Webinar Transcript
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

J. Michael Mcginnis, Md, Ma, Mpp
J. MICHAEL MCGINNIS, MD, MA, MPP National Academy of Medicine, the National Academies, 500 Fifth Street NW, Washington DC 20001, (202) 334-3963, [email protected] Highlights: Michael McGinnis is a physician and epidemiologist who lives and works in Washington DC. Through his writing, government service, and work in philanthropy, he has been a long-time contributor to national and international field leadership in health, health care, and health policy. He currently serves at the National Academy of Medicine (NAM), where he is the Leonard D. Schaeffer Executive Officer, Senior Scholar, and Executive Director of the NAM’s Leadership Consortium for public and private collaboration on behalf of a continuously learning health system. Previously, he served as founding Director, respectively, of the Robert Wood Johnson Foundation’s (RWJF) Health Group, the World Health Organization’s Office for Health Reconstruction in Bosnia, the federal Office of Research Integrity (interim), and the federal Office of Disease Prevention and Health Promotion. In a tenure unusual for political and policy posts, he held continuous appointment through the Carter, Reagan, Bush and Clinton Administrations at the Department of Health and Human Services, with policy responsibilities for disease prevention and health promotion (1977-1995). Programs and policies conceived and launched at his initiative include the Healthy People process establishing national health goals and objectives (1979-present), the U.S. Preventive Services Task Force (1984-present), the Dietary Guidelines for Americans (with USDA, 1980- present), the multi-level Public Health Functions Steering Group and the Ten Essential Services of Public Health (1994-present), the RWJF Active Living family of programs (2000-present), the RWJF Young Epidemiology Scholars Program (2001-2012), the RWJF Health and Society Scholars Program (2002-2017), and the current Learning Health System initiative of the NAM. -

CTRI Trial Data
PDF of Trial CTRI Website URL - http://ctri.nic.in Clinical Trial Details (PDF Generation Date :- Tue, 28 Sep 2021 15:39:14 GMT) CTRI Number CTRI/2009/091/001080 [Registered on: 28/06/2010] - Last Modified On Post Graduate Thesis Type of Trial Type of Study Study Design Randomized, Parallel Group, Placebo Controlled Trial Public Title of Study A clinical Trial to study the safety, immunogenicity and tolerability of a tetravalent rotavirus vaccine in Indian infants. Scientific Title of Phase I/II, randomized, double-blind, placebo-controlled, dosage selection (10e5.5 or 10e6.25 FFU Study of each constituent serotype per 0.5 mL) study to evaluate the safety, tolerability, and immunogenicity of a 3-dose series of Live Attenuated Tetravalent (G1-G4) Bovine-Human Reassortant Rotavirus Vaccine [BRV-TV] administered to healthy Indian infants. Secondary IDs if Any Secondary ID Identifier NCT01061658 ClinicalTrials.gov SBL/BRV-TV/Form1/PhI/2009/0100 Protocol Number SBL/BRV-TV/Form1/PhI/2009/0100 Protocol Number Details of Principal Details of Principal Investigator Investigator or overall Name Dr. Gagandeep Kang Trial Coordinator (multi-center study) Designation Affiliation Address Department of Gastrointestinal Sciences, Christian Medical College Vellore TAMIL NADU 632004 India Phone 0416-2282052 Fax 0416-2282486 Email [email protected] Details Contact Details Contact Person (Scientific Query) Person (Scientific Name Dr. Raman Rao Query) Designation Affiliation Shantha Biotechnics Limited Address VP, R&D, 4th Floor, Vasantha Chambers, Fateh Maidan Road, Basheer Bagh Hyderabad ANDHRA PRADESH 500004 India Phone 040-66301800 Fax 040-23234133 Email [email protected] Details Contact Details Contact Person (Public Query) Person (Public Query) Name Dr. -

THE SURGEON GENERAL and the BULLY PULPIT Michael Stobbe a Dissertation Submitted to the Faculty of the University of North Carol
THE SURGEON GENERAL AND THE BULLY PULPIT Michael Stobbe A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Public Health in the Department of Health Policy and Administration, School of Public Health Chapel Hill 2008 Approved by: Ned Brooks Jonathan Oberlander Tom Ricketts Karl Stark Bryan Weiner ABSTRACT MIKE STOBBE: The Surgeon General and the Bully Pulpit (Under the direction of Ned Brooks) This project looks at the role of the U.S. Surgeon General in influencing public opinion and public health policy. I examined historical changes in the administrative powers of the Surgeon General, to explain what factors affect how a Surgeon General utilizes the office’s “bully pulpit,” and assess changes in the political environment and in who oversees the Surgeon General that may affect the Surgeon General’s future ability to influence public opinion and health. This research involved collecting and analyzing the opinions of journalists and key informants such as current and former government health officials. I also studied public documents, transcripts of earlier interviews and other materials. ii TABLE OF CONTENTS LIST OF TABLES.................................................................................................................v Chapter 1. INTRODUCTION ...............................................................................................1 Background/Overview .........................................................................................1 -

“Women Rarely Put Themselves Forward Despite Being Very Capable.”
IN CONVERSATION “Women rarely put themselves forward despite being very capable.” Professor Gagandeep Kang is currently the Executive Director of Translational Health Science and Technology Institute (THSTI), Faridabad. She is the first Indian woman scientist to be elected as Fellow of Royal Society (FRS) by the Royal Society in the UK. She is a leading scientist with over 300 scientific research papers published on diarrhoeal infections in children, mainly from work done at the Christian Medical College (CMC) in Vellore. Amongst several awards, she is the recipient of the Infosys Life Sciences Award in 2016. She is a member of many review and advisory committees for national and international funding agencies related to public health. Dr. Kang has chaired the WHO SEAR’s Regional Immunization Technical Advisory Group since 2015. In an interview given to PARUL R. SHETH for Science Reporter, Dr Gagandeep Kang talks about her work on rotaviruses, safety of Indian vaccines, the advantages and disadvantages of being a woman in science, and her experiences with community health programmes. 20 | Science Reporter | June 2019 GAGANDEEP KANG: My colleague, Ira and I published a PARUL R. SHETH: Congratulations to you for being the paper a couple of years ago, comparing children of doctors and first woman scientist to be elected as FRS in 360 years! This children who lived in urban slum areas, showing that middle indeed is a great honour and we are all proud of you. Your class Indian children carry in their guts one-fourth the number work has been recognised for its quality and impact. -

Annual Meeting
Volume 97 | Number 5 Volume VOLUME 97 NOVEMBER 2017 NUMBER 5 SUPPLEMENT SIXTY-SIXTH ANNUAL MEETING November 5–9, 2017 The Baltimore Convention Center | Baltimore, Maryland USA The American Journal of Tropical Medicine and Hygiene The American Journal of Tropical astmh.org ajtmh.org #TropMed17 Supplement to The American Journal of Tropical Medicine and Hygiene ASTMH FP Cover 17.indd 1-3 10/11/17 1:48 PM Welcome to TropMed17, our yearly assembly for stimulating research, clinical advances, special lectures, guests and bonus events. Our keynote speaker this year is Dr. Paul Farmer, Co-founder and Chief Strategist of Partners In Health (PIH). In addition, Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, will deliver a plenary session Thursday, November 9. Other highlighted speakers include Dr. Scott O’Neill, who will deliver the Fred L. Soper Lecture; Dr. Claudio F. Lanata, the Vincenzo Marcolongo Memorial Lecture; and Dr. Jane Cardosa, the Commemorative Fund Lecture. We are pleased to announce that this year’s offerings extend beyond communicating top-rated science to direct service to the global community and a number of novel events: • Get a Shot. Give a Shot.® Through Walgreens’ Get a Shot. Give a Shot.® campaign, you can not only receive your free flu shot, but also provide a lifesaving vaccine to a child in need via the UN Foundation’s Shot@Life campaign. • Under the Net. Walk in the shoes of a young girl living in a refugee camp through the virtual reality experience presented by UN Foundation’s Nothing But Nets campaign. -

THE SURGEON GENERAL and the BULLY PULPIT Michael Stobbe a Dissertation Submitted to the Faculty of the University of North Carol
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Carolina Digital Repository THE SURGEON GENERAL AND THE BULLY PULPIT Michael Stobbe A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Public Health in the Department of Health Policy and Administration, School of Public Health Chapel Hill 2008 Approved by: Ned Brooks Jonathan Oberlander Tom Ricketts Karl Stark Bryan Weiner ABSTRACT MIKE STOBBE: The Surgeon General and the Bully Pulpit (Under the direction of Ned Brooks) This project looks at the role of the U.S. Surgeon General in influencing public opinion and public health policy. I examined historical changes in the administrative powers of the Surgeon General, to explain what factors affect how a Surgeon General utilizes the office’s “bully pulpit,” and assess changes in the political environment and in who oversees the Surgeon General that may affect the Surgeon General’s future ability to influence public opinion and health. This research involved collecting and analyzing the opinions of journalists and key informants such as current and former government health officials. I also studied public documents, transcripts of earlier interviews and other materials. ii TABLE OF CONTENTS LIST OF TABLES.................................................................................................................v Chapter 1. INTRODUCTION ...............................................................................................1 -

Quotes on Rotavirus Vaccine News
Additional statements on ROTASIIL® Phase 3 India clinical trial results It is important to have a new approach to look at rotavirus vaccine efficacy. Rotavirus vaccination in developing countries has always struggled with interpretation of efficacy through use of markers of seroconversion or reduction of death in the community. Both are erroneous because of babies being breastfed as well as high infant mortality under five years of age in certain geographic regions of India. Better indicators have been surrogate indicators, which reflect fewer admissions of children to the hospital related to rotavirus as well as a reduced stay in the hospital due to the same. These markers have worked well in Mexico and El Salvador. Prof. N.K. Ganguly, Former Director General, Indian Council of Medical Research; Visiting Professor of Eminence, Policy Center for Biomedical Research, Translational Health Science & Technology Institute, Faridabad, India India now has another rotavirus vaccine that is manufactured indigenously. This is a win for the children of the country as it will support the Government of India’s efforts to roll out the rotavirus vaccine across the country through the Universal Immunization Programme. Dr. M.K. Bhan, Former Secretary, Department of Biotechnology, Government of lndia I am delighted that India has another rotavirus vaccine. Scientific studies have shown that rotavirus vaccines are making a major public health impact. Swift and significant declines in hospitalizations and deaths due to rotavirus and all‐cause diarrhea have been observed in many of the countries that have introduced rotavirus vaccines into their national immunization programs. Dr. Gagandeep Kang, Executive Director of Translational Health Science & Technology Institute, Faridabad, India, and member of the ROTA Council Rotavirus is the most common cause of diarrhea and one of the leading cause of under‐five child mortality. -

Distribution Agreement in Presenting This Thesis Or Dissertation As A
Distribution Agreement In presenting this thesis or dissertation as a partial fulfillment of the requirements for an advanced degree from Emory University, I hereby grant to Emory University and its agents the non-exclusive license to archive, make accessible, and display my thesis or dissertation in whole or in part in all forms of media, now or hereafter known, including display on the world wide web. I understand that I may select some access restrictions as part of the online submission of this thesis or dissertation. I retain all ownership rights to the copyright of the thesis or dissertation. I also retain the right to use in future works (such as articles or books) all or part of this thesis or dissertation. Signature: _____________________________ ______________ Anita L. Renahan-White Date Faith and the Public's Health By Anita L. Renahan-White Master of Divinity Candler School of Theology ___________________________________________ [Thesis Advisor's signature] Dr. John Blevins Committee Chair ___________________________________________ [Member's signature] Dr. Steven J. Kraftchick Director of General and Advanced Studies ___________________________________________ [Member's signature] Dr. Emmanuel Lartey Committee Member Faith and the Public's Health By Anita L. Renahan-White MPH Emory University 1993 Thesis Committee Chair: John Blevins, ThD An abstract of A thesis submitted to the Faculty of the Candler School of Theology in partial fulfillment of the requirements for the degree of Master of Divinity 2012 Abstract Faith and the Public's Health By Anita L. Renahan-White In the following thesis "Faith and the Public's Health," I detail findings from research and interviews I conducted from March 2011 through February 2012. -
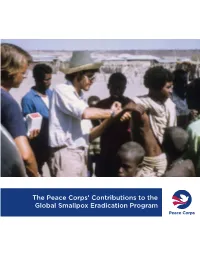
The Peace Corps' Contributions to the Global Smallpox Eradication Program
The Peace Corps’ Contributions to the Global Smallpox Eradication Program About the Office of Strategic Information, Research, and Planning (OSIRP) It is the mission of OSIRP to advance evidence-based management at the Peace Corps by guiding agency strategic planning; monitoring and evaluating agency-level performance and programs; conducting research to generate new insights in the fields of international development, cultural exchange, and Volunteer service; enhancing the stewardship and governance of agency data; and helping to shape agency engagement on high-level, governmentwide initiatives. Front Cover: Peace Corps Volunteers Robert Steinglass and Doug Arbuckle administering the smallpox vaccine in Mille, Ethiopia, in 1974. Photo: Steinglass, personal collection. ii Dedication This report is dedicated to the memory of Dr. Donald Ainslie “D. A.” Henderson (September 7, 1928—August 19, 2016), a seminal figure in the field of smallpox eradication. The Peace Corps is deeply appreciative of having had the opportunity to correspond with Dr. Henderson about the contributions of Peace Corps Volunteers and returned Volunteers within the context of the global eradication program. His charismatic leadership, tireless energy, and unflagging devotion to this program inspired countless public health workers around the world, including many of the returned Peace Corps Volunteers interviewed for this report. iii Acknowledgments In 1806, approximately 10 years after Dr. Edward Jenner conducted the first documented experiment with smallpox vaccination, laying the foundations of modern medicine, President Thomas Jefferson wrote to the English physician and scientist. Jefferson acknowledged the importance of this discovery, extending “a portion of the tribute of gratitude due to you from the whole human family. -

Seamus Heaney Exhibit Is Tribute to Friend of Emory Emory Photo Video
Welcome to spring semester SPECIAL ISSUE Online all the time at news.emory.edu JANUARY 21, 2014 ATHLETICS BEARDEN EXHIBIT Oxford’s organic farm 2 Eagle teams ‘Black Odyssey’ return strong draws scholars, Spring break alternatives 5 for 2014. faculty and local Calendar highlights 6-7 Page 3 celebrities. Page 12 Founders Week 11 University Course expands 11 Seamus Heaney exhibit is tribute to friend of Emory Emory Photo Video Nobel Prize-winning poet Seamus Heaney had a long relationship with Emory, having presented the inaugural Richard Ellmann Lectures. By MAUREEN MCGAVIN beginning at 6 p.m. with W. Ronald Schuchard, Emory profes- were part of an old bench from Carysfort College in Dublin, sor emeritus of English, as toastmaster. where Heaney taught in the 1970s. “Seamus Heaney: The Music of What Happens,” opening Geraldine Higgins, director of Emory’s Irish studies pro- There will also be a custom-built media space where people Saturday, Feb. 22, will be Emory’s first major exhibition cel- gram, curated the exhibition, choosing the title from a line can listen to recordings of Heaney and other distinguished writ- ebrating the life of the late Irish poet and Nobel Prize winner. in the Heaney poem “Song:” “The finest music of all is the ers, artists and well-known figures, including Irish actor Liam Heaney had a special connection to Emory beginning music of what happens.” Neeson and novelist Sir Salman Rushdie, reading his poems. with his first reading in March 1981. He delivered the inau- The exhibition will showcase Heaney’s poems and drafts A large kite will be at the center of the exhibition, suspended gural Richard Ellmann Lectures in Modern Literature in showing his handwritten revisions, rare publications, and over the spiral staircase in the gallery that descends to the lower 1988, donated his lecture notes to Emory’s Manuscript, artists’ books containing his poetry. -

Proquest Dissertations
'RANDOM MURDER BY TECHNOLOGY': THE ROLE OF SCIENTIFIC AND BIOMEDICAL EXPERTS IN THE ANTI-NUCLEAR MOVEMENT, 1969 - 1992 LISA A. RUMIEL A DISSERTATION SUBMITTED TO THE FACULTY OF GRADUATE STUDIES IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY GRADUATE PROGRAM IN HISTORY YORK UNIVERSITY, TORONTO, ONTARIO AUGUST 2009 Library and Archives Bibliotheque et 1*1 Canada Archives Canada Published Heritage Direction du Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington OttawaONK1A0N4 Ottawa ON K1A 0N4 Canada Canada Your file Votre reference ISBN: 978-0-494-54104-3 Our file Notre r6f6rence ISBN: 978-0-494-54104-3 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing Library and permettant a la Bibliotheque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par telecommunication ou par I'lnternet, preter, telecommunication or on the Internet, distribuer et vendre des theses partout dans le loan, distribute and sell theses monde, a des fins commerciales ou autres, sur worldwide, for commercial or non support microforme, papier, electronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriete du droit d'auteur ownership and moral rights in this et des droits moraux qui protege cette these. Ni thesis. Neither the thesis nor la these ni des extraits substantiels de celle-ci substantial extracts from it may be ne doivent etre imprimes ou autrement printed or otherwise reproduced reproduits sans son autorisation. -

'Share Her Journey' the First Indian Shipyard to Deliver 100 Warships the New Flag Officer Co
Rima Das: new ambassador of ‘Share Her Journey’ Assam filmmaker Rima Das has got appointed as the official ambassador of Toronto International Film Festival (TIFF)’s ‘Share Her Journey’ campaign on 29th March 2019. This five year campaign had begun in 2017 to increase participation, skills, and opportunities for women behind and in front of the camera. Recently Rima’s movie, ‘Village Rockstars’ had made official entry into Oscars 2019 from India and her another film ‘Bulbul Can Sing’ had fetched her Dublin Film Critics Circle Jury Award in Best Director category. She has claimed many national and international awards including the ICC NE Excellence Award of Indian Chamber of Commerce. The first Indian Shipyard to deliver 100 Warships Garden Reach Shipbuilders & Engineers Limited (GRSE) has delivered its 100th Warship ‘Landing Craft Utility, L-56’, to the Indian Navy on 30th March, 2019. Rear Admiral V. K. Saxena, Chairman & Managing Director, GRSE to Lt. Cdr. Gopinath Narayanan, Commanding Officer of the Ship did this honor and with this GRSE has become the first Indian Shipyard to deliver 100 Warships to the Indian Navy, Indian Coast Guard and Mauritius Coast Guard. The new Flag Officer Commanding Eastern Fleet Rear Admiral Suraj Berry has got appointed as the Flag Officer Commanding Eastern Fleet on 30th March 2019. He has succeeded Vice Admiral Karambir Singh as the 24th chief of naval staff. He has led Eastern Fleet in several bilateral exercises viz. JIMEX-18 with the Japanese Navy, the 25th edition of SIMBEX with the Singapore Navy and INDRA-18 with the Russian Navy.