Provider Manual
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Sanford Directory
HealthPartners® Sanford Basic (Cost) HealthPartners® Sanford Active (Cost) HealthPartners® Sanford Vital (Cost) HealthPartners® Sanford Ultimate (Cost) This directory addenda provides a list of HealthPartners® Sanford network providers and pharmacies. This directory is current as of December 2020. Some network providers may have been added or removed from our network after this directory was printed. We do not guarantee that each network provider is still accepting new members. 2020 NORTH DAKOTA/SOUTH DAKOTA PROVIDER DIRECTORY - ADDENDA H2462_119077_C IR 11/2019 This document is a list of changes to the HealthPartners® Sanford network providers. Use this list to find the network providers that have had changes. Providers are organized first by the network change. The network change categories are New to the Network, No longer in the Network, Accepting New Patients, Address Changes and Phone Number Changes. After category, it is organized by provider type, then alphabetically by facility name. If you have any questions, please call Member Services at 800-233-9645 (TTY 711). Facility Name Address City, State, Zip Phone Number NEW TO THE NETWORK Primary care physicians and specialists – New to the Network Accelerate Therapy 1908 W 42nd St Ste B Sioux Falls, SD 57105 (605) 212-3446 Advanced Physical 1000 Tacoma Ave Ste Bismarck, ND 58504 (701) 751-3001 Therapy 500 Advanced Physical 4535 Northern Sky Dr Bismarck, ND 58503 (701) 354-1200 Therapy Ste 2 Advanced Physical 112 W Broadway Ave Steele, ND 58482 (701) 475-2911 Therapy Anderson-Smith -

A Bedrock Research Foundation
A Bedrock Research Foundation American Indian Health Research Conference Richard Wilsnack Holiday 2015 VOLUME 40, NUMBER 4 www.ndmedicine.org NORTH DAKOTA MEDICINE Holiday 2015 1 10 FEATURES A Bedrock Research Foundation 10 16 Researchers at the School provide the knowledge that produces well- trained healthcare professionals. American Indian Health Research Conference 16 22 Annual conference provides forum for culturally appropriate research. Richard Wilsnack 22 An unbounded intellectual curiosity that is fortified by the research partnership with his equally inquisitive spouse continues to nourish Wilsnack’s highly productive career. UNIVERSITY OF NORTH DAKOTA DEPARTMENTS SCHOOL OF MEDICINE AND HEALTH SCIENCES Dean’s Letter 4 ROBERT O. KELLEY, President, University of North Dakota News Briefs 6 JOSHUA WYNNE, Vice President for Health Affairs and Workforce 18 Dean, School of Medicine and Health Sciences Student Profile - Samantha Peterson and Rachel Engel 20 Alumni Profile - Heidi Roeber Rice, BS ’93, MD ’00 24 EDITOR Denis MacLeod Alumni Notes 26 WRITERS Alyssa Konickson, Stacy Kusler, Building Progress 28 Lonnie Laffen, Denis MacLeod, Nikki Massmann, Dave Miedema, In Memoriam 31 Juan Pedraza, Jessica Sobolik Philanthropy 32 CONTRIBUTORS Kristen Peterson Parting Shots 34 GRAPHIC DESIGN Laura Cory, John Lee, Victoria Swift PHOTOGRAPHY Nicole Pape, Wanda Weber www.ndmedicine.org WEBMASTER Eric Walter NORTH DAKOTA MEDICINE (ISSN 0888-1456; USPS 077-680) is published four times a year (March, June, September, December) by the University of North Dakota School of Medicine and Health Sciences, Room 1106, 501 N. Columbia Road Stop 9037, Grand Forks, ND 58202-9037. Periodical postage paid at Grand Forks, ND. Printed at Forum Communications Printing, Fargo, ND. -

Important Information for Providers About Sanford Health Plan
PO Box 91110 Sioux Falls, SD 57109-1110 Important Information for Phone: (877) 305-5463 Fax: (605) 328-6811 Providers about Sanford Health Plan TTY: (877) 652-1844 sanfordhealthplan.com Sanford Health Plan (Plan) asks you to take some time and review this information. The following annual notices are required to keep you informed of Sanford Health Plan operations and outcomes. Where can I find important plan information? If you have any questions…. Provider Relations Phone: (605) 328-6877 or toll free at (800) 601-5086 Email: [email protected] Care Management Phone: (888) 315-0884 Email: [email protected] Utilization Management Phone: (800) 805-7938 | TTY/TDD: (877) 652-1844 (toll-free) Fax: (605) 328-6813 NDPERS Members: Phone: (888) 315-0885 | TTY/TDD: (877) 652-1844 (toll-free) Fax: (701) 234-4547 North Dakota Medicaid Expansion Phone: (855) 276-7214 Members: Pharmacy Management Phone: (855) 305-5062 Fax: (701) 234-4568 NDPERS Members: Phone: (877) 658-9194 North Dakota Medicaid Expansion Phone: (855) 263-3547 Members: Compliance / Privacy Email: [email protected] The Utilization and Pharmacy Management Departments are available between the business hours of 8 a.m. to 5 p.m., CT, Monday through Friday (excluding holidays). For North Dakota Public Employees Retirement System (NDPERS), the Utilization and Pharmacy Management Departments are available between the business hours of 8 a.m. to 5:30 p.m. CT, Monday through Friday (excluding holidays). After business hours, you may leave a confidential -

Altru & You with Medica Fact Sheet (Accountable Care System Product)
Altru & You with Medica Fact Sheet (Accountable Care System Product) Overview Altru & You with MedicaSM is an accountable care system product offered in 14 counties in northeastern North Dakota and 6 counties in northwestern Minnesota, effective as of July 1, 2016. Altru & You providers deliver care in more than 30 communities plus provide access to several specialties via telemedicine. In Grand Forks and East Grand Forks, care is provided at 13 locations including an acute care hospital, a specialty hospital, inpatient rehabilitation hospital, various clinics, Altru Cancer Center, Altru Advanced Orthopedics, Sanny & Jerry Ryan Center for Prevention & Genetics, and Yorhom Medical Essentials. In addition, local health care providers throughout the region ensure that Medica members can get the care they need close to home. Members may see any provider in the Altru & You with Medica network without a referral. Members can also access non-network providers but may have higher deductibles and out-of pocket expenses than for in-network providers. To verify which providers are included in this product’s network, see the online provider search tool on medica.com. 2021 ID Card Example (MN) 2021 ID Card Example (ND) Altru & You with Medica Fact Sheet Page 1 of 3 Rev 11/17/2020 Available to Commercial large groups in the following counties: MN counties: . Kittson . Marshall . Pennington . Polk . Red Lake . Roseau ND counties: . Benson . Cavalier . Eddy . Grand Forks . Griggs . Nelson . Pembina . Pierce . Ramsey . Rolette . Steele . Towner . Traill . Walsh Network Hospitals . Altru Health System (Grand Forks, ND) . Cavalier County Memorial Hospital (Langdon, ND) . Cooperstown Medical Center (Cooperstown, ND) . Essentia Health Fosston (Fosston, MN) . -

Behavioral Health Quick Reference Please Call an In-Network Provider List Below for Behavioral Health Needs Assessment Services
Iowa Behavioral Health Quick Reference Please call an In-Network provider list below for behavioral health needs assessment services. LOCATION PHONE All Things New Therapy Services Inc 111 Arizona Ave NW Orange City, IA 51041 (712) 737-9444 Jeremy Koerselman, LISW Rachel Valentine, LMHC Associates for Psychiatric Services, PC 600 4th St Ste 501 Sioux City, IA 51101 (712) 234-0220 Beth Harms, LISW Patricia Whalen, LISW Collette McCullough, ARNP Philip Muller, DO Glenda DenHerder, ARNP Susan Richards, LISW Jeannie Franklin, ARNP Associates for Psychological & Therapy Services 1106 4th St Ste 205 Sioux City, IA 51101 (712) 252-1473 Aaron Baker, LMHC Melissa Schuldt, LMSW Michael Baker, PhD Avera Medical Group Spencer A Department of Spencer 116 E 11th St Ste 101 Spencer, IA 51301 (712) 264-3500 Hugh Starks, MD Kimberly Whisenant, ARNP Behavior Care Specialists, Inc. 745 10th St Ste C Rock Valley, IA 51247 (712) 454-3484 Tracy Stephens, BCBA,PhD Bethany Christian Services of the Heartland 123 Albany Ave SE Orange City, IA 51041 (712) 737-4831 Rachel Valentine, LMHC Bethesda Christian Counseling Midwest, Inc. 400 Central Ave NW Ste 300 Orange City, IA 51041 (712) 737-2635 Deon Wynia, LMHC,MA Stephanie Adams, LISW Mandi Dolieslager, LMSW,MSW William Fuller, MD Melody Becker Pullman, LMHC,MS William Huisken, LISW,MSW Sanford Health Plan Participating Providers as of June 8, 2020 1 Iowa Behavioral Health Quick Reference Please call an In-Network provider list below for behavioral health needs assessment services. LOCATION PHONE Catholic Charities -
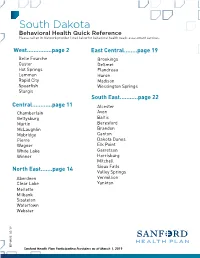
South Dakota Behavioral Health Quick Reference Please Call an In-Network Provider Listed Below for Behavioral Health Needs Assessment Services
South Dakota Behavioral Health Quick Reference Please call an In-Network provider listed below for behavioral health needs assessment services. West...............page 2 East Central........page 19 Belle Fourche Brookings Custer DeSmet Hot Springs Flandreau Lemmon Huron Rapid City Madison Spearfish Wessington Springs Sturgis South East...........page 22 Central............page 11 Alcester Chamberlain Avon Gettysburg Baltic Martin Beresford McLaughlin Brandon Mobridge Canton Pierre Dakota Dunes Wagner Elk Point White Lake Garretson Winner Harrisburg Mitchell Sioux Falls North East.......page 14 Valley Springs Aberdeen Vermillion Clear Lake Yankton Mellette Milbank Sissteton Watertown Webster 9 /1 3 HP-0985 0 Sanford Health Plan Participating Providers as of March 1, 2019 South Dakota - West Behavioral Health Quick Reference Please call an In-Network provider listed below for behavioral health needs assessment services. Abourezk Counseling Services 2020 W Omaha St Rapid City, SD 57702 Phone: (605) 863-2881 Illyani Abourezk, CAC,LLPC-MH,MS,QMHP Ardith Sand, MSW, LCSW-PIP 5202 Pinedale Circle Rapid City, SD 57702 Phone: (605) 391-3456 Ardith Sand, LCSW-PIP,MSW Awareness Counseling LLC 809 South St Ste 201 Rapid City, SD 57701 Phone: (605) 391-3482 Pamela Barickman, LPC-MH,MS,QMHP,RN Bach Counseling Services LLC 2218 Jackson Blvd Ste 13 Rapid City, SD 57702 Phone: (605) 431-4106 Mahala Bach, LPC,NCC,QMHP Behavior Care Specialists, Inc. 3820 Jackson Blvd Ste 2 Rapid City, SD 57702 Phone: (605) 791-3373 Tracy Stephens, BCBA,PhD Behavior Management -

North Dakota HEALTH INSURANCE by the NUMBERS
North Dakota HEALTH INSURANCE BY THE NUMBERS ACCESS TO INSURANCE COVERED LIVES Large Group1A 149,111 Small Group1A 60,381 Individual1A 47,190 HSA/HDHP2B 19,350 Medigap3C 52,163 Medicare Advantage4 3,659 Medicaid5D 20,334 0 25,000 50,000 75,000 100,000 125,000 150,000 175,000 200,000 Health Insurance Employment Health Insurance Coverage in North Dakota of North Dakota Residents8G 2% EMPLOYEES Health Plan Employees6 3,759 8% Insurance-Related Employees7 2,156 13% PAYROLL 67% Health Plan Employees6E Not Reported 11% Insurance-Related Employees7F $114,720,000 AVERAGE WAGE Health Plan Employees6E Not Reported Private Uninsured Medicaid Other Insurance-Related Employees7F $53,210 Medicare Data compiled by America’s Health Insurance Plans (AHIP), Center for Policy and Research, March 2019. NORTH DAKOTA Largest Health Plans by Number of Covered LivesH Blue Cross and Sanford Health 9I Aetna Blue Shield of Medica US Life Commercial Plan North Dakota Blue Cross and American 10 Aetna Blue Shield of Mutual Of Omaha UnitedHealthcare Medigap Republic North Dakota Medicare Great Plains Health Care 11 Aetna Medicare Service Corporation Humana UnitedHealthcare Advantage Advantage (HCSC) Medicaid12 Sanford Health Plan State Premium Tax Collected13J $63,558,000 Sources All data sources, labeled 1 - 13, are referenced in detail on the “Sources” page at the end of the full report, or at this link: http://www.ahip.org/2019-State-Data Notes A. Access to Insurance – Large Group, Small Group and Individual Covered Lives The U.S. Census Bureau does not report data for those states having a limited number Large group covered lives were calculated as domestic comprehensive health coverage of employers in order to maintain anonymity. -

Trauma Conference Walter Kemp, MD, Phd Forensic Pathologist Jeffrey Sather, MD When Making Your Reservation
CONFERENCE SPEAKERS Mentor Ahmeti, MD Sherrie Murphy, BSN, CEN, CPEN, CPHQ Trauma and Acute Care Surgeon Pediatric Trauma & Critical Care Coordinator Sanford Health - Fargo, ND Hennepin County Medical Center - Minneapolis, MN Johanna Askegard-Giesmann, MD Joshua Ranum, MD Pediatric Surgeon Internal Medicine Physician Sanford Health - Fargo, ND West River Regional Hospital - Hettinger, ND Kimber Boyko, MD Shoshone Richardson, MD General / Trauma Surgeon Emergency Physician Sanford Health - Bismarck, ND Essentia Health - Fargo, ND Meghan Compton, JD Denise Roerich, MSW, LICSW Chief Legal Counsel Social Worker Altru Health System - Grand Forks, ND Trinity Health - Minot, ND 19th Annual Mark Eikenberry, MD Jeffrey Sather, MD Pediatric Intensive Care / Medical Director of ECMO ETC Medical Director / State EMS Medical Director North Dakota Statewide Children's Hospitals and Clinics of Minnesota - Minneapolis, MN Trinity Health - Minot, ND / NDDOH - Bismarck, ND Sara Gebhardt, MSN, BSN Martin Schreiber, MD, FACS Assistant Professor Trauma Surgeon University of Mary - Bismarck, ND Oregon Health & Sciences University - Portland, OR Trauma William Gebhardt Ryan Smart, MD, DMD Student Oral & Maxillofacial Surgeon Bismarck, ND Essentia Health- Fargo, ND Conference Michael Hea ly, MD Steven Weiser, MD Pediatric Orthopedic Surgeon Emergency Medicine Sept. 28 - 29, 2016 Gillette Childrens Specialty Healthcare - St. Paul, MN Altru Health System - Grand Forks, ND Matthew Heberer, MD Alerus Center Surgical Resident UND School of Medicine & Health Sciences - Grand Forks, ND 1200 S 42nd St Hans Joseph, DO Grand Forks, ND Orthopedic Surgeon Altru Health System - Grand Forks, ND A block of rooms is reserved until August 27, 2016 at: Canad Inns at $94.00 + tax /night - 701-772-8404 Scott Johnson, MD Special Thank You to the Physicians Obstetrician / Chief of Surgery helping with the Chest Tube Labs Baymont Inn & Suites at $99.00 + tax/night - 701-757-2345 Essentia Health - Fargo, ND Expressway Suites at $80.10 + tax/night - 701-757-7000 Derek Kane, MD, FACS Derek Kane, MD, FACS CHI St. -

2018 Sanford Provider Directory | Healthpartners
HealthPartners® Sanford Basic (Cost) HealthPartners® Sanford Active (Cost) HealthPartners® Sanford Vital (Cost) HealthPartners® Sanford Ultimate (Cost) 2018 NORTH DAKOTA/SOUTH DAKOTA PROVIDER DIRECTORY - ADDENDA This directory addenda provides a list of HealthPartners® Sanford network providers and pharmacies. This directory is current as of December 2018. Some network providers may have been added or removed from our network after this directory was printed. We do not guarantee that each network provider is still accepting new members. H2462_107343 NM 11/2017 Sanford Directory Addenda This document is a list of changes to the HealthPartners® Sanford network providers. Use this list to find the network providers that have had changes. Providers are organized first by the network change. The network change categories are New to the Network, No longer in the Network, Address Changes and Phone Number Changes. After category, it is organized by provider type, then alphabetically by facility name. If you have any questions, please call Member Services at 800-233-9645 (TTY 711). Facility Name Address City, State, Zip Phone Number NEW TO THE NETWORK Primary care physicians and specialists – New to the Network Caring Edge OP LLC 1810 S Dorothy Ave Sioux Falls, SD 57106 (605) 356-8888 Caring Edge OP, LLC 3124 Colorado Ln Bismarck, ND 58503- (701) 751-5325 5447 Caring Edge OP, LLC 3406 Dominion St Bismarck, ND 58503- (701) 258-7489 5577 Caring Edge OP, LLC 4420 37th Ave S Fargo, ND 58104 (701) 365-4771 Davis Independent OBGYN Care 414 W 18th St -

Altru Health System Uses Telstrat WFO to Enhance Patient Services Quality
Altru Health System uses TelStrat WFO to Enhance Patient Services Quality Altru Health System is a community of over 4,000 healthcare professionals and support staff committed to serving the Grand Forks, North Dakota region for more than 100 years. The staff includes over 200 physicians and more than 75 nurse practitioners and physician PBX Environment assistants in 65+ specialties. ¥ ShoreTel Release 14.2 Through 12 Grand Forks practice locations and 12 regional practice locations Altru serves ¥ Cisco network more than 200,000 residents in northeast North Dakota and northwest Minnesota, providing ¥ 4,500 users healthcare services to meet needs of patients of all ages and levels of health. In 2015 the ¥ 150 agents system supported 494,085 clinic visits. As a member of the Mayo Clinic Care Network, Altru brings the Mayo ClinicÕs knowledge and expertise to Red River Valley. ¥ 76,000 inbound calls/week ¥ 50,000 outbound calls/week The Challenge Needs Altru Health System has long recognized the need to record telephone calls coming into the ¥ Ability to record 100% of calls healthcare delivery system via its switchboard, nursing lines and patient access. Availability of interaction recordings facilitates speedier resolution healthcare issues for both patients ¥ Comply with PCI and care providers. However, Altru Health System realized its call recording system was not and HIPAA requirements well-suited to support regional healthcare providersÕ ongoing growth. ¥ Review calls for quality and training In 2016, assisted by High Point Networks, Altru replaced their legacy recording system with SerenovaÕs TelStrat Call Recording software, with encryption for HIPAA compliance. Solution This solution will support its growing number of call-handling agents spread across the healthcare providerÕs campus that comprises the main hospital, specialty clinics, and SerenovaÕs TelStrat WFO Including: rehabilitation and counseling centers. -

Susan Berry, Director, Sanford Telemedicine, Enterprise Director of Telehealth Services, Sanford Health
BIOS Susan Berry, Director, Sanford Telemedicine, Enterprise Director of Telehealth Services, Sanford Health. In her role as Telehealth Director, Susan has responsibility for all telehealth activities for Sanford Health. She has 25 years of experience in various roles in the healthcare IT field. Susan started her career in cardiovascular services for a tertiary medical center. From there she transitioned into healthcare IT and has held roles in product development, education and training, Six Sigma and Global Product Management for GE Healthcare IT, FUJIFILM Medical Systems and now Sanford Health. Susan is a member of the American Telemedicine Association (ATA), Center for Telehealth and e-Health Law (CTeL) and sits on the Great Plains Telehealth Resource and Assistance Center Program Advisory Council (gpTRAC PAC). Susan holds a MBA degree from Colorado Technical University, a Bachelor’s degree from the University of Sioux Falls and is a registered Cardiovascular Invasive Specialist. Susan is a native of South Dakota. She enjoys spending time with family and friends at her lake cabin, reading and cooking. She currently resides in Sioux Falls, SD with her husband Christopher. Jeffrey Leichter Ph.D., L.P., born and raised in Long Beach, CA., received an undergraduate degree in biological sciences from the University of California, Irvine and a doctorate in clinical psychology from Alliant University in Los Angeles. He completed a two-year fellowship in health psychology at Michigan State University. He was director of behavioral medicine at National Rehabilitation Hospital in Washington D.C. before joining Sanford Health in 1990. He has worked for the past 27 years in a rural primary care clinic in Detroit Lakes, Minnesota where he has collaborated closely in integrated practice with family medicine, internal medicine, and OB-GYN physicians and advanced practice providers. -

Sanford Health
Adult Immunization (AI) Best Practices Learning Collaborative, Group 2: Case Study Sanford Health Sioux Falls, SD Organizational Profile Acronym Legend Sanford Health, one of the largest health systems in the United AI Collaborative: AMGA’s Adult Immunization Best States, is dedicated to the integrated delivery of health care, Practices Collaborative genomic medicine, senior care and services, global clinics, CDC: Centers for Disease Control and Prevention research and affordable insurance. Headquartered in Sioux EMR: Electronic medical record Falls, South Dakota, the organization includes 44 hospitals, HM: Health Maintenance 1,400 physicians and more than 200 Good Samaritan PCV13: Pneumococcal Conjugate Vaccine Society senior care locations in 26 states and nine countries. PPSV23: Pneumococcal Polysaccharide Vaccine Nearly $1 billion in gifts from philanthropist Denny Sanford QA: Quality assurance have transformed how Sanford Health improves the human condition. the two types of pneumococcal vaccines, and the adult Executive Summary vaccination schedule. Staff were also educated on the Every year, many people are affected by influenza and transition to a “no missed opportunities” culture. A “no missed pneumococcal disease. Although vaccines are available opportunities” culture means that vaccines are administered at to prevent these diseases, many individuals have not been all visit types—not just complete physical exams. The second vaccinated and are left unprotected. Sanford Health has been intervention utilized was distribution of reminder letters to working hard to make improvements in vaccination rates patients overdue for pneumococcal vaccination. Lastly, an for all patients. AMGA’s Adult Immunization Best Practices incentive program was instituted to provide compensation Learning Collaborative (AI Collaborative) provided an to the clinic that saw the greatest increase in pneumococcal opportunity to focus on better protecting adult patients.