Neoplasia: Core Concepts
Neoplasia: core concepts

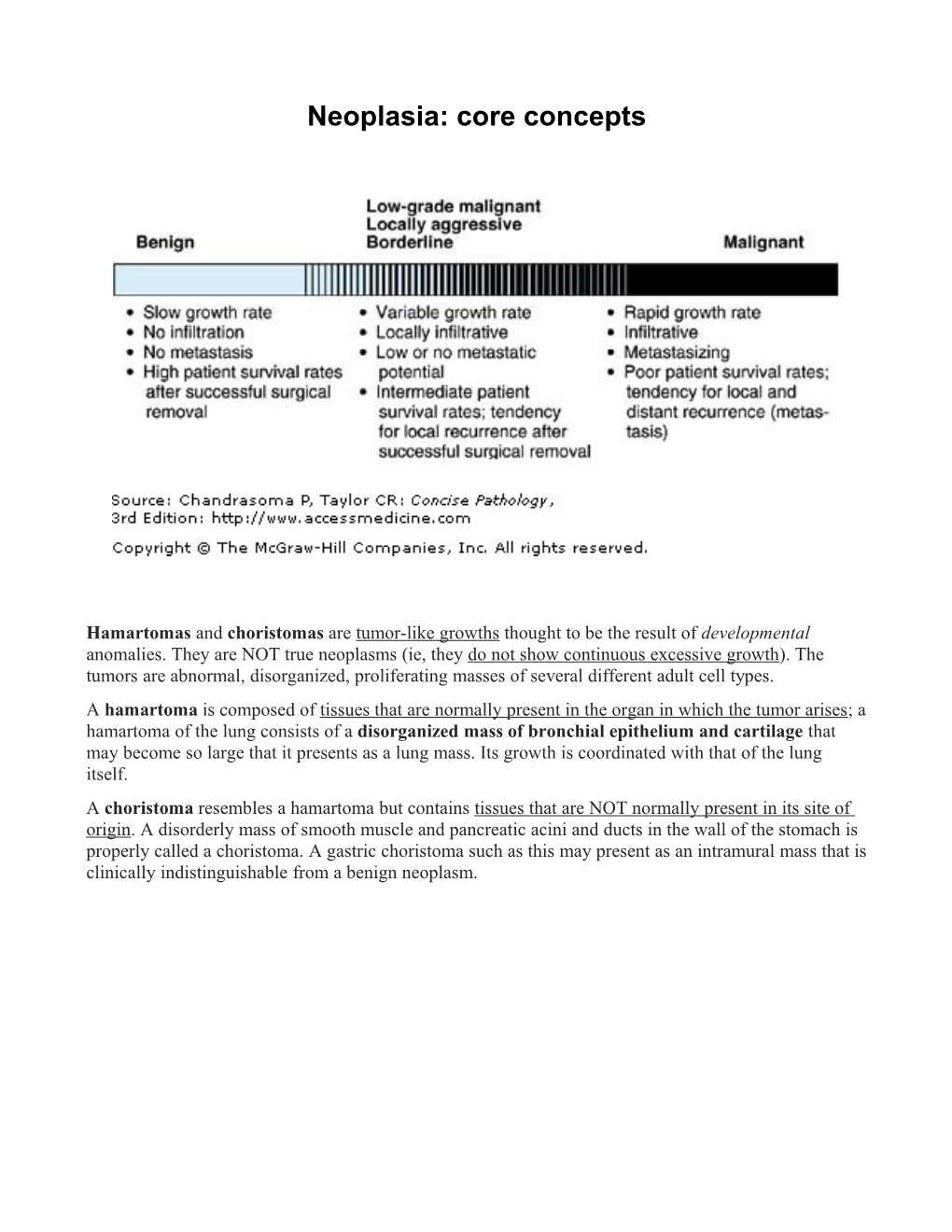
Hamartomas and choristomas are tumor-like growths thought to be the result of developmental anomalies. They are NOT true neoplasms (ie, they do not show continuous excessive growth). The tumors are abnormal, disorganized, proliferating masses of several different adult cell types.
A hamartoma is composed of tissues that are normally present in the organ in which the tumor arises; a hamartoma of the lung consists of a disorganized mass of bronchial epithelium and cartilage that may become so large that it presents as a lung mass. Its growth is coordinated with that of the lung itself.
A choristoma resembles a hamartoma but contains tissues that are NOT normally present in its site of origin. A disorderly mass of smooth muscle and pancreatic acini and ducts in the wall of the stomach is properly called a choristoma. A gastric choristoma such as this may present as an intramural mass that is clinically indistinguishable from a benign neoplasm.

A benignepithelial neoplasm is called an adenoma if it arises within a gland (eg, thyroid adenoma, colonic adenoma) or a papilloma when arising from an epithelial surface. Papillomas may arise from squamous, glandular, or transitional epithelium (eg, squamous papilloma, intraductal papilloma of the breast, and transitional cell papilloma, respectively).
-Malignantepithelial neoplasms are called carcinomas (adenocarcinomas if derived from glandular epithelia; squamous carcinoma and transitional cell carcinoma if originating in those kinds of epithelia).
Benignmesenchymal neoplasms are named after the cell of origin (a Greek or Latin word is used) followed by the suffix -oma (Table 17-4). The names of these tumors may contain the organ of origin and an adjective, eg, cavernous hemangioma of the liver
Malignantmesenchymal neoplasms are named after the cell of origin, to which is added the suffix -sarcoma. Again, adjectives are commonly used; liposarcomas are classified as sclerosing, myxoid, round cell, or pleomorphic
Mixed Tumors: Neoplasms composed of more than one neoplastic cell type are called mixed tumors. Malignant mixed tumors may have two epithelial components, as in adenosquamous carcinoma; two mesenchymal components, as in malignant fibrous histiocytoma; or an epithelial and a mesenchymal component, as in carcinosarcoma of the lung and malignant mixed müllerian tumor of the uterus
Mechanisms and Causes
Intro: Neoplasia is an abnormality of cell growth and multiplication characterized by the following features: (1) excessive cellular proliferation that typically produces an abnormal mass, or tumor; (2) uncoordinated growth occurring without any apparent purpose; and (3) persistence of excessive cell proliferation and growth even after the inciting stimulus that evoked the change has been removed—ie, neoplasia is an irreversible process.
Origin of tumor:
Monoclonal: the initial neoplastic change affects a single cell, which then multiplies and gives rise to the neoplasm. Example: neoplasms of B lymphocytes (B-cell lymphomas and plasma-cell myelomas) that produce immunoglobulin.
-REMEMBER: as a neoplasm progresses, further subclones may evolve from the initial clone as a result of additional ongoing genetic changes (multiple hits)
Field origin: A carcinogenic agent acting on a large number of similar cells may produce a field of potentially neoplastic cells. Neoplasms may then arise from one or more cells within this field. In many cases the result is several discrete neoplasms, each of which derives from a separate clonal precursor. The field change may be regarded as the first of 2 or more sequential steps that lead to overt cancer.
Multiple Hits
Theory that carcinogenesis requires two hits. The first event is initiation, with the carcinogen causing it called the initiator. The second event, which induces neoplastic growth, is promotion, and the agent is the promoter. It is now believed that in fact multiple hits occur (five or more), that multiple factors may cause these hits, and that each hit produces a change in the genome of the affected cell that is transmitted to its progeny (ie, the neoplastic clone).
-another way to put it - Genetic predisposition = 1st hit, then a somatic mutation (due to, for example, a carcinogen) provides the 2nd hit
-another example: Oncogenesis in Burkitt's lymphoma. The 1st hit is infection of B lymphocytes with Epstein-Barr virus. Chronic malaria induces proliferation of B lymphocytes, increasing the likelihood of the 2nd hit, which is a chromosomal translocation that activates a cellular oncogene and leads to malignant lymphoma.
Oncogenes and tumor suppressor genes
There are two main categories of genes that regulate cell growth, and the abnormal action of either or both may lead to neoplasia. Proto-oncogenes (cellular oncogenes: c-onc) code for a variety of growth factors, receptors, and signal-relay or transcription factors, which act in concert to control entry into the cell cycle (eg, the growth promoter effect). The action of these genes is opposed by the action of tumor suppressor genes, which serve to down-regulate the cell cycle. A net increase in the production of stimulatory (promoter) factors, a decrease in inhibitory (suppressor) growth factors, or the production of functionally abnormal factors may lead to uncontrolled cell growth.
The neoplastic cell is then the result of several such changes interacting in summative fashion (multiple hits). Hits may result from inherited genetic abnormalities, spontaneous mutations, or the actions of external agents that may affect the gene. These mutagens include chemical carcinogens, ionizing radiation, and viruses (which introduce new DNA). The effect of these agents is exacerbated by incompetent DNA repair mechanisms such as mutation of the genes that monitor DNA duplication. Defective repair is common in peeps with certain inherited conditions (such as xeroderma pigmentosum [sunlight; skin cancer]). In dudes with these conditions, a first hit (eg, defective repair mechanisms) is inherited and is already present in every cell in the body.
Mechanisms of gene activation and inactivation
Neoplastic transformation occurs as a result of activation (or “derepression”) of growth promoter genes (proto-oncogenes) or inactivation or loss of suppressor genes. Activation is a functional concept where the normal action of growth regulation is diverted into oncogenesis. The resultant activated proto-oncogene is referred to as an activated oncogene (or a mutant oncogene, if structurally changed). Activation and inactivation may occur through several mechanisms:
(1)mutation, including single nucleotide loss (frameshift) or substitution (nonsense or missense codon), codon loss, gene deletion or more major chromosomal loss
(2)translocation to a different part of the genome where regulatory influences may favor inappropriate expression or repression
(3)insertion of an oncogenic virus at an adjacent site
(4)amplification (production of multiple copies of the proto-oncogenes), which appear as additional chromosome bands or extra DNA fragments (double minutes)
(5)introduction of viral oncogenes
(6)derepression (loss of suppressor control).
See lecture slides for summary of agents causing neoplasms (i.e. carcinogens) - she actually wasn’t terrible at that part
Biological and clinical effects of neoplasias
Products/markers of neoplasias
- Enzymes: Elevated serum levels of prostate-specific acid phosphatase occur in prostate cancer, usually when invasion has occurred beyond the capsule of the gland. Measurement of prostate-specific epithelial antigen (PSA) is more sensitive and has found use as a screening test in older men.
- Excessive Hormone Secretion: Well-differentiated neoplasms of endocrine cells are frequently associated with excessive production of hormones. Overproduction is due not only to the increased number of cells caused by the tumor but also to a failure of normal control mechanisms. The resulting clinical symptoms are readily predictable because they represent the manifestations of excess hormone levels.
- Example: GH, prolactin, ACTH in pituitary adenoma
Abnormal differentiation and anaplasia
When benign or slow-growing malignant neoplastic cells proliferate, they tend to differentiate normally and resemble their normal counterparts (ie, they are well-differentiated). For example, the cells constituting a lipoma resemble mature adipocytes on microscopic examination.
As the degree of malignancy increases, the degree of differentiation decreases, and neoplastic cells do not resemble the cell of origin so closely. When the cell of origin cannot be recognized on microscopic examination, it is dubbed undifferentiated or anaplastic.
-Anaplastic cells display marked pleomorphism. The nuclei are characteristically extremely hyperchromatic (darkly stained) and large. The nuclear-cytoplasmic ratio may approach 1:1 instead of the normal 1:4 or 1:6. Giant cells that are considerably larger than their neighbors may be formed and possess either one enormous nucleus or several nuclei (syncytia). Anaplastic nuclei are variable and bizarre in size and shape. The chromatin is coarse and clumped, and nucleoli may be of astounding size. More important, mitoses are often numerous and distinctly atypical. Also, anaplastic cells usually fail to develop recognizable patterns of orientation to one another (i.e. they lose normal polarity). They may grow in sheets, with total loss of communal structures, such as gland formation or stratified squamous architecture. Anaplasia is the most extreme disturbance in cell growth encountered in the spectrum of cellular proliferations.
-Metaplasia: Neoplastic cells may occasionally differentiate in a manner that is abnormal for the cell of origin. For example, neoplastic endometrial glandular epithelium sometimes differentiates to form both glandular and squamous epithelial cells (adenosquamous carcinoma). To put it another way, metaplasia is the reversible replacement of one differentiatedcell type with another mature differentiated cell type. This is often due to an abnormal stimulus, forcing the cells to convert into a different type which is better suited for the situation.
Invasion/Infiltration
Carcinomas and sarcomas demonstrate similar patterns of invasion despite their different tissues of origin. Invasion of the basement membrane by carcinoma distinguishes invasive cancer from intraepithelial (i.e. carcinoma in situ) cancer. Having penetrated (haha, penetrated) the basement membrane, malignant cells gain access to the lymphatics and blood vessels, the first step toward general dissemination (Figure 19-10). Infiltrating neoplastic cells tend to follow fascial planes along the pathway of least resistance; eventually, destruction of tissue occurs. The mechanisms whereby neoplastic cells invade and destroy tissues are poorly understood, but protease production, loss of contact inhibition of neoplastic cells, and decreased cell adhesiveness are believed to play a part.
So, to sum up the sequence of events:
■Dysplasia is the earliest form of pre-cancerous lesion recognizable in a pap smear or biopsy. Dysplasia can be low grade or high grade. The risk of low grade dysplasia transforming into high grade dysplasia, and eventually cancer, is low. Treatment is usually straightforward. High grade dysplasia represents a more advanced progression towards malignant transformation.
■Carcinoma in siturepresents the transformation of a neoplastic lesion to one in which cells undergo essentially no maturation, and thus may be considered “cancer-like”. In this state, epithelial cells have lost their tissue identity and have reverted back to a primitive cell form that grows rapidly and without regulation. However, this form of cancer remains localized, and hasNOT invaded past the basement membrane.
■Invasivecarcinoma is the final step in this sequence. It is a cancer which has invaded beyond the basement membrane and has potential to metastasize.
Lymphatic Metastasis
Metastasis via the lymphatics occurs early in carcinomas and melanomas but is an unusual occurrence in most sarcomas, which tend to spread mainly via the bloodstream
Hematogenous Metastasis
Entry of cancerous cells into the bloodstream tends to occur during the early clinical course. Most of these malignant cells are thought to be destroyed by the immune system, but some become coated with fibrin and entrapped in capillaries. Metastasis can occur only if enough cancerous cells survive in the tissues to become established and proliferate at a second site. Production of tumor angiogenesis factor (TAF) by the cancerous cells stimulates growth of new capillaries in the vicinity of tumor cells and encourages vascularization of the growing metastasis.
Grade vs. Stage
Grade: the degree of cellular differentiation. A low grade is well differentiated, a high grade is poorly/undifferentiated.
Stage: the extent of spread of a neoplasm; pathologic stage is determined by the extent of infiltration and metastasis (eg, depth of invasion of the wall of a viscus; lymph node, bone marrow, or organ involvement). Described using TNM classification, which classifies neoplasms on the basis of size of the primary tumor (T), lymph node involvement (N), and distant metastases (M).