Community Health Needs Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fy 2020-2021 All Funds Biennial Budget
FY 2020-2021 ALL FUNDS BIENNIAL BUDGET CINCINNATI, OHIO VOLUME I: APPROVED OPERATING BUDGET City of Cincinnati - Approved FY 2017 Budget UpdateCity of Cincinnati - Approved FY 2017 Budget Update Approved Fiscal Years 2020-2021 All Funds Biennial Operating Budget Mayor John Cranley Vice-Mayor Christopher Smitherman Members of City Council Tamaya Dennard Greg Landsman David Mann Amy Murray Jeff Pastor Chris Seelbach P. G. Sittenfeld Wendell Young City Administration Patrick A. Duhaney, City Manager Christopher A. Bigham, Assistant City Manager John Juech, Assistant City Manager Sheryl Long, Assistant City Manager Karen Alder, Interim Finance Director Nicole Lee, Interim Deputy Finance Director &LWL]HQVRI&LQFLQQDWL &LW\&RQWUDFWXDO%RDUGV %RDUGVDQG&RPPLVVLRQ 0D\RU &LW\&RXQFLO 'HSDUWPHQWV Southwest Ohio Regional Transit Authority (SORTA) +XPDQ5HODWLRQV Board of Health &LW\0DQDJHU %XGJHW (YDOXDWLRQ (QYLURQPHQW 6XVWDLQDELOLW\ ,QWHUQDO$XGLW 3HUIRUPDQFH 'DWD$QDO\WLFV Park Board &RPPXQLFDWLRQV (PHUJHQF\&RPPXQLFDWLRQV&HQWHU Recreation Commission Fire Department Public Services Department Police Department Law Department Retirement Human Resources Department Community & Economic Development Department Transportation & Engineering Department Finance Department Enterprise Technology Solutions Greater Cincinnati Water Works Sewers Stormwater Citizen Complaint Authority Buildings & Inspections Economic Inclusion City Planning Department Enterprise Services Convention Center Parking Systems City Manager’s Office Office of Budget and Evaluation 801 Plum -

Trauma Centers
Updated: 5/5/2021 TRAUMA CENTERS Location Level EMS Adult Pediatric HOSPITAL CITY COUNTY Status Expires Visit Date Region Level Level Akron Children's Hospital Akron Summit 5 ACS 9/10/2022 2 Atrium Medical Center Franklin Butler 6 ACS 11/6/2022 3 Aultman Hospital Canton Stark 5 ACS 10/24/2021 6/4/2021 V 2 Bethesda North Cincinnati Hamilton 6 ACS 6/9/2022 3 Blanchard Valley Hospital Findlay Hancock 1 ACS 1/15/2024 3 Cincinnati Children's Hospital Medical Center Cincinnati Hamilton 6 ACS 1/23/2022 1 Cleveland Clinic Akron General Akron Summit 5 ACS 4/17/2022 1 Cleveland Clinic Fairview Hospital Cleveland Cuyahoga 2 ACS 3/9/2022 2 Cleveland Clinic Hillcrest Hospital Mayfield Heights Cuyahoga 2 ACS 12/9/2021 2 Dayton Children's Hospital Dayton Montgomery 3 ACS 2/12/2024 1 Firelands Regional Medical Center Sandusky Erie 1 ACS 2/23/2023 3 Fisher-Titus Medical Center Norwalk Huron 1 ACS 11/23/2022 3 Genesis HealthCare System Zanesville Muskingum 8 ACS 10/6/2024 3 Grandview Medical Center Dayton Montgomery 3 ACS 10/26/2022 3 Kettering Health Network Fort Hamilton Hospital Hamilton Butler 6 Ohio-18 8/24/2022 *3* Kettering Health Network Soin Medical Center Beavercreek Greene 3 ACS 11/13/2023 3 Kettering Medical Center Kettering Montgomery 3 ACS 1/11/2023 2 Lima Memorial Hospital Lima Allen 1 ACS 5/13/2021 5/4-5/2021 V 2 Marietta Memorial Hospital Marietta Washington 8 ACS 11/20/2022 3 Mercy Health St. Charles Hospital Toledo Lucas 1 ACS 12/8/2022 3 Mercy Health St. -

Allen Ashland Ashtabula Athens Auglaize Belmont Butler Clark Clinton Columbiana Crawford Cuyahoga Darke Defiance Delaware Erie F
Central Paternity Registry | Birthing Facilities Directory ALLEN CLARK PROMEDICA DEFIANCE REGIONAL BLANCHARD VALLEY HOSPITAL – SPRINGFIELD REGIONAL MEDICAL CENTER BLUFFTON CAMPUS MEDICAL CENTER 1200 RALSTON AVENUE 139 GARAU STREET 100 MEDICAL CENTER DRIVE DEFIANCE, OH 43512 BLUFFTON, OH 45817 SPRINGFIELD, OH 45504 DELAWARE LIMA MEMORIAL HOSPITAL CLINTON GRADY MEMORIAL HOSPITAL 1001 BELLEFONTAINE AVENUE CLINTON MEMORIAL HOSPITAL 561 WEST CENTRAL AVENUE LIMA, OH 45804 610 WEST MAIN STREET DELAWARE, OH 43015 WILMINGTON, OH 45177 ST RITA'S MEDICAL CENTER ERIE 730 WEST MARKET STREET COLUMBIANA FIRELANDS COMMUNITY HOSPITAL LIMA, OH 45801 1101 DECATUR ST SALEM REGIONAL MEDICAL CENTER 1995 EAST STATE STREET SANDUSKY, OH 44870 ASHLAND SALEM, OH 44460 UNIVERSITY HOSPITALS FAIRFIELD SAMARITAN MEDICAL CENTER FAIRFIELD MEDICAL CENTER 1025 CENTER STREET CRAWFORD GALION COMMUNITY HOSPITAL 401 NORTH EWING STREET ASHLAND, OH 44805 LANCASTER,OH 43130 269 PORTLAND WAY SOUTH GALION, OH 44833 ASHTABULA FRANKLIN ASHTABULA COUNTY CUYAHOGA DOCTORS HOSPITAL WEST MEDICAL CENTER 5100 WEST BROAD STREET 2420 LAKE AVENUE FAIRVIEW HEALTH SYSTEM 18101 LORAIN AVENUE COLUMBUS, OH 43228 ASHTABULA, OH 44004 CLEVELAND, OH 44111 DUBLIN METHODIST HOSPITAL ATHENS MERIDIA HILLCREST HOSPITAL 7500 HOSPITAL DRIVE O'BLENESS MEMORIAL HOSPITAL 6780 MAYFIELD ROAD DUBLIN, OH 43016 55 HOSPITAL DRIVE MAYFIELD HEIGHTS, OH 44124 ATHENS, OH 45701 GRANT MEDICAL CENTER METROHEALTH MEDICAL CENTER 111 SOUTH GRANT AVENUE AUGLAIZE 2500 METROHEALTH DRIVE COLUMBUS, OH 43215 ST MARY'S JOINT TOWNSHIP CLEVELAND, OH 44109 DISTRICT MOUNT CARMEL EAST MEMORIAL HOSPITAL SOUTHWEST GENERAL 6001 EAST BROAD STREET 200 ST. CLAIR STREET HEALTH CENTER COLUMBUS, OH 43213 SAINT MARYS, OH 45885 18697 BAGLEY ROAD MIDDLEBURG HEIGHTS, OH 44130 OHIO STATE UNIVERSITY MEDICAL BELMONT CENTER ST. -
Community Resource Guide for Patients and Families Dear Patient
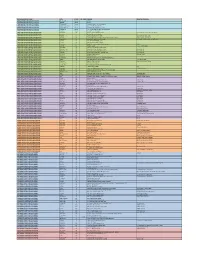
Community Resource Guide for Patients and Families Dear Patient, The Christ Hospital would like to thank you for making us your preferred health care provider. This community resource guide is for you to access the care and services you may need once you have been discharged from the Christ Hospital. In order to better serve all of our patients, the resources included in this guide are from all over the Tri-state area. If you find an error in this booklet, please notify Kevin Drummond (editor) at 513-263-9208. Thank you for allowing us to serve you. We hope we have completed our mission: “To provide the finest patient experience and improve the health of our community.” Sincerely, The Christ Hospital Health Network Last Updated 12/2020 TABLE OF CONTENTS The Christ Hospital Helpful Numbers 4 Palliative Care & Hospice 48 The Christ Hospital 5 Parenting Services and Support 50 Clinics 5 Childcare 50 Imaging 5 Parenting 50 Lab Services 6 Help Me Grow 50 Every Child Succeeds 50 Advocacy Resources 7 Post Partum/Loss Support 51 Alcohol & Other Addiction Information 8 Pharmacies with Delivery 51 Education/Advocacy/Referrals 8 Inpatient Treatment 8 Pregnancy Counseling & Services 52 Medication Assisted Treatment 10 Outpatient Treatment 14 Prescription Assistance 53 Residential and Sober Living Programs 17 Psychiatric and Crisis Hotlines 54 Addiction Support 20 Alternatives to Alcoholics Anonymous AA) Services for Seniors 54 and Narcotics Anonymous (NA) 20 Adult Day Programs 54 Family Support for Addicts 20 Driving Assessments 55 Elder Law 55 Baby -
Participants List Through April 2019
REGIONAL GROUP NAME CITY STATE ZIP CODE CENTER HEALTH SYSTEM(s) CANADIAN VASCULAR QUALITY INITIATIVE Montreal, QC Canada CHUM CANADIAN VASCULAR QUALITY INITIATIVE Gatineau Canada CISSSO CANADIAN VASCULAR QUALITY INITIATIVE Edmonton, AB Canada Covenant Health - Grey Nuns Hospital CANADIAN VASCULAR QUALITY INITIATIVE Kentville, Nova Scotia Canada Nova Scotia Health Authority CANADIAN VASCULAR QUALITY INITIATIVE Toronto, Ontario Canada Sunnybrook Health Sciences Centre CANADIAN VASCULAR QUALITY INITIATIVE Thunder Bay Canada Thunder Bay ReGional Health Sciences Centre CANADIAN VASCULAR QUALITY INITIATIVE Toronto Canada Toronto General Hospital CAROLINAS VASCULAR QUALITY GROUP (CVQG) BurlinGton NC Alamance ReGional Medical Center Cone Health System; Carolinas Healthcare CAROLINAS VASCULAR QUALITY GROUP (CVQG) louidiana SC Beaufort Memorial Hospital CAROLINAS VASCULAR QUALITY GROUP (CVQG) Pinveille NC Carolinas Healthcare - Pineville Carolinas Healthcare System CAROLINAS VASCULAR QUALITY GROUP (CVQG) Charlotte NC Carolinas Healthcare System- SanGer Heart & Vascular Institute Carolinas Healthcare System CAROLINAS VASCULAR QUALITY GROUP (CVQG) Greensboro NC Cone Health Heart & Vascular Center Cone Health System; Carolinas Healthcare CAROLINAS VASCULAR QUALITY GROUP (CVQG) Durham NC Duke University Medical Center CAROLINAS VASCULAR QUALITY GROUP (CVQG) Florence SC McLeod ReGional Medical Center CAROLINAS VASCULAR QUALITY GROUP (CVQG) Charleston SC Medical University of South Carolina Hospital MUHA CAROLINAS VASCULAR QUALITY GROUP (CVQG) Asheville -

Ohio Department of Heath Recognized Stroke
Ohio Department of Health Hospital Stroke Level Recognition ‐ Revised 4/07/2021 Supplemental Distinction AHR Hospital Name Hospital Address City County State Zip Code Stroke Level Accrediting Organization (Only Primary Stroke Centers) 1276 Akron General Medical Center 1 Akron General Avenue Akron Summit OH 44307 Thrombectomy Capable Stroke Center The Joint Commission None 1106 Ashtabula County Medical Center 2420 Lake Ave. Ashtabula Ashtabula OH 44004 Primary Stroke Center The Joint Commission None 1116 Atrium Medical Center One Medical Center Drive Franklin Warren OH 43560 Primary Stroke Center The Joint Commission None 1270 Aultman Health Foundation 2600 Sixth Street, SW Canton Stark OH 44710 Primary Stroke Center The Joint Commission None 1178 Bay Park Community Hospital 2801 Bay Park Drive Oregon Lucas OH 43616 Primary Stroke Center The Joint Commission None 1024 Bethesda North Hospital 10500 Montgomery Road Cincinnati Hamilton OH 45242 Primary Stroke Center The Joint Commission None 1101 Blanchard Valley Reg. Hlth Ctr‐Bluf 139 Garau Street Bluffton Allen OH 45817 Acute Stroke Ready Hospital The Joint Commission N/A 1194 Blanchard Valley Regional Hlth Ctr 1900 S. Main St. Findlay Hancock OH 45840 Primary Stroke Center The Joint Commission N/A 1187 Christ Hospital 2139 Auburn Avenue Cincinnati Hamilton OH 45219 Primary Stroke Center The Joint Commission None 1531 Cleveland Clinic Avon Hospital 33300 Cleveland Clinic Blvd. Avon Lorain OH 44011 Primary Stroke Center The Joint Commission None 1151 Cleveland Clinic Foundation 9500 Euclid Avenue Cleveland Cuyahoga OH 44195 Comprehensive Stroke Center The Joint Commission N/A 1285 Cleveland Clinic Union Hospital 659 Boulevard St Dover Tuscarawas OH 44622 Primary Stroke Center The Joint Commission None 1494 Diley Ridge Medical Center 7911 Diley Road Canal Winchester Fairfield OH 43701 Acute Stroke Ready Hospital The Joint Commission N/A 1015 Doctor's Hospital 5100 West Broad St. -

2021 Molina Ohio Marketplace Fact Sheet
Ohio Marketplace Fact Sheet Marketplace Counties: Allen Ashtabula Why Choose Molina? Athens Butler Champaign Member Benefits Clark Clermont • NEW $0 deductible Silver and Bronze plans Clinton Coshocton • NEW copay driven plan designs for 2021! Crawford Cuyahoga • FREE 24/7 Teladoc virtual care services and 24-hour nurse advice line Erie Fairfield • FREE child vision benefits include free annual exam and frames/lenses Fayette • FREE annual wellness exams and preventative prescription drugs Franklin Greene • Urgent Care copays are the same as PCP visit copays on all plans Hamilton Hancock • No referral required for specialist visits Highland Holmes • Adult vision services provided by VSP available on select plans Huron Lake • Ability to set up reoccurring premium payments with autopay Lawrence Licking • Ability to choose your PCP at the time of enrollment Lorain Lucas • Mail Order Pharmacy benefit is available to all members Madison Mahoning Molina Healthcare has more than 40 Montgomery Broker Benefits Muskingum years of experience providing quality Pickaway health care for those in need. We offer • Increased renewal commission rates Pike Richland Marketplace plans in California, Florida, • Improved new and renewal member bonus program Ross Michigan, Mississippi, New Mexico, Scioto • One of the best Broker Support Units in the industry Stark Ohio, South Carolina, Texas, Utah, Trumbull • CARE Team can assist with member access to care, claims, and billing Warren Washington, and Wisconsin. Wood www.MolinaHealthcare.com issues without member -

Designated Hospitals and Outpatient Surgery Centers
Ohio and Northern Kentucky UnitedHealthcare Directory of Designated Hospitals and Outpatient Surgery Centers With Choice Plus Advanced with Hospital Tiering, UnitedHealthcare encourages members to make well-informed decisions about who to see and where to go for quality, cost-efficient care through the UnitedHealth Premium® designation program, Place of Service and Hospital Tiering. This directory is a listing of the Designated hospitals and Outpatient Surgery Centers that offer services to UnitedHealthcare members enrolled in our Choice Plus Advanced with Hospital Tiering health plans in Ohio and Northern Kentucky. Members may pay lower co-payments and co-insurance amounts for services provided by Designated hospitals and surgery centers. The providers on this list may change. The Ohio Designated Hospitals and Outpatient Surgery Centers Allen: Belmont: Springfield Regional Cleveland Association Digestive Health Endoscopy Digestive Health Complex Medical Center* 5106 Wilson Mills Rd 375 N Eastown Rd 300 W Main St 100 Medical Center Drive Richmond Heights, OH 44143 Springfield, OH 45504 Lima, OH 45807 Saint Clairsville, OH 43950 Cleveland Center For Digestive Endoscopy Center Valley Endoscopy Center Mercy Memorial Hospital* Health & Endoscopy Of West Central Ohio 68377 STEwart Dr STE 202 904 Scioto St 3700 Park East Dr STE 100A 2793 Shawnee Rd Saint Clairsville, OH 43950 Urbana, OH 43078 Beachwood, OH 44122 Lima, OH 45806 Cleveland Eye/Laser Butler: Clermont: Endoscopy Center Surgery Center GI Endoscopy Center Midwest Eye Surgery Center -

Network Plan Trihealth Inc FCC Healthcare Connect Fund
Network Plan TriHealth Inc FCC Healthcare Connect Fund 1. Background, Goals and Objectives of the proposed network TriHealth is a unified health care system based in Cincinnati, Ohio. It was formed in 1995 by bringing together two of Cincinnati’s most reputable health care organizations: Bethesda Hospital and Good Samaritan Hospital. These two acute care hospitals enable TriHealth to provide a wide range of clinical, emergency, educational, preventive and social programs. In addition, TriHealth's non-hospital services include physician practice management, fitness centers, occupational health centers, home health, and hospice care. To accomplish its mission, TriHealth has a large number of physicians and specialists on staff. In fact, TriHealth is one of the largest employers in greater Cincinnati with over 11,000 employees including nearly 600 employed physicians and residents. TriHealth is ranked as a top rated employer in the country. The TriHealth system now comprises five hospitals: Bethesda North Hospital with approximately 360 adult and 60 newborn beds. Good Samaritan Hospital with approximately 460 adult and 130 newborn beds. Bethesda Butler Hospital in Hamilton, Ohio. McCullough-Hyde Memorial Hospital in Oxford, Ohio. TriHealth Evandale Hospital in Evandale, Ohio. In addition, there are over 125 clinics and other health care facilities in the Greater Cincinnati area that have access to the TriHeath resources. TriHealth is also a major affiliate of undergraduate medical education with the University of Cincinnati College of Medicine including: Graduate medical education/residency programs in: Family Practice, Internal Medicine, Obstetrics and Gynecology, and General Surgery. Fellowships in: Vascular Surgery, Female Pelvic Medicine and Reconstructive Surgery, Family Medicine/Sports Medicine, Robotic-Assisted Cardiovascular Surgery, Family Medicine/Sleep Medicine. -

How Safe Is Your Hospital?
FEATURE SURGICAL INFECTION Patrick Roth of Dartmouth, Mass., can’t walk unassisted since he experienced several complications after surgery. the government doesn’t adequately track it as it does deaths from automobiles, plane crashes, and cancer. It’s appalling.” How safe is That lack of information not only makes it difficult to define the extent of the prob- lem but also makes it challenging for pa- tients to know about the safety of the your hospital? hospitals in their communities. To address that problem, Consumer Our new Ratings find too many pose risks Reports has for the first time rated hospi- tals for safety, using the most current data ospitals should be places says. “That’s like wiping out the entire pop- available to us at the time of our analysis. you go to get better, but too of- ulations of North Dakota, Rhode Island, It included information from government ten the opposite happens. and Vermont. It’s a man-made disaster.” and independent sources on 1,159 hospi- Infections, surgical mistakes, Some hospitals have responded to the tals in 44 states. For this report, we also Hand other medical harm contribute to the crisis with safety initiatives such as elec- interviewed patients, physicians, hospi- deaths of 180,000 hospital patients a year, tronic prescribing to help prevent drug er- tal administrators, and safety experts; re- according to projections based on a 2010 rors and checklists to prevent infections, viewed medical literature; and looked at report from the Department of Health and with some success. Rates of central-line hospital inspections and investigations. -

City of Cincinnati Budget Book Update.Book
FISCAL YEAR 2019 RECOMMENDED CINCINNATI, OHIO ALL FUNDS BUDGET UPDATE City of Cincinnati - Approved FY 2017 Budget UpdateCity of Cincinnati - Approved FY 2017 Budget Update Recommended Fiscal Year 2019 All Funds Budget Update Mayor John Cranley Vice-Mayor Christopher Smitherman Members of City Council Tamaya Dennard Greg Landsman David Mann Amy Murray Jeff Pastor Chris Seelbach P. G. Sittenfeld Wendell Young City Administration Patrick A. Duhaney, Acting City Manager Sheila Hill-Christian, Assistant City Manager John Juech, Assistant City Manager Christopher A. Bigham, Budget Director Reginald Zeno, Finance Director Karen Alder, Assistant Finance Director &LWL]HQVRI&LQFLQQDWL &LW\&RQWUDFWXDO%RDUGV %RDUGVDQG&RPPLVVLRQ 0D\RU &LW\&RXQFLO 'HSDUWPHQWV Southwest Ohio Regional Transit Authority (SORTA) +XPDQ5HODWLRQV Board of Health &LW\0DQDJHU %XGJHW (YDOXDWLRQ (QYLURQPHQW 6XVWDLQDELOLW\ ,QWHUQDO$XGLW 3HUIRUPDQFH 'DWD$QDO\WLFV Park Board &RPPXQLFDWLRQV Recreation Commission Fire Department Public Services Department Police Department Law Department Retirement Human Resources Department Community & Economic Development Department Transportation & Engineering Department Finance Department Enterprise Technology Solutions Greater Cincinnati Water Works Sewers Stormwater Citizen Complaint Authority Buildings & Inspections Economic Inclusion City Planning Department Enterprise Services Convention Center Parking Systems City Manager’s Office Office of Budget and Evaluation 801 Plum Street, Suite 142 Cincinnati, OH 45202 513.352.3232 513.352.3233 (fax) -

Healthcare Practice Leader [email protected] 937-224-0861
For More Information Please Contact Joseph Ferdelman, PE, HFDP, LEED AP BD+C Healthcare Practice Leader [email protected] 937-224-0861 www.heapy.com Enhancing the Patient Experience ABOUT HEAPY HEAPY is a nationally recognized leader in Sustainability, providing innovative and creative engineering solutions for the Healthcare, Mission Critical, Higher Education, Government and Cultural Markets. Our services include: • Mechanical, Electrical & Fire Protection Systems Design • Technology Design • Planning Services • LEED & Energy Services • Commissioning Services • SMART Technologies Integration HEALTHCARE ENGINEERING Building a More Resilient and Sustainable Society HealthCare Facility Design Professionals Certified Healthcare Constructor ISO Certified Company (FS-98575) HEALTHCARE FACILITIES CLIENTS ENHANCING THE PATIENT Adena Cancer Center • Academic Medical Centers • Labs & Pharmacies Avondale Meadows • Ambulatory Care • Medical Centers / Hospitals Health and Wellness • Cancer Centers • Medical Education Berger Hospital Cleveland Clinic EXPERIENCE • Children’s Hospitals • Medical Office Buildings Dayton Children’s Hospital • Senior Living • Dental Medicine Dublin Methodist Hospital • Emergency Departments • Veteran Affairs Genesis Hospital Good Samaritan Hospital Kettering Health Network - Fort Hamilton Hospital - Grandview Medical Center - Greene Memorial Hospital - Kettering Medical Center - Soin Medical Center - Southview Hospital - Sycamore Medical Center Mount Carmel Grove City Memorial Hospital of South Bend VAMC Patient Tower