War Neurosurgery: Triumphs and Transportation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A History of the Society of British Neurological Surgeons 1926 to Circa 1990
A History of the Society of British Neurological Surgeons 1926 to circa 1990 TT King TT King A History of the Society of British Neurological Surgeons, 1926 to circa 1990 TT King Society Archivist 1 A History of the Society of British Neurological Surgeons, 1926 to circa 1990 © 2017 The Society of British Neurological Surgeons First edition printed in 2017 in the United Kingdom. No part of this publication may be reproduced, stored in a retrieval sys- tem or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior written permis- sion of The Society of British Neurological Surgeons. While every effort has been made to ensure the accuracy of the infor- mation contained in this publication, no guarantee can be given that all errors and omissions have been excluded. No responsibility for loss oc- casioned to any person acting or refraining from action as a result of the material in this publication can be accepted by The Society of British Neurological Surgeons or the author. Published by The Society of British Neurological Surgeons 35–43 Lincoln’s Inn Fields London WC2A 3PE www.sbns.org.uk Printed in the United Kingdom by Latimer Trend EDIT, DESIGN AND TYPESET Polymath Publishing www.polymathpubs.co.uk 2 The author wishes to express his gratitude to Philip van Hille and Matthew Whitaker of Polymath Publishing for bringing this to publication and to the British Orthopaedic Association for their help. 3 A History of the Society of British Neurological Surgeons 4 Contents Foreword -

Stereotactic Neurosurgery in the United Kingdom: the Hundred Years from Horsley to Hariz
LEGACY STEREOTACTIC NEUROSURGERY IN THE UNITED KINGDOM: THE HUNDRED YEARS FROM HORSLEY TO HARIZ Erlick A.C. Pereira, M.A. THE HISTORY OF stereotactic neurosurgery in the United Kingdom of Great Britain Oxford Functional Neurosurgery, and Northern Ireland is reviewed. Horsley and Clarke’s primate stereotaxy at the turn Nuffield Department of Surgery, of the 20th century and events surrounding it are described, including Mussen’s devel- University of Oxford, and Department of Neurological Surgery, opment of a human version of the apparatus. Stereotactic surgery after the Second The John Radcliffe Hospital, World War is reviewed, with an emphasis on the pioneering work of Gillingham, Oxford, England Hitchcock, Knight, and Watkins and the contributions from Bennett, Gleave, Hughes, Johnson, McKissock, McCaul, and Dutton after the influences of Dott, Cairns, and Alexander L. Green, M.D. Jefferson. Forster’s introduction of gamma knife radiosurgery is summarized, as is the Oxford Functional Neurosurgery, Nuffield Department of Surgery, application of computed tomography by Hounsfield and Ambrose. Contemporary University of Oxford, and contributions to the present day from Bartlett, Richardson, Miles, Thomas, Gill, Aziz, Department of Neurological Surgery, Hariz, and others are summarized. The current status of British stereotactic neuro- The John Radcliffe Hospital, Oxford, England surgery is discussed. KEY WORDS: Atlas, Computed tomography, Functional neurosurgery, History, Radiosurgery, Stereotactic Dipankar Nandi, Ph.D. frame, Stereotactic neurosurgery Imperial College London, and Charing Cross Hospital, Neurosurgery 63:594–607, 2008 DOI: 10.1227/01.NEU.0000316854.29571.40 www.neurosurgery-online.com London, England Tipu Z. Aziz, M.D., D.M.Sc. Pigmaei gigantum humeris impositi Sir Victor Alexander Haden Horsley (1857– Oxford Functional Neurosurgery, plusquam ipsi gigantes vident 1916) (Fig. -
Compassion and Courage
Compassion and courage Australian doctors and dentists in the Great War Medical History Museum, University of Melbourne War has long brought about great change and discovery in medicine and dentistry, due mainly to necessity and the urgency and severity of the injuries, disease and other hardships confronting patients and practitioners. Much of this innovation has taken place in the field, in makeshift hospitals, under conditions of poor Compassion hygiene and with inadequate equipment and supplies. During World War I, servicemen lived in appalling conditions in the trenches and were and subjected to the effects of horrific new weapons courage such as mustard gas. Doctors and dentists fought a courageous battle against the havoc caused by AUSTRALIAN DOCTORS AND DENTISTS war wounds, poor sanitation and disease. IN THE REAT AR Compassion and courage: Australian doctors G W and dentists in the Great War explores the physical injury, disease, chemical warfare and psychological trauma of World War I, the personnel involved and the resulting medical and dental breakthroughs. The book and exhibition draw upon the museums, archives and library of the University of Melbourne, as well as public and private collections in Australia and internationally, Edited by and bring together the research of historians, doctors, dentists, curators and other experts. Jacqueline Healy Front cover (left to right): Lafayette-Sarony, Sir James Barrett, 1919; cat. 247: Yvonne Rosetti, Captain Arthur Poole Lawrence, 1919; cat. 43: [Algernon] Darge, Dr Gordon Clunes McKay Mathison, 1914. Medical History Museum Back cover: cat. 19: Memorial plaque for Captain Melville Rule Hughes, 1922. University of Melbourne Inside front cover: cat. -

Lawrence of Arabia, Sir Hugh Cairns, and the Origin of Motorcycle Helmets
LEGACIES Lawrence of Arabia, Sir Hugh Cairns, and the Origin of Motorcycle Helmets Nicholas F. Maartens, F.R.C.S.(SN), Andrew D. Wills, M.R.C.S., Christopher B.T. Adams, M.A., M.Ch., F.R.C.S. Department of Neurological Surgery, The Radcliffe Infirmary, Oxford, England WHEN COLONEL T.E. LAWRENCE (“Lawrence of Arabia”) was fatally injured in a motorcycle accident in May 1935, one of the several doctors attending him was a young neurosurgeon, Hugh Cairns. He was moved by the tragedy in a way that was to have far-reaching consequences. At the beginning of the Second World War, he highlighted the unnecessary loss of life among army motorcycle dispatch riders as a result of head injuries. His research concluded that the adoption of crash helmets as standard by both military and civilian motorcyclists would result in consid- erable saving of life. It was 32 years later, however, that motorcycle crash helmets were made compulsory in the United Kingdom. As a consequence of treating T.E. Lawrence and through his research at Oxford, Sir Hugh Cairns’ work largely pioneered legislation for protective headgear by motorcyclists and subsequently in the workplace and for many sports worldwide. Over subsequent decades, this has saved countless lives. (Neurosurgery 50:176–180, 2002) Key words: Head injury, Hugh Cairns, Lawrence of Arabia, Motorcycle helmets raumatic injuries are a major worldwide public health T.E. Lawrence concern and remain the leading cause of death in chil- Colonel Thomas Edward Lawrence, famous by the pseud- dren and adults under 45 years. As a consequence, T onym “Lawrence of Arabia,” was one of the most romantic 142,000 lives are lost and 62 million people seek medical and enigmatic figures to emerge from the First World War. -

Articles About Sir Hugh Cairns Chalif, J. I., Gillies, M. J., Magdum, S. A., Aziz, T. P., & Pereira, E. A. C. (2013). Everyt
Articles about Sir Hugh Cairns Chalif, J. I., Gillies, M. J., Magdum, S. A., Aziz, T. P., & Pereira, E. A. C. (2013). Everything to gain: Sir Hugh Cairns' Treatment of Central Nervous System Infection at Oxford and Abroad. Neurosurgery, 72(2), 135-42. DOI: 10.1227/NEU.0b013e31827b9fae Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23149954 Johnson, R. D., & Sainsbury, W. (2012). The "combined eye" of Surgeon and Artist: Evaluation of the Artists who Illustrated for Cushing, Dandy and Cairns. Journal of Clinical Neuroscience: Official Journal of the Neurosurgical Society of Australasis, 19(1), 34-8. DOI: 10.1016/j.jocn.2011.03.042 Retrieved from http://www.sciencedirect.com/science/article/pii/S0967586811004395 Nuffield Department of Surgical Sciences. (2011). Sir Hugh Cairns: Head of the Nuffield Department of Surgery 1937-1952. Retrieved from http://www.nds.ox.ac.uk/about-us/our-history/sir-hugh-cairns Ladgrove, P. (2010, February 8). Local legend - Sir Hugh Cairns. Retrieved from http://www.abc.net.au/local/stories/2010/02/08/2813284.htm Walker, N. M. (2008). Hugh Cairns--Neurosurgical Innovator. Journal of the Royal Army Medical Corps, 154(3), 146–8. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/19202816 Powell, M. (2007). Re: Hugh Cairns and the Origin of British Neurosurgery. British Journal of Neurosurgery, 21(4), 421. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/17676469 Tailor, J., & Handa, A. (2007). Hugh Cairns and the Origin of British Neurosurgery. British Journal of Neurosurgery, 21(2), 190–6. DOI: doi:10.1080/02688690701317193 Retrieved from http://informahealthcare.com/doi/abs/10.1080/02688690701317193 Hughes, J. -

Dentistry and the British Army: 1661 to 1921
Military dentistry GENErAL Dentistry and the British Army: 1661 to 1921 Quentin Anderson1 Key points Provides an overview of dentistry in Britain and Provides an overview of the concerns of the dental Illustrates some of the measures taken to provide its relation to the British Army from 1661 to 1921. profession over the lack of dedicated dental dental care to the Army in the twentieth century provision for the Army from the latter half of the before 1921 and the formation of the Army nineteenth century. Dental Corps. Abstract Between 1661 and 1921, Britain witnessed signifcant changes in the prevalence of dental caries and its treatment. This period saw the formation of the standing British Army and its changing oral health needs. This paper seeks to identify these changes in the Army and its dental needs, and place them in the context of the changing disease prevalence and dental advances of the time. The rapidly changing military and oral health landscapes of the late nineteenth century and early twentieth century bring recognition of the Army’s growing dental problems. It is not, however, without years of campaigning by members of the profession, huge dental morbidity rates on campaign and the outbreak of a global confict that the War Ofce resource a solution. This culminates in 1921 with, for the frst time in 260 years, the establishment of a professional Corps within the Army for the dental care of its soldiers; the Army Dental Corps is formed. Introduction Seventeenth century site; caries at contact areas was rare. In the seventeenth century, however, the overall This paper sets out to illustrate the links At the Restoration in 1660, Britain had three prevalence increased, including the frequency between dentistry and the British Army over armies:1 the Army raised by Charles II in of lesions at contact areas and in occlusal the 260 years between the Royal Warrant exile, the Dunkirk garrison and the main fssures.3 In contrast, it is suggested by Kerr of Charles II establishing today’s Army Commonwealth army. -

Memories of Hugh Cairns* by Sir Geoffrey Jefferson
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.22.3.155 on 1 August 1959. Downloaded from J. Neurol. Neurosurg. Psychiat., 1959, 22, 155. MEMORIES OF HUGH CAIRNS* BY SIR GEOFFREY JEFFERSON Hugh Cairns was born at Port Pirie in South whom all went for advice, She had natural talents Australia on June 26, 1896. That is the starting and a zest for life; she was one to whom everyone in point, but some enrichment should come from a the village went with their troubles. Perhaps from sketch of his early days and his Australian back- her he inherited his love of music, which she taught, ground. To be born of sound, if humble, stock but there was also his father with his violin playing. under the high and wide Australian skies is as Hugh inherited something else from his father, a fine a beginning as a perfectionist trait in man could desire. His manual skills. The father, William Cairns, son was fortunate to threatened with tuber- have fused into his culosis, had sailed out character so much of from Scotland on medi- the best qualities of guest. Protected by copyright. cal advice. At Port his parents. I have had Pirie he had found the pleasure of visiting work in timber con- Riverton, a quiet place struction for the load- indeed, basking and ing of ships, for this often baking in the was the port of ship- brilliant sun and heat ment from the smelting of South Australia. I plant of the great saw the little primary Broken Hill Proprie- school and met, by tory, Australia's chief request, two or three up-country mining area people who had been and today its largest Hugh's school fellows. -
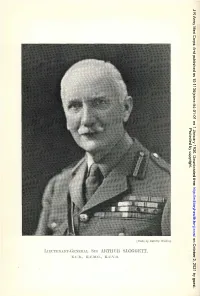
Lmc'renakt-Geciehal SIR Artiluh SLOGGETT, K .N.B., K.C.1-J.G., K.E.V.O
J R Army Med Corps: first published as 10.1136/jramc-54-01-01 on 1 January 1930. Downloaded from Protected by copyright. http://militaryhealth.bmj.com/ on October 2, 2021 by guest. [Photo hy Dorcth?/ WtldiJlg LmC'rENAKT-GECiEHAL SIR ARTIlUH SLOGGETT, K .n.B., K.C.1-J.G., K.e.v.o. J R Army Med Corps: first published as 10.1136/jramc-54-01-01 on 1 January 1930. Downloaded from VOL. LIV. JANUARY, 1930. No. 1. Authors are alone responsible for the statements made and the opinions expressed in their papers. ~tlurnal of tb' ~bituar\? LIEUTENANT-GENERAL SIR ARTHUR SLOGGETT, K.C.B., Protected by copyright. K.C.M.G., K.C.V.O. SIR ARl'HUR SLOGGEl'l' was the son of Inspector-General W. H. Sloggett, R.N., and was born at Stoke Damerel, Devon, on November 24, 1857. He was educated' at King's College, London, of which he was subsequently elected a Fellow. He obtained the M.R.C.S.England and L.R.C.P.Edinburgh in 1880, and on February 5, 1881, was commissioned as Surgeon in the Medical Staff. In his batch were several men who afterwards attained distinction as administrators, the most eminent among them being the late Sir William Babtie. Sir Arthur Sloggett will be chiefly remembered as a wise administrator, his savoir-faire, knowledge of the world and of men, enabled him to succeed where other men, though http://militaryhealth.bmj.com/ well versed in Regulations, would have failed. Sir Arthur saw much active service ana was senior medical officer with British troops in' the Dongola expedition, 1896; he was mentioned in dispatches, received the Egyptian medal with two clasps, the Order of the Osmanieh and was promoted Surgeon Lieutenant-Colonel. -

Raising Professional Confidence: the Influence of the Anglo-Boer War (1899 – 1902) on the Development and Recognition of Nursing As a Profession
Raising professional confidence: The influence of the Anglo-Boer War (1899 – 1902) on the development and recognition of nursing as a profession A thesis submitted to The University of Manchester for the degree of Doctor of Philosophy in Nursing in the Faculty of Medical and Human Sciences. 2013 Charlotte Dale School of Nursing, Midwifery and Social Work 2 Abstract ........................................................................................................................................................ 5 Declaration ........................................................................................................................................................... 6 Copyright Statement ......................................................................................................................................... 7 Acknowledgements ........................................................................................................................................... 8 The Author ............................................................................................................................................................ 9 Introduction ....................................................................................................................................................... 10 Chapter One ........................................................................................................................................................ 17 Nursing, War and the late Nineteenth Century -

Musical Performance in the Canadian Military
MUSICAL PERFORMANCE IN THE CANADIAN MILITARY: A PRELIMINARY ANALYSIS OF AN INSTITUTION by Lucie Alaimo A thesis submitted to the Faculty of Graduate Studies and Research in partial fulfillment of the requirements for the degree of Master of Arts in Music and Culture Carleton University Ottawa, Ontario August 15, 2011 2011, Lucie Alaimo Library and Archives Bibliotheque et 1*1 Canada Archives Canada Published Heritage Direction du Branch Patrimoine de I'edition 395 Wellington Street 395, rue Wellington OttawaONK1A0N4 OttawaONK1A0N4 Canada Canada Your file Votre rGf&rence ISBN: 978-0-494-83142-7 Our file Notre reference ISBN: 978-0-494-83142-7 NOTICE: AVIS: The author has granted a non L'auteur a accorde une licence non exclusive exclusive license allowing Library and permettant a la Bibliotheque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par telecommunication ou par I'lnternet, preter, telecommunication or on the Internet, distribuer et vendre des theses partout dans le loan, distribute and sell theses monde, a des fins commerciales ou autres, sur worldwide, for commercial or non support microforme, papier, electronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriete du droit d'auteur ownership and moral rights in this et des droits moraux qui protege cette these. Ni thesis. Neither the thesis nor la these ni des extraits substantiels de celle-ci substantial extracts from it may be ne doivent etre imprimes ou autrement printed or otherwise reproduced reproduits sans son autorisation. -

A Brief History of Sir Hugh Cairns and His Helmet Creation Breve História Sobre Sir Hugh Cairns E Sua Criação Do Capacete
Original A Brief History of Sir Hugh Cairns and His Helmet Creation Breve História sobre Sir Hugh Cairns e Sua Criação do Capacete Lara Mariana Rosa1 Carlos Umberto Pereira2 Nicollas Nunes Rabelo1,3 ABSTRACT Introduction: Sir Hugh Cairns was an Austrian physician who contributed much to neurology and neurosurgical practices. He created the anti-impact helmet for motorcyclists, which led to a significant reduction in mortality due to head injury. Besides, he performed tests and antibiotic treatments on neurological infections. He has made many publications on neurosurgical techniques that are used to this day. Method: This article discusses his biography and its several discoveries and contribution to medicine and society.Conclusion: Hugh Cairns was the inventor of the anti-impact helmet responsible for reducing head injuries from motorcycle accidents. He was a founder of the neurosurgery specialty at Oxford University. His surgical techniques and studies are widely used in surgical and student practices nowadays. Keywords: Hugh Cairns; Helmet; Biography; Neurosurgery; Historical review; British Neurosurgery RESUMO Introdução: Sir Hugh Cairns foi um médico austríaco que contribuiu muito para a neurologia e práticas neurocirúrgicas. Foi responsável pela criação do capacete anti-impacto para motociclistas, o que levou à significativa redução da mortalidade por traumatismo craniano. Além disso, executou testes e tratamentos antibióticos em infecções neurológicas. Realizou muitas publicações sobre técnicas neurocirúrgicas que são utilizadas até os dias atuais. Método: Este artigo discorre sobre sua biografia e suas respectivas descobertas e contribuição à medicina e sociedade. Conclusão: Hugh Cairns foi o inventor do capacete anti-impacto responsável pela redução de ferimentos craniais em acidentes motociclísticos. -

Chapter 1 12 13 the Birth of the Wfns
11 the birth of the wfns 1 The Birth of the World Federation of Neurosurgical Societies A. Earl Walker † and H. August van Alphen chapter 1 12 13 the birth of the wfns Birth of the Federation Modern neurosurgery can be considered as dating from the late nineteenth/early twentieth century. With steady development over subsequent decades, its posi- tion as an independent medical discipline was secured in the United States by the beginning of the Second World War. In many European countries, however, neu- rosurgery remained under the control of neurologists and sometimes also general surgeons, which inevitably led to conflicts and a demand for the emancipation of neurosurgery as a separate discipline. This situation was reflected in the way the International Neurological Congresses were organized, neurological subspecialties such as neuropathology, clinical neuro- physiology and neurosurgery being subsumed from the beginning. The first Inter- national Neurological Congress was held at the Municipal Casino in Berne from 31st August until 3rd September 1931, as a result of a generous initiative by the American Neurological Association. It was the first time since the World War of 1914-1918 that neurologists from Germany, France and England, as well as from other countries, had found it possible to have a joint meeting, and it proved to be a gathering little marred by politics or the old animosities of war. At that time in Ger- many, where neurology was born out of psychiatry, the neurologists still formed a joint body with the psychiatrists in the Gesellschaft Deutscher Nervenärzte and neurology was still not recognized as a separate discipline.