Interactionsof Streptococcus Suis with Host Mucosa
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
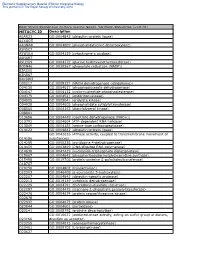
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

Increasing the Amylose Content of Durum Wheat Through Silencing of the Sbeiia Genes
Sestili et al. BMC Plant Biology 2010, 10:144 http://www.biomedcentral.com/1471-2229/10/144 RESEARCH ARTICLE Open Access IncreasingResearch article the amylose content of durum wheat through silencing of the SBEIIa genes Francesco Sestili1, Michela Janni1, Angela Doherty2, Ermelinda Botticella1, Renato D'Ovidio1, Stefania Masci1, Huw D Jones2 and Domenico Lafiandra*1 Abstract Background: High amylose starch has attracted particular interest because of its correlation with the amount of Resistant Starch (RS) in food. RS plays a role similar to fibre with beneficial effects for human health, providing protection from several diseases such as colon cancer, diabetes, obesity, osteoporosis and cardiovascular diseases. Amylose content can be modified by a targeted manipulation of the starch biosynthetic pathway. In particular, the inactivation of the enzymes involved in amylopectin synthesis can lead to the increase of amylose content. In this work, genes encoding starch branching enzymes of class II (SBEIIa) were silenced using the RNA interference (RNAi) technique in two cultivars of durum wheat, using two different methods of transformation (biolistic and Agrobacterium). Expression of RNAi transcripts was targeted to the seed endosperm using a tissue-specific promoter. Results: Amylose content was markedly increased in the durum wheat transgenic lines exhibiting SBEIIa gene silencing. Moreover the starch granules in these lines were deformed, possessing an irregular and deflated shape and being smaller than those present in the untransformed controls. Two novel granule bound proteins, identified by SDS- PAGE in SBEIIa RNAi lines, were investigated by mass spectrometry and shown to have strong homologies to the waxy proteins. RVA analysis showed new pasting properties associated with high amylose lines in comparison with untransformed controls. -

Product Guide
www.megazyme.com es at dr hy o rb a C • s e t a r t s b u S e m y z n E • s e m y z n E • s t i K y a s s A Plant Cell Wall & Biofuels Product Guide 1 Megazyme Test Kits and Reagents Purity. Quality. Innovation. Barry V. McCleary, PhD, DScAgr Innovative test methods with exceptional technical support and customer service. The Megazyme Promise. Megazyme was founded in 1988 with the We demonstrate this through the services specific aim of developing and supplying we offer, above and beyond the products we innovative test kits and reagents for supply. We offer worldwide express delivery the cereals, food, feed and fermentation on all our shipments. In general, technical industries. There is a clear need for good, queries are answered within 48 hours. To validated methods for the measurement of make information immediately available to the polysaccharides and enzymes that affect our customers, we established a website in the quality of plant products from the farm 1994, and this is continually updated. Today, it gate to the final food. acts as the source of a wealth of information on Megazyme products, but also is the hub The commitment of Megazyme to “Setting of our commercial activities. It offers the New Standards in Test Technology” has been possibility to purchase and pay on-line, to continually recognised over the years, with view order history, to track shipments, and Megazyme and myself receiving a number many other features to support customer of business and scientific awards. -

Transcriptomic Analysis of Streptococcus Suis in Response to Ferrous Iron and Cobalt Toxicity
G C A T T A C G G C A T genes Article Transcriptomic Analysis of Streptococcus suis in Response to Ferrous Iron and Cobalt Toxicity Mengdie Jia 1,2, Man Wei 1,2, Yunzeng Zhang 1,2 and Chengkun Zheng 1,2,* 1 Joint International Research Laboratory of Agriculture and Agri-Product Safety, The Ministry of Education of China, Yangzhou University, Yangzhou 225009, China; [email protected] (M.J.); [email protected] (M.W.); [email protected] (Y.Z.) 2 Jiangsu Key Laboratory of Zoonosis, Yangzhou University, Yangzhou 225009, China * Correspondence: [email protected]; Tel.: +86-1520-527-9658 Received: 16 August 2020; Accepted: 1 September 2020; Published: 2 September 2020 Abstract: Streptococcus suis is a zoonotic pathogen causing serious infections in swine and humans. Although metals are essential for life, excess amounts of metals are toxic to bacteria. Transcriptome-level data of the mechanisms for resistance to metal toxicity in S. suis are available for no metals other than zinc. Herein, we explored the transcriptome-level changes in S. suis in response to ferrous iron and cobalt toxicity by RNA sequencing. Many genes were differentially expressed in the presence of excess ferrous iron and cobalt. Most genes in response to cobalt toxicity showed the same expression trends as those in response to ferrous iron toxicity. qRT-PCR analysis of the selected genes confirmed the accuracy of RNA sequencing results. Bioinformatic analysis of the differentially expressed genes indicated that ferrous iron and cobalt have similar effects on the cellular processes of S. suis. Ferrous iron treatment resulted in down-regulation of several oxidative stress tolerance-related genes and up-regulation of the genes in an amino acid ABC transporter operon. -

Streptococcus Suis
Identification ofStreptococcus suis Meningitis by Direct Triplex Real-Time PCR, Burkina Faso Mahamoudou Ouattara, Mamadou Tamboura, Dinanibe Kambire, Mahamoudou Sanou, Kalifa Ouattara, Malika Congo, Adama Kaboré, Soufiane Sanou, Elie Kabré, Sable Sharpley, Theresa Tran, Stephanie Schwartz, Soumeya Ouangraoua, Abdoul-salam Ouedraogo, Lassana Sangaré, Rasmata Ouedraogo-Traore, Cynthia G. Whitney, Bernard Beall Meningitis confirmation in Burkina Faso uses PCR for The Study detecting Streptococcus pneumoniae, Neisseria menin- Burkina Faso conducts nationwide case-based sur- gitidis, or Hemophilus influenzae. We identified 38 cases veillance for bacterial meningitis. Cerebrospinal fluid of meningitis among 590 that were PCR-positive for 3 (CSF) samples collected from patients with suspected nonpneumococcal streptococcal pathogens, including 21 meningitis are sent to 1 of 5 national laboratories for cases of Streptococcus suis. Among the country’s 13 re- confirmation by culture and real-time PCR testing (6). gions, 10 had S. suis–positive cases. Because of multiple challenges encountered by the laboratories in isolating bacteria from CSF, the confir- treptococcus suis is a commensal organism of the mation of meningitis cases relies heavily on molecular upper respiratory tract of pigs that can occasion- S detection (6). The real-time PCR assay currently used ally cause severe invasive infections in these animals at the national laboratories only detects Streptococcus (1,2). The bacterium also can infect humans who have pneumoniae, Neisseria meningitidis, and Haemophilus close contact with pigs or pork products, leading to influenzae. Between 2015 and 2018, the national labo- serious diseases such as meningitis, endocarditis, and ratories tested 7,174 CSF samples from patients with sepsis (3). S. -

Identification of Conditionally Essential Genes for Streptococcus Suis Infection in Pigs
Virulence ISSN: (Print) (Online) Journal homepage: https://www.tandfonline.com/loi/kvir20 Identification of conditionally essential genes for Streptococcus suis infection in pigs Jesús Arenas , Aldert Zomer , Jose Harders-Westerveen , Hester J. Bootsma , Marien I. De Jonge , Norbert Stockhofe-Zurwieden , Hilde E. Smith & Astrid De Greeff To cite this article: Jesús Arenas , Aldert Zomer , Jose Harders-Westerveen , Hester J. Bootsma , Marien I. De Jonge , Norbert Stockhofe-Zurwieden , Hilde E. Smith & Astrid De Greeff (2020) Identification of conditionally essential genes for Streptococcussuis infection in pigs, Virulence, 11:1, 446-464, DOI: 10.1080/21505594.2020.1764173 To link to this article: https://doi.org/10.1080/21505594.2020.1764173 © 2020 The Author(s). Published by Informa View supplementary material UK Limited, trading as Taylor & Francis Group. Published online: 18 May 2020. Submit your article to this journal Article views: 201 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at https://www.tandfonline.com/action/journalInformation?journalCode=kvir20 VIRULENCE 2020, VOL. 11, NO. 1, 446–464 https://doi.org/10.1080/21505594.2020.1764173 RESEARCH PAPER Identification of conditionally essential genes for Streptococcus suis infection in pigs Jesús Arenas a,b, Aldert Zomer c,d, Jose Harders-Westerveena, Hester J. Bootsmad, Marien I. De Jonged, Norbert Stockhofe-Zurwiedena, Hilde E. Smitha, and Astrid De Greeff a aDepartment of Infection Biology, Wageningen Bioveterinary Research (WBVR), -

Studies of Barley Limit Dextrinase I I
b ¡\il i: ilq.5l¡Tt-!iÈ' ta. S.S LIBRARY STUDIES OF BARLEY LIMIT DEXTRINASE I I I I by I l I ¡ I Michael John Sissons ì B.Ag.Sc. (University of Adelaide)' I I M.Ag.Sc. (La Trobe UniversitY) i l A thesis submitted to the University of Adelaide for the degree of Doctor of Philosophy Departnent of Plant Science, Waite Agricultural Resea¡ch Institute, Glen Osmond, South Australia October, 1991 LIST OF CONTENTS Contents Page No. Summary i-ü Statement of originality and consent for photocopy or loan lU Acknowledgements iv List of publications v Chapter 1: LITERATURE REVIEW 1.1 Introduction I 1.2 Properties of limit dextrinase 2 t.2.r Purification 2 1.2.2 Enzyme properties 3 t.2.3 Effect of inhibitors 3 r.2.4 Polymorphism 7 t.2.5 Substrate specificity 7 1.2.5.1 Action of limit dextrinase on oligosaccharides 7 t.2.5.2 Polysaccharides 7 1.3 Methods of Assay 9 1.3.1 Detection of Limit Dextrinase Activity in Electrophoretic Gels 10 t.4 Synthesis of limit dextrinase t2 1.4.1 Mechanism of Increase in Limit Dextrinase Activity during Germination 13 1.5 Effect of Barley Genotype and Environment on Limit Dextrinase ActivitY 15 1.6 Limit dextrinase - Role in Malting and Brewing 16 1.6.1 Effect of Kilning on Limit Dextrinase Activity 18 r.6.2 Effect of Mashing on Limit Dextrinase Activity 18 1.6.3 Limit 0extrinase-Role in Speciality Brewing, Distiling and Related Iridustries 2l 1.6.4 Relationship beween Limit Dextrinase Activity, Wort Fermentability and Alcohol Production 22 r.7 Role of Limit Dextrinase in Starch Degradation 23 1.8 Conclusions 24 Chapter -

Streptococcosis Humans and Animals
Zoonotic Importance Members of the genus Streptococcus cause mild to severe bacterial illnesses in Streptococcosis humans and animals. These organisms typically colonize one or more species as commensals, and can cause opportunistic infections in those hosts. However, they are not completely host-specific, and some animal-associated streptococci can be found occasionally in humans. Many zoonotic cases are sporadic, but organisms such as S. Last Updated: September 2020 equi subsp. zooepidemicus or a fish-associated strain of S. agalactiae have caused outbreaks, and S. suis, which is normally carried in pigs, has emerged as a significant agent of streptoccoccal meningitis, septicemia, toxic shock-like syndrome and other human illnesses, especially in parts of Asia. Streptococci with human reservoirs, such as S. pyogenes or S. pneumoniae, can likewise be transmitted occasionally to animals. These reverse zoonoses may cause human illness if an infected animal, such as a cow with an udder colonized by S. pyogenes, transmits the organism back to people. Occasionally, their presence in an animal may interfere with control efforts directed at humans. For instance, recurrent streptococcal pharyngitis in one family was cured only when the family dog, which was also colonized asymptomatically with S. pyogenes, was treated concurrently with all family members. Etiology There are several dozen recognized species in the genus Streptococcus, Gram positive cocci in the family Streptococcaceae. Almost all species of mammals and birds, as well as many poikilotherms, carry one or more species as commensals on skin or mucosa. These organisms can act as facultative pathogens, often in the carrier. Nomenclature and identification of streptococci Hemolytic reactions on blood agar and Lancefield groups are useful in distinguishing members of the genus Streptococcus. -

Detection of Various Streptococcus Spp. and Their Antimicrobial Resistance Patterns in Clinical Specimens from Austrian Swine Stocks
antibiotics Article Detection of Various Streptococcus spp. and Their Antimicrobial Resistance Patterns in Clinical Specimens from Austrian Swine Stocks René Renzhammer 1,* , Igor Loncaric 2, Marisa Ladstätter 1, Beate Pinior 3, Franz-Ferdinand Roch 3, Joachim Spergser 2, Andrea Ladinig 1 and Christine Unterweger 1 1 University Clinic for Swine, Department for Farm Animals and Veterinary Public Health, University of Veterinary Medicine, 1210 Vienna, Austria; [email protected] (M.L.); [email protected] (A.L.); [email protected] (C.U.) 2 Department for Pathobiology, Institute of Microbiology, University of Veterinary Medicine, 1210 Vienna, Austria; loncarici@staff.vetmeduni.ac.at (I.L.); i102us01@staff.vetmeduni.ac.at (J.S.) 3 Unit of Veterinary Public Health and Epidemiology, Department for Farm Animals and Veterinary Public Health, Institute of Food Safety, Food Technology and Veterinary Public Health, University of Veterinary Medicine, 1210 Vienna, Austria; [email protected] (B.P.); [email protected] (F.-F.R.) * Correspondence: [email protected] Received: 31 October 2020; Accepted: 9 December 2020; Published: 11 December 2020 Abstract: Knowledge of pathogenic potential, frequency and antimicrobial resistance patterns of porcine Streptococcus (S.) spp. other than S. suis is scarce. Between 2016 and 2020, altogether 553 S. spp. isolates were recovered from clinical specimens taken from Austrian swine stocks and submitted for routine microbiological examination. Antimicrobial susceptibility testing towards eight antimicrobial substances was performed using disk diffusion test. All isolates from skin lesions belonged to the species S. dysgalactiae subspecies equisimilis (SDSE). S. hyovaginalis was mainly isolated from the upper respiratory tract (15/19) and S. -

Streptococcus Suis Induces Expression of Cyclooxygenase-2 in Porcine Lung Tissue
microorganisms Article Streptococcus suis Induces Expression of Cyclooxygenase-2 in Porcine Lung Tissue Muriel Dresen 1,†, Josephine Schenk 1,†, Yenehiwot Berhanu Weldearegay 1 ,Désirée Vötsch 1, Wolfgang Baumgärtner 2, Peter Valentin-Weigand 1,* and Andreas Nerlich 1,3,* 1 Institute for Microbiology, Department of Infectious Diseases, University of Veterinary Medicine Hannover, Foundation, 30173 Hannover, Germany; [email protected] (M.D.); [email protected] (J.S.); [email protected] (Y.B.W.); [email protected] (D.V.) 2 Institute for Pathology, University of Veterinary Medicine Hannover, Foundation, 30173 Hannover, Germany; [email protected] 3 Veterinary Centre for Resistance Research, Department of Veterinary Medicine, Freie Universität Berlin, 14163 Berlin, Germany * Correspondence: [email protected] (P.V.-W.); [email protected] (A.N.); Tel.: +49-511-856-7362 (P.V.-W.); +49-30-838-58508 (A.N.) † These authors contributed equally to this work. Abstract: Streptococcus suis is a common pathogen colonising the respiratory tract of pigs. It can cause meningitis, sepsis and pneumonia leading to economic losses in the pig industry worldwide. Cyclooxygenase-2 (COX-2) and its metabolites play an important regulatory role in different bio- logical processes like inflammation modulation and immune activation. In this report we analysed the induction of COX-2 and the production of its metabolite prostaglandin E2 (PGE2) in a porcine precision-cut lung slice (PCLS) model. Using Western blot analysis, we found a time-dependent Citation: Dresen, M.; Schenk, J.; induction of COX-2 in the infected tissue resulting in increased PGE2 levels. -

Evaluation of Saccharifying Methods for Alcoholic Fermentation of Starchy Substrates Alice Lee Iowa State College
Iowa State University Capstones, Theses and Retrospective Theses and Dissertations Dissertations 1955 Evaluation of saccharifying methods for alcoholic fermentation of starchy substrates Alice Lee Iowa State College Follow this and additional works at: https://lib.dr.iastate.edu/rtd Part of the Biochemistry Commons Recommended Citation Lee, Alice, "Evaluation of saccharifying methods for alcoholic fermentation of starchy substrates " (1955). Retrospective Theses and Dissertations. 13626. https://lib.dr.iastate.edu/rtd/13626 This Dissertation is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Retrospective Theses and Dissertations by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. NOTE TO USERS This reproduction is the best copy available. ® UMI EVALUATION OF SACCHARIFYING METHODS FOR ALCOHOLIC FERMENTATION OF STARCHY SUBSTRATES by Alice Lee A Dlseertatlon Submitted to the Graduate Faculty In Partial Fulfillment of The RequirementB for the Degree of DOCTOR OF PHILOSOPHY Major Subjects Blochensletry Approved: Signature was redacted for privacy. In Charge of Major Work Signature was redacted for privacy. Head of Major Department Signature was redacted for privacy. Dean of Graduate College Iowa State College 1955 UMI Number: DP12815 INFORMATION TO USERS The quality of this reproduction is dependent upon the quality of the copy submitted. Broken or indistinct print, colored or poor quality illustrations and photographs, print bleed-through, substandard margins, and improper alignment can adversely affect reproduction. In the unlikely event that the author did not send a complete manuscript and there are missing pages, these will be noted. -

STUDY of STARCH DEBRANCHING ENZYMES in DEVELOPING WHEAT KERNELS a Thesis Submitted to the College of Graduate Studies and Resear
STUDY OF STARCH DEBRANCHING ENZYMES IN DEVELOPING WHEAT KERNELS A Thesis Submitted to the College of Graduate Studies and Research in Partial Fulfilment of the Requirements for the Degree of Doctor of Philosophy in the Department of Biochemistry University of Saskatchewan Saskatoon By Supatcharee Netrphan Spring 2002 © Copyright Supatcharee Netrphan, 2002. All rights reserved. PERMISSION TO USE In presenting this thesis in partial fulfilment of the requirements for a Postgraduate degree from the University of Saskatchewan, I agree that the Libraries of this University may make it freely available for inspection. I further agree that permission for copying of this thesis in any manner, in whole or in part, for scholarly purposes may be granted by the professor or professors who supervised my thesis work or, in their absence, by the Head of the Department or the Dean of the College in which my thesis work was done. It is understood that any copying or publication or use of this thesis or parts thereof for financial gain shall not be allowed without my written permission. It is also understood that due recognition shall be given to me and to the University of Saskatchewan in any scholarly use which may be made of any material in my thesis. Requests for permission to copy or to make other use of material in this thesis in whole or in part should be addressed to: Head of the Department of Biochemistry University of Saskatchewan 107 Wiggins Road Saskatoon, Saskatchewan S7N 5E5 i ABSTRACT Starch debranching enzymes, which specifically hydrolyse a-1,6 glucosidic bonds in glucans containing both a-1,4 and a-1,6 linkages, are classified into two types: isoamylase (EC.