2015 Population 2015 -
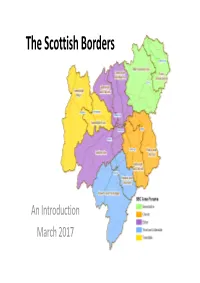
The Scottish Borders
The Scottish Borders An Introduction March 2017 2015 Population Total % % Working % Pension Area Forum / Ward Children Working Age Pension Age Population Children Age Age Berwickshire 3,332 12,268 5,227 20,827 16% 59% 25% East Berwickshire 1,745 6,243 2,603 10,591 16% 59% 25% Mid Berwickshire 1,587 6,025 2,624 10,236 16% 59% 26% Cheviot 2,987 11,273 5,254 19,514 15% 58% 27% Jedburgh and District 1,419 5,384 2,394 9,197 15% 59% 26% Kelso and District 1,568 5,889 2,860 10,317 15% 57% 28% Eildon 5,968 21,718 7,349 35,035 17% 62% 21% Galashiels and District 2,419 9,555 2,658 14,632 17% 65% 18% Leaderdale and 2,046 6,439 2,294 10,779 19% 60% 21% Melrose Selkirkshire 1,503 5,724 2,397 9,624 16% 59% 25% Teviot and Liddesdale 2,824 10,566 4,416 17,806 16% 59% 25% Hawick and Denholm 1,665 5,503 2,117 9,285 18% 59% 23% Hawick and Hermitage 1,159 5,063 2,299 8,521 14% 59% 27% Tweeddale 3,864 12,482 4,502 20,848 19% 60% 22% Tweeddale East 2,107 6,343 2,355 10,805 20% 59% 22% Tweeddale West 1,757 6,139 2,147 10,043 17% 61% 21% Grand Total 18,975 68,307 26,748 114,030 17% 60% 23% % % Working Pension Total % Children Working Pension Age Age Population Children Data Zone Name Age Age Bonchester Bridge and Chesters Area 83 421 233 737 11.3% 57.1% 31.6% Denholm 87 349 205 641 13.6% 54.4% 32.0% Hawick - Burnfoot - Central 220 447 98 765 28.8% 58.4% 12.8% Hawick - Burnfoot - North 275 516 63 854 32.2% 60.4% 7.4% Hawick - Burnfoot - South East 152 438 153 743 20.5% 59.0% 20.6% Hawick - Burnfoot - West 138 373 106 617 22.4% 60.5% 17.2% Hawick Central - Drumlanrig -

Scottish Local Election
Local authority elections in Scotland Report 3 May 2007 and Analysis The illustration on the cover of this report represents the town hall in Lerwick, Shetland, a building whose imposing features reflect the important role of local councils and local democracy. Its foundations were laid in 1884, the year that the Electoral Reform Society was established. Local authority elections in Scotland Report and 3 May 2007 Analysis Local authority elections in Scotland 3 May 2007 5 Contents Acknowledgements 7 Introduction 9 Summary 11 17 Part 1: What happened in the elections? Chapter 1: The results of 3 May 2007 17 Chapter 2: The political parties and the local elections 29 Chapter 3: Candidate strategy in multi-member wards 51 Chapter 4: Representation of women, young people and minorities 57 65 Part 2: The voters’ experience Chapter 5: More choice for voters 65 Chapter 6: Transferable voting 69 Chapter 7: Did people record valid votes? 83 91 Part 3: Election issues Chapter 8: Ballot design 91 Chapter 9: Multi-member wards 97 107 Part 4: Looking ahead Chapter 10: Looking forward 107 111 Appendix Scotland’s 32 new councils 111 Local authority elections in Scotland 3 May 2007 7 Acknowledgements and Dedication A project of this size is never a one-person job and I would like to thank Ken Ritchie, Amy Rodger and Martin Steven in particular for their constant help, guidance and support. Alasdair Stuart contributed magnificently to the sections on the results council-by-council and equalities. Other colleagues have assisted with the text and gathering data, including Christine McCartney, Gertrud Malmersjo and Hywel Nelson. -

Notice of Election
NOTICE OF ELECTION SCOTTISH BORDERS COUNCIL Election of Councillors Councillors are to be elected for each of the eleven wards of Scottish Borders Council. The number of councillors to be elected for each ward is as follows: Ward Number of Councillors to be elected 1. Tweeddale West Three 2. Tweeddale East Three 3. Galashiels and District Four 4. Selkirkshire Three 5. Leaderdale and Melrose Three 6. Mid Berwickshire Three 7. East Berwickshire Three 8. Kelso and District Three 9. Jedburgh and District Three 10. Hawick and Denholm Three 11. Hawick and Hermitage Three 1. Nomination forms can be obtained from the Election Office at Council Headquarters, Newtown St. Boswells, Melrose, TD6 0SA, by telephoning 01835 825005 or on the website at www.scotborders.gov.uk. The Election Office is open for the issue and delivery of nomination papers on weekdays from Tuesday, 14 March 2017 between 10am to 4pm. 2. Completed nomination forms must be delivered to the Returning Officer at the above address by 4pm on Wednesday, 29 March 2017. 3. An election will be held in each contested ward and voting will take place between 7am and 10pm on Thursday, 4 May 2017. 4. Applications to register to vote must reach the Electoral Registration Officer at Old School Building, Council Headquarters, Newtown St. Boswells, Melrose, TD6 0SA by Monday, 17 April 2017. Applications can be made online: https://www.gov.uk/register-to-vote. Postal or proxy voting 1. Any elector may apply for a postal or proxy vote at this election. 2. Applications, amendments or cancellations of postal votes must reach the Electoral Registration Officer, Old School Building, Council Headquarters, Newtown St. -

Constitution
AREA PARTNERSHIPS Constitution 1. Each Area Partnership will comprise – (a) Core Members: i. The elected Scottish Borders Councillors representing – Berwickshire Area Partnership: the six Elected Members for the Wards of East Berwickshire and Mid- Berwickshire; Cheviot Area Partnership: the six Elected Members for the Wards of Kelso & District and Jedburgh and District; Eildon Area Partnership: the ten Elected Members for the Wards of Galashiels & District, Leaderdale & Melrose, and Selkirkshire; Teviot & Liddesdale Area Partnership: the six Elected Members for the Wards of Hawick & Denholm and Hawick & Hermitage; Tweeddale Area Partnership: the six Elected Members for the Wards of Tweeddale East and Tweeddale West; ii. One representative from each of four different Community Councils in the Area Partnership area as non-voting members; iii. Any other non-voting member appointed by the Area Partnership up to a total core membership maximum of 20. (b) Additional Invited members: Invitations to attend and participate as non-voting members in meetings where there are relevant agenda items: i. appropriate representative(s) from the Community Planning partners (NHS Borders, Scottish Police, Scottish Fire & Rescue Service, Scottish Enterprise, Live Borders, RSLs, Borders College, Health & Social Care Integration Board, SEPA, SNH, Skills Development Scotland, SESTRAN, Third Sector, Visit Scotland); ii. a representative from any other Community Group or Local body, as appropriate; and iii. a representative from any other community of interest group, as appropriate. Chairman/Vice Chairman The Chairman and Vice Chairman of each Area Partnership shall be a Member of Scottish Borders Council. Quorum Three of the Scottish Borders Council Members of each Locality Committee, including at least one representative from each Ward, shall constitute a quorum, except for the Eildon Area Partnership where five shall constitute a Quorum. -

Local Government Boundary Commission for Scotland 5Th Review of Electoral Arrangements – Recommendations to Scottish Ministers
LOCAL GOVERNMENT BOUNDARY COMMISSION FOR SCOTLAND 5TH REVIEW OF ELECTORAL ARRANGEMENTS – RECOMMENDATIONS TO SCOTTISH MINISTERS Report by Chief Executive SCOTTISH BORDERS COUNCIL 29 June 2016 1 PURPOSE AND SUMMARY 1.1 This report advises the Council of the final report and recommendations being made by the Local Government Boundary Commission for Scotland to Scottish Ministers for the number of Councillors and the Electoral Ward Boundaries for the Scottish Borders Council area. 1.2 The Local Government Boundary Commission has submitted to Scottish Ministers its Reports and Final Recommendations for the number of Councillors and the electoral ward boundaries in each of Scotland’s 32 local authorities, which included those for the Scottish Borders Council area. The Commission has recommended that from May 2017, Scottish Borders Council should comprise 32 Councillors in 10 Wards, comprising 2 Wards each returning 4 Members, and 8 Wards each returning 3 Members. 1.3 The Council has previously provided two responses to consultations by the Commission (in April 2014 and May 2015) and another response to the then Scottish Minister for Local Government and Community Empowerment in February 2016. The Council has a six week period from 26 May 2016 to submit any comments to Scottish Ministers at the Directorate for Local Government and Communities. Members should note that any substantive change to that response made in February 2016 would require the suspension of Standing Orders, as the decision was taken within the preceding 6 months. 2 RECOMMENDATIONS 2.1 I recommend that the Council considers whether it wishes to make any further comments to Scottish Ministers regarding the final recommendations of the Local Government Boundary Commission for Scotland for the proposed number of Councillors and the Electoral Ward Boundaries for the Scottish Borders Council area. -
SCOTTISH BORDERS 03.Indd
Local Government Boundary Commission for Scotland Fourth Statutory Review of Electoral Arrangements Scottish Borders Council Area Report E06026 Report to Scottish Ministers July 2006 Local Government Boundary Commission for Scotland Fourth Statutory Review of Electoral Arrangements Scottish Borders Council Area Constitution of the Commission Chairman: Mr John L Marjoribanks Deputy Chairman: Mr Brian Wilson OBE Commissioners: Professor Hugh M Begg Dr A Glen Mr K McDonald Mr R Millham Report Number E06026 July 2006 Scottish Borders Council Area 1 Local Government Boundary Commission for Scotland 2 Scottish Borders Council Area Fourth Statutory Review of Electoral Arrangements Contents Page Summary Page 7 Part 1 Background Pages 9 – 14 Paragraphs Origin of the Review 1 The Local Governance (Scotland) Act 2004 2 – 4 Commencement of the 2004 Act 5 Directions from Scottish Ministers 6 – 9 Announcement of our Review 10 – 16 General Issues 17 – 18 Defi nition of Electoral Ward Boundaries 19 – 24 Electorate Data used in the Review 25 – 26 Part 2 The Review in Scottish Borders Council Area Pages 15 – 26 Paragraphs Meeting with the Scottish Borders Council 1 – 3 Concluded View of the Council 4 – 7 Aggregation of Existing Wards 8 – 11 Initial Proposals 12 – 19 Informing the Council of our Initial Proposals 20 – 21 The Scottish Borders Council Response 22 – 23 Consideration of the Council Response to the Initial Proposals 24 – 30 Provisional Proposals 31 – 35 Representations 36 Consideration of Representations 37 – 46 Part 3 Final Recommendation Pages -
Local Government Boundary Commission for Scotland 5Th Review of Electoral Arrangements – Proposals for Wards
LOCAL GOVERNMENT BOUNDARY COMMISSION FOR SCOTLAND 5TH REVIEW OF ELECTORAL ARRANGEMENTS – PROPOSALS FOR WARDS Report by Chief Executive SCOTTISH BORDERS COUNCIL 21 May 2015 1 PURPOSE AND SUMMARY 1.1 This report seeks approval for a proposed response to the Local Government Boundary Commission for Scotland’s proposals for wards in the Scottish Borders Council area. 1.2 The current proposals by the Local Government Boundary Commission for Scotland for the Scottish Borders Council area present an electoral arrangement for 32 Councillors representing 8 x 3-member wards and 2 x 4-member wards, reducing the number of wards in the area by 1 and reducing Councillor numbers by 2. Appendix 1 details the electorates and associated variation from parity of the proposed Wards, and gives details of the Commission’s new Ward proposals, in particular Jedburgh, Denholm & Hermitage and Hawick. The proposals remove the existing Hawick & Denholm and Hawick & Hermitage Wards, placing Newcastleton and Denholm (and surrounding areas) into a new Jedburgh, Denholm & Hermitage Ward. A minor change is also proposed moving around 80 electors from Charlesfield from the Jedburgh Ward into the Selkirkshire Ward, with the detail of this change in boundary given in Appendix 2. 1.3 The Commission has made it clear that parity of electors to Councillors is the main determinant for Councillor numbers and ward design. This has been used to develop a response for the Council, proposing a different configuration of Wards, retaining Newcastleton in a Hawick Ward. Details of this are given in Appendix 3. Consideration has been given to including Denholm in the Hawick Ward but this is not being recommended as it would take the total electorate for that Ward 20% above parity.