Cellular and Regional Vulnerability in Frontotemporal Tauopathies
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pathologic Thr175 Tau Phosphorylation in CTE and CTE with ALS
Published Ahead of Print on January 3, 2018 as 10.1212/WNL.0000000000004899 ARTICLE OPEN ACCESS Pathologic Thr175 tau phosphorylation in CTE and CTE with ALS Alexander J. Moszczynski, PhD, Wendy Strong, BSc, Kathy Xu, MSc, Ann McKee, MD, Arthur Brown, PhD, Correspondence and Michael J. Strong, MD Dr. M.J. Strong [email protected] Neurology® 2018;90:e1-8. doi:10.1212/WNL.0000000000004899 Abstract Objective To investigate whether chronic traumatic encephalopathy (CTE) and CTE with amyotrophic lateral sclerosis (CTE-ALS) exhibit features previously observed in other tauopathies of pathologic phosphorylation of microtubule-associated protein tau at Thr175 (pThr175 tau) and Thr231 (pThr231 tau), and glycogen synthase kinase–3β (GSK3β) activation, and whether these pathologic features are a consequence of traumatic brain injury (TBI). Methods Tau isoform expression was assayed by western blot in 6 stage III CTE cases. We also used immunohistochemistry to analyze 5 cases each of CTE, CTE-ALS, and 5 controls for ex- pression of activated GSK3β, pThr175 tau, pThr231 tau, and oligomerized tau within spinal cord tissue and hippocampus. Using a rat model of moderate TBI, we assessed tau pathology and phospho-GSK3β expression at 3 months postinjury. Results CTE and CTE-ALS are characterized by the presence of all 6 tau isoforms in both soluble and insoluble tau isolates. Activated GSK3β, pThr175 tau, pThr231 tau, and oligomerized tau protein expression was observed in hippocampal neurons and spinal motor neurons. We observed tau neuronal pathology (fibrillar inclusions and axonal damage) and increased levels of pThr175 tau and activated GSK3β in moderate TBI rats. Conclusions Pathologic phosphorylation of tau at Thr175 and Thr231 and activation of GSK3β are features of the tauopathy of CTE and CTE-ALS. -

Elucidating Crosstalk Mechanisms Between Phosphorylation and O
Elucidating crosstalk mechanisms between PNAS PLUS phosphorylation and O-GlcNAcylation Aneika C. Leneya,b,c,d, Dris El Atmiouie, Wei Wua,b,c,d, Huib Ovaae, and Albert J. R. Hecka,b,c,d,1 aBiomolecular Mass Spectrometry and Proteomics, Utrecht University, 3584 CH Utrecht, The Netherlands; bBijvoet Center for Biomolecular Research, Utrecht University, 3584 CH Utrecht, The Netherlands; cUtrecht Institute for Pharmaceutical Sciences, Utrecht University, 3584 CH Utrecht, The Netherlands; dNetherlands Proteomics Centre, Utrecht University, 3584 CH Utrecht, The Netherlands; and eChemical Immunology, Leiden University Medical Centre, 2333 ZA Leiden, The Netherlands Edited by Tony Hunter, The Salk Institute for Biological Studies, La Jolla, CA, and approved July 21, 2017 (received for review December 14, 2016) Proteins can be modified by multiple posttranslational modifications from studies in which cellular stimuli were shown to increase both (PTMs), creating a PTM code that controls the function of proteins in O-GlcNAcylation and phosphorylation levels simultaneously (6, 7). space and time. Unraveling this complex PTM code is one of the great Although, many studies have demonstrated that crosstalk occurs, challenges in molecular biology. Here, using mass spectrometry-based studies that identify and colocalize both the phosphorylation and assays, we focus on the most common PTMs—phosphorylation and O-GlcNAcylation sites simultaneously on the same protein/peptide O-GlcNAcylation—and investigate how they affect each other. We are sporadic. Thus, doubt still exists as to whether on a specific demonstrate two generic crosstalk mechanisms. First, we define a protein molecule O-GlcNAcylation directly affects phosphorylation frequently occurring, very specific and stringent phosphorylation/ or vice versa. -

NIH Public Access Author Manuscript J Neuropathol Exp Neurol
NIH Public Access Author Manuscript J Neuropathol Exp Neurol. Author manuscript; available in PMC 2010 September 24. NIH-PA Author ManuscriptPublished NIH-PA Author Manuscript in final edited NIH-PA Author Manuscript form as: J Neuropathol Exp Neurol. 2009 July ; 68(7): 709±735. doi:10.1097/NEN.0b013e3181a9d503. Chronic Traumatic Encephalopathy in Athletes: Progressive Tauopathy following Repetitive Head Injury Ann C. McKee, MD1,2,3,4, Robert C. Cantu, MD3,5,6,7, Christopher J. Nowinski, AB3,5, E. Tessa Hedley-Whyte, MD8, Brandon E. Gavett, PhD1, Andrew E. Budson, MD1,4, Veronica E. Santini, MD1, Hyo-Soon Lee, MD1, Caroline A. Kubilus1,3, and Robert A. Stern, PhD1,3 1 Department of Neurology, Boston University School of Medicine, Boston, Massachusetts 2 Department of Pathology, Boston University School of Medicine, Boston, Massachusetts 3 Center for the Study of Traumatic Encephalopathy, Boston University School of Medicine, Boston, Massachusetts 4 Geriatric Research Education Clinical Center, Bedford Veterans Administration Medical Center, Bedford, Massachusetts 5 Sports Legacy Institute, Waltham, MA 6 Department of Neurosurgery, Boston University School of Medicine, Boston, Massachusetts 7 Department of Neurosurgery, Emerson Hospital, Concord, MA 8 CS Kubik Laboratory for Neuropathology, Department of Pathology, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts Abstract Since the 1920s, it has been known that the repetitive brain trauma associated with boxing may produce a progressive neurological deterioration, originally termed “dementia pugilistica” and more recently, chronic traumatic encephalopathy (CTE). We review the 47 cases of neuropathologically verified CTE recorded in the literature and document the detailed findings of CTE in 3 professional athletes: one football player and 2 boxers. -

Immune Effector Mechanisms and Designer Vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA
EXPERT REVIEW OF VACCINES https://doi.org/10.1080/14760584.2019.1674144 REVIEW How vaccines work: immune effector mechanisms and designer vaccines Stewart Sell Wadsworth Center, New York State Department of Health, Empire State Plaza, Albany, NY, USA ABSTRACT ARTICLE HISTORY Introduction: Three major advances have led to increase in length and quality of human life: Received 6 June 2019 increased food production, improved sanitation and induction of specific adaptive immune Accepted 25 September 2019 responses to infectious agents (vaccination). Which has had the most impact is subject to debate. KEYWORDS The number and variety of infections agents and the mechanisms that they have evolved to allow Vaccines; immune effector them to colonize humans remained mysterious and confusing until the last 50 years. Since then mechanisms; toxin science has developed complex and largely successful ways to immunize against many of these neutralization; receptor infections. blockade; anaphylactic Areas covered: Six specific immune defense mechanisms have been identified. neutralization, cytolytic, reactions; antibody- immune complex, anaphylactic, T-cytotoxicity, and delayed hypersensitivity. The role of each of these mediated cytolysis; immune immune effector mechanisms in immune responses induced by vaccination against specific infectious complex reactions; T-cell- mediated cytotoxicity; agents is the subject of this review. delayed hypersensitivity Expertopinion: In the past development of specific vaccines for infections agents was largely by trial and error. With an understanding of the natural history of an infection and the effective immune response to it, one can select the method of vaccination that will elicit the appropriate immune effector mechanisms (designer vaccines). These may act to prevent infection (prevention) or eliminate an established on ongoing infection (therapeutic). -

Investigation of Anti-Iglon5-Induced Neurodegenerative Changes in Human Neurons
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.27.269795; this version posted August 28, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Manuscript BioRxiv Investigation of anti-IgLON5-induced neurodegenerative changes in human neurons Mattias Gamre1,2, Matias Ryding1,2, Mette Scheller Nissen1,2,3, Anna Christine Nilsson4, Morten Meyer1,2,5, Morten Blaabjerg1,2,3,5 1Neurobiological Research, Institute of Molecular Medicine, University of Southern Denmark, Odense, Denmark. 2Department of Neurology, Odense University Hospital, Odense, Odense, Denmark 3Department of Clinical Research, Odense University Hospital, Odense, Denmark 4Department of Clinical Immunology, Odense University Hospital, Odense, Denmark 5BRIDGE – Brain Research Inter-Disciplinary Guided Excellence, Department of Clinical Research, University of Southern Denmark, Odense, Denmark Number of pages: 12 Number of figures: 4 Keywords: IgLON5, Autoimmune encephalitis, neurodegeneration, inflammation, Tau Corresponding author Professor Morten Blaabjerg, MD, PhD Department of Neurology Odense University Hospital J.B. Winsløws Vej 4 5000 Odense C Denmark Phone: (+45) 6541 2457 E-mail: [email protected] Page 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.27.269795; this version posted August 28, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. -

Aluminum Neurotoxicity — Potential Role in the Pathogenesis of Neurofibrillary Tangle Formation Daniel P
LE JOURNAL CANADIEN DES SCIENCES NEUROLOGIQUES Aluminum Neurotoxicity — Potential Role in the Pathogenesis of Neurofibrillary Tangle Formation Daniel P. Perl and William W. Pendlebury ABSTRACT: Alzheimer's disease is a progressive neurodegenerative disease characterized neuropathologically by the development of large numbers of neurofibrillary tangles in certain neuronal populations of affected brains. This paper presents a review of the available evidence which suggests that aluminum is associated with Alzheimer's disease and specifically with the development of the neurofibrillary tangle. Aluminum salts innoculated into experi mental animals produce neurofilamentous lesions which are similar, though not identical, to the neurofibrillary tangle of man. Although a few reports have suggested evidence of increased amounts of aluminum in the brains of Alzheimer's disease victims, such bulk analysis studies have been difficult to replicate. Using scanning electron microscopy with x-ray spectrometry, we have identified accumulations of aluminum in neurofibrillary tangle-bearing neurons of Alzheimer's disease. Similar accumulations have been identified in the neurofibrillary tangle-bearing neurons found in the brains of indigenous natives of Guam who suffer from parkinsonism with dementia and amyotrophic lateral sclerosis. This ongoing research still cannot ascribe a causal role of aluminum in the pathogenesis of neurofibrillary tangle formation; however, it does suggest that environmental factors may play an important part in the formation of this abnormality. RESUME: La neurotoxicity de Paluminium: son role possible dans la pathogenese de la formation des enchevetrements neurofibrillaires. La maladie d'Alzheimer est une maladie neurodegenerative progressive caracterisee au point de vue anatomo-pathologique par le developpement d'un grand nombre d'enchevetrements neurofibrillaires au sein de certaines populations de neurones dans le cerveau des sujets atteints. -

Chronic Traumatic Encephalopathy-Like Abnormalities in a Routine Neuropathology Service
J Neuropathol Exp Neurol Vol. 75, No. 12, December 2016, pp. 1145–1154 doi: 10.1093/jnen/nlw092 ORIGINAL ARTICLE Chronic Traumatic Encephalopathy-Like Abnormalities in a Routine Neuropathology Service Shawna Noy, MD, Sherry Krawitz, MD, PhD, and Marc R. Del Bigio, MD, PhD, FRCPC Downloaded from https://academic.oup.com/jnen/article-abstract/75/12/1145/2452334 by guest on 07 September 2018 sports including boxing, American football, soccer, ice Abstract hockey, wrestling and rugby, as well as in military personnel Chronic traumatic encephalopathy (CTE) has been described who have had exposure to blast or concussive injury (3–6). mainly in professional athletes and military personnel and is charac- McKeeetal(1) categorized the histological findings of CTE terized by deposition of hyperphosphorylated tau at the depths of into 4 stages. Their evidence suggests that CTE begins at the cortical sulci and around blood vessels. To assess CTE-like changes depths of cortical sulci in a perivascular distribution, and in a routine neuropathology service, we prospectively examined 111 spreads to involve widespread regions of the central nervous brains (age 18–60 years). The presence of tau-immunoreactive de- system. The pathogenesis of CTE is not well understood. posits was staged using guidelines described by others and was cor- Repetitive mild brain trauma is the postulated underlying related with the medical history. 72/111 cases were negative for stimulus (3). Tau (which is encoded by the MAPT gene) is an CTE-like changes; 34/111 were CTE stage <1; 3/111 were CTE axonal protein that promotes microtubule assembly and stabil- stage 1; and 2/111 were CTE stage 2. -

Functional Studies of Alzheimer's Disease Tau Protein
The Journal of Neuroscience, February 1993, 13(2): 508415 Functional Studies of Alzheimer’s Disease Tau Protein Qun Lu and John G. Wood Department of Anatomy and Cell Biology, Emory University School of Medicine, Atlanta, Georgia 30322 In vitroassays were used to monitor and compare the kinetic concentration at which pure tubulin assembles(Weingarten et behavior of bovine tubulin polymerization enhanced by tau al., 1975; Cleveland et al., 1977). In cultured fibroblasts, which proteins isolated from Alrheimer’s disease (AD) and nonde- do not contain endogenoustau, microinjected tau can incor- mented (ND) age-matched control brains. Tau from AD cases porate into microtubules and stabilize them against depoly- induced slower polymerization and a steady state turbidity merization conditions (Drubin and Kirschner, 1986; Lu and value approximately 50% of that stimulated by tau from con- Wood, 1991b). trol cases. Tau from the most severe AD case was least In brain, tau is largely localized in axons (Binder et al., 1985; effective at promoting polymerization. Dark-field light mi- Brion et al., 1988). However, in AD brain tau becomes an croscopy of the control samples revealed abundant micro- integral part of paired helical filaments (PHFs) in neurofibrillary tubule formation and many microtubule bundles. Microtubule tangles of neuronal cell bodies as well as dystrophic neurites assembly was observed in AD samples as well, but bundling associatedwith neuritic plaques (Brion et al., 1985; Grundke- was not obvious. These results were confirmed by negative- Iqbal et al., 1986, 1988; Kosik et al., 1986; Wood et al., 1986). stain electron microscopy. Morphological analysis showed This dislocation is accompanied by abnormal phosphorylation that AD tau-induced microtubules were longer than control (Grundke-Iqbal et al., 1986; Wood et al., 1986; Iqbal et al., microtubules. -

An Autopsy Case of Progressive Supranuclear Palsy with Incidental
Letters Discussion | This pilot study successfully explored the effect size 3. Korte J-M, Kaila T, Saari KM. Systemic bioavailability and cardiopulmonary of timolol eyedrops on migraine headaches. Several partici- effects of 0.5% timolol eyedrops. Graefes Arch Clin Exp Ophthalmol. 2002;240 (6):430-435. pants responded extremely well to the timolol. Further re- 4. Migliazzo CV, Hagan JC III. Beta blocker eyedrops for treatment of acute search is needed to determine what patient factors might pre- migraine. Mo Med. 2014;111(4):283-288. dict responsiveness to timolol. 5. Chiam PJT. Topical beta-blocker treatment for migraine. Int Ophthalmol. 2012; 32(1):85-88. Limitations. Study limitations include a small sample size, a 6. Headache Classification Committee of the International Headache Society. lack of investigator masking, and an imperfect placebo, as The international classification of headache disorders, 3rd edition (beta artificial tears tend to cause less of a burning sensation than version). https://www.ichd-3.org/wp-content/uploads/2016/08/International -Headache-Classification-III-ICHD-III-2013-Beta-1.pdf. Accessed June 1, 2016. timolol. With a half-life of 4 hours, timolol ophthalmic is unlikely to have had an association with repeated head- aches or beyond the 3-day washout period. Four 50-μL drops of timolol, 0.5%, represent 1 mg of timolol, which An Autopsy Case of Progressive Supranuclear compares with an oral prophylactic dosage of 10 to 30 mg of Palsy With Incidental ATXN2 Expansion timolol daily. Future research should aim for a target enroll- A case of multiple system atrophy with predominant parkin- ment of more than 86 participants and explore optimal dos- sonism (MSA-P) with ATXN2 (OMIM 601517) expansion was ing regimens. -
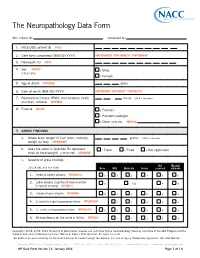
The Neuropathology Data Form
The Neuropathology Data Form ADC subject ID: Completed by: 1. MDS/UDS patient ID PTID 2. Date form completed (MM/DD/ YYYY) NPFORMMO / NPFORMDY / NPFORMYR 3. Neuropath ID NPID 4. Sex NPSEX 1 Male (CHECK ONE) 2 Female 5. Age at death NPDAGE years 6. Date of death (MM/ DD/ YYYY) NPDODMO / NPDODDY / NPDODYR 7. Postmortem interval (PMI): time between death . hours (99.9 = unknown) and brain removal NPPMIH 8. Fixative NPFIX 1 Formalin 2 Paraformaldehyde 7 Other (SPECIFY): NPFIXX 9. GROSS FINDINGS a. Whole brain weight (if half brain, multiply grams (9999 = unknown) weight by two) NPWBRWT b. Does the value in Question 9a represent 1 Fresh 2 Fixed 8 Not applicable fresh or fixed weight? (CHECK ONE) NPWBRF c. Severity of gross findings Not Missing/ (CHECK ONE BOX PER ROW) None Mild Moderate Severe assessed unknown 1. Cerebral cortex atrophy NPGRCCA 0 1 2 3 8 9 Lobar atrophy (significant frontal and/or 2. 0 1 Yes 8 9 temporal atrophy) NPGRLA 3. Hippocampus atrophy NPGRHA 0 1 2 3 8 9 4. Substantia nigra hypopigmentation NPGRSNH 1 2 3 8 9 5. L. ceruleus hypopigmentation NPGRLCH 0 1 2 3 8 9 6. Atherosclerosis (of the circle of Willis) NPAVAS 1 2 3 8 9 Copyright© 2006, 2008, 2014 University of Washington. Created and published by the Neuropathology Steering ommittee of the ADC Program and the National Alzheimer’s Coordinating Center (Walter A. Kukull, PhD, Director). All rights reserved. This publication was funded by the National Institutes of Health through the National Institute on Aging (Cooperative Agreement U01 AG016976). -

Identification of Genetic Modifiers in Hereditary Spastic Paraplegias Due to SPAST/SPG4 Mutations Livia Parodi
Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations Livia Parodi To cite this version: Livia Parodi. Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations. Human health and pathology. Sorbonne Université, 2019. English. NNT : 2019SORUS317. tel-03141229 HAL Id: tel-03141229 https://tel.archives-ouvertes.fr/tel-03141229 Submitted on 15 Feb 2021 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Sorbonne Université Institut du Cerveau et de la Moelle Épinière École Doctorale Cerveau-Cognition-Comportement Thèse de doctorat en Neurosciences Identification of genetic modifiers in Hereditary Spastic Paraplegias due to SPAST/SPG4 mutations Soutenue le 9 octobre 2019 par Livia Parodi Membres du jury : Pr Bruno Stankoff Président Pr Lesley Jones Rapporteur Dr Susanne de Bot Rapporteur Pr Christel Depienne Examinateur Pr Cyril Goizet Examinateur Pr Alexandra Durr Directeur de thèse Table of contents Abbreviations _________________________________________________________ -

And Α-Synuclein Pathology in a Case of Hereditary Spastic Paraplegia SPG7 with an Ala510val Mutation
Int. J. Mol. Sci. 2015, 16, 25050-25066; doi:10.3390/ijms161025050 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Article Abnormal Paraplegin Expression in Swollen Neurites, τ- and α-Synuclein Pathology in a Case of Hereditary Spastic Paraplegia SPG7 with an Ala510Val Mutation Dietmar R. Thal 1,2,*, Stephan Züchner 3,4, Stephan Gierer 5, Claudia Schulte 6,7, Ludger Schöls 6,7, Rebecca Schüle 3,6,7,† and Matthis Synofzik 5,6,†,* 1 Laboratory of Neuropathology—Institute of Pathology, Center of Clinical Research, University of Ulm, Helmholtzstraße 8/1, D-89081 Ulm, Germany 2 Department of Neuroscience, Katholieke Universiteit Leuven, B-3000 Leuven, Belgium 3 Dr. John T. Macdonald Foundation Department of Human Genetics University of Miami Miller School of Medicine, Miami, FL 33136, USA; E-Mails: [email protected] (S.Z.); [email protected] (R.S.) 4 John P. Hussman Institute for Human Genomics, University of Miami Miller School of Medicine, Miami, FL 33136, USA 5 Outpatient Praxis for Neurology, D-89407 Dillingen, Germany; E-Mail: [email protected] 6 Department of Neurodegenerative Diseases, Hertie-Institute for Clinical Brain Research, Hoppe-Seyler-Strasse 3, University of Tübingen, 72077 Tübingen, Germany; E-Mails: [email protected] (C.S.); [email protected] (L.S.) 7 German Research Center for Neurodegenerative Diseases (DZNE), University of Tübingen, 72076 Tuebingen, Germany † These authors contributed equally to this work. * Authors to whom correspondence should be addressed; E-Mails: [email protected] (D.R.T.); [email protected] (M.S.); Tel.: +32-16-3-44047 (D.R.T); +49-7071-298-2060 (M.S.); Fax: +32-16-3-36548 (D.R.T); +49-7071-2925-0001 (M.S.).