Smoking Cessation Guide
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CLINICAL TRIALS Safety and Immunogenicity of a Nicotine Conjugate Vaccine in Current Smokers
CLINICAL TRIALS Safety and immunogenicity of a nicotine conjugate vaccine in current smokers Immunotherapy is a novel potential treatment for nicotine addiction. The aim of this study was to assess the safety and immunogenicity of a nicotine conjugate vaccine, NicVAX, and its effects on smoking behavior. were recruited for a noncessation treatment study and assigned to 1 of 3 doses of the (68 ؍ Smokers (N nicotine vaccine (50, 100, or 200 g) or placebo. They were injected on days 0, 28, 56, and 182 and monitored for a period of 38 weeks. Results showed that the nicotine vaccine was safe and well tolerated. Vaccine immunogenicity was dose-related (P < .001), with the highest dose eliciting antibody concentrations within the anticipated range of efficacy. There was no evidence of compensatory smoking or precipitation of nicotine withdrawal with the nicotine vaccine. The 30-day abstinence rate was significantly different across with the highest rate of abstinence occurring with 200 g. The nicotine vaccine appears ,(02. ؍ the 4 doses (P to be a promising medication for tobacco dependence. (Clin Pharmacol Ther 2005;78:456-67.) Dorothy K. Hatsukami, PhD, Stephen Rennard, MD, Douglas Jorenby, PhD, Michael Fiore, MD, MPH, Joseph Koopmeiners, Arjen de Vos, MD, PhD, Gary Horwith, MD, and Paul R. Pentel, MD Minneapolis, Minn, Omaha, Neb, Madison, Wis, and Rockville, Md Surveys show that, although about 41% of smokers apy, is about 25% on average.2 Moreover, these per- make a quit attempt each year, less than 5% of smokers centages most likely exaggerate the efficacy of are successful at remaining abstinent for 3 months to a intervention because these trials are typically composed year.1 Smokers seeking available behavioral and phar- of subjects who are highly motivated to quit and who macologic therapies can enhance successful quit rates are free of complicating diagnoses such as depression 2 by 2- to 3-fold over control conditions. -

Smoking Cessationreview Smoking Cessation YEARS Research Review MAKING EDUCATION EASY SINCE 2006
RESEARCH Smoking CessationREVIEW Smoking Cessation YEARS Research Review MAKING EDUCATION EASY SINCE 2006 Making Education Easy Issue 24 – 2016 In this issue: Welcome to issue 24 of Smoking Cessation Research Review. Encouraging findings suggest that varenicline may increase smoking abstinence rates in light smokers Have combustible cigarettes (5–10 cigarettes per day). However, since the study was conducted in a small cohort of predominantly White met their match? cigarette smokers, it will be interesting to see whether the results can be generalised to a larger population Supporting smokers with that is more representative of the real world. depression wanting to quit Computer-generated counselling letters that target smoking reduction effectively promote future cessation, Helping smokers quit after report European researchers. Their study enrolled smokers who did not intend to quit within the next diagnosis of a potentially 6 months. At the end of this 24-month investigation, 6-month prolonged abstinence was significantly higher curable cancer amongst smokers who received individually tailored letters compared with those who underwent follow-up assessments only. Preventing postpartum return to smoking We hope you enjoy the selection in this issue, and we welcome any comments or feedback. Varenicline assists smoking Kind Regards, cessation in light smokers Brent Caldwell Natalie Walker [email protected] [email protected] Novel pMDI doubles smoking quit rates Progress towards the Smokefree 2025 goal: too slow Independent commentary by Dr Brent Caldwell. Brent Caldwell was a Senior Research Fellow at Wellington Asthma Research Group, and worked on UK data show e-cigarettes are the Inhale Study. His main research interest is in identifying and testing improved smoking cessation linked to successful quitting methods, with a particular focus on clinical trials of new smoking cessation pharmacotherapies. -

Are Smoking, Environmental Pollution, and Weather Conditions Risk Factors for COVID-19? José Miguel Chatkin1a, Irma Godoy2a
J Bras Pneumol. 2020;46(5):e20200183 https://dx.doi.org/10.36416/1806-3756/e20200183 REVIEW ARTICLE Are smoking, environmental pollution, and weather conditions risk factors for COVID-19? José Miguel Chatkin1a, Irma Godoy2a 1. Departamento de Medicina Interna ABSTRACT e Pneumologia, Escola de Medicina, Pontifícia Universidade Católica do Rio Coronavirus disease 2019 (COVID-19), caused by the highly contagious severe acute Grande do Sul, Porto Alegre (RS) Brasil. respiratory syndrome coronavirus 2 (SARS-CoV-2), is probably systemic, has a major 2. Disciplina de Pneumologia, respiratory component, and is transmitted by person-to-person contact, via airborne Departamento de Clínica Médica, droplets or aerosols. In the respiratory tract, the virus begins to replicate within cells, Faculdade de Medicina de Botucatu, after which the host starts shedding the virus. The individuals recognized as being at risk Universidade Estadual Paulista, Botucatu (SP) Brasil. for an unfavorable COVID-19 outcome are those > 60 years of age, those with chronic diseases such as diabetes mellitus, those with hypertension, and those with chronic lung Submitted: 20 April 2020. diseases, as well as those using chemotherapy, corticosteroids, or biological agents. Accepted: 27 May 2020. Some studies have suggested that infection with SARS-CoV-2 is associated with other Study carried out at the Escola de risk factors, such as smoking, external environmental pollution, and certain climatic Medicina, Pontifícia Universidade Católica conditions. The purpose of this narrative review was to perform a critical assessment of do Rio Grande do Sul, Porto Alegre (RS) the relationship between COVID-19 and these potential risk factors. and at the Faculdade de Medicina de Botucatu, Universidade Estadual Paulista, Keywords: Coronavirus infections; COVID-19; Air pollution; Smoking; Tobacco use Botucatu (SP) Brasil. -

Healthy Mouth, Healthy You the Connection Between Oral and Overall Health
Healthy Mouth, Healthy You The connection between oral and overall health Your dental health is part of a bigger picture: whole-body wellness. Learn more about the relationship between your teeth, gums and the rest of your body. We keep you smiling® deltadentalins.com/enrollees Pregnancy Pregnancy is a crucial time to take care of your oral health. Hormonal changes may increase the risk of gingivitis, or inflammation of the gums. Symptoms include tenderness, swelling and bleeding of the gums. Without proper care, these problems may become more serious and can lead to gum disease. Gum disease is linked to premature birth and low birth weight. If you notice any changes in your mouth during pregnancy, see your dentist. WHAT YOU CAN DO • Be vigilant about your oral health. Brush twice daily and floss at least once a day — these basic oral health practices will help reduce plaque buildup and keep your mouth healthy. • Talk to your dentist. Always let your dentist know that you are pregnant. • Eat well. Choose nutritious, well-balanced meals, including fresh fruits, raw vegetables and dairy products. Athletics Sports and exercise are great ways to build muscle and improve cardiovascular health, but they can also increase risks to your oral health. Intense exercise can dry out the mouth, leading to a greater chance of tooth decay. If you play a high-impact sport without proper protection, you risk knocking out a tooth or dislocating your jaw. WHAT YOU CAN DO • Hydrate early. Prevent dehydration by drinking water during your workout — and several hours beforehand. • Skip the sports drinks. -

July 2021 L.A. Care Health Plan Medi-Cal Dual Formulary
L.A. Care Health Plan Medi-Cal Dual Formulary Formulary is subject to change. All previous versions of the formulary are no longer in effect. You can view the most current drug list by going to our website at http://www.lacare.org/members/getting-care/pharmacy-services For more details on available health care services, visit our website: http://www.lacare.org/members/welcome-la-care/member-documents/medi-cal LA1308E 02/20 EN lacare.org Last Updated: 07/01/2021 INTRODUCTION Foreword Te L.A. Care Health Plan (L.A. Care) Medi-Cal Dual formulary is a preferred list of covered drugs, approved by the L.A. Care Health Plan Pharmacy Quality Oversight Committee. Tis formulary applies only to outpatient drugs and self-administered drugs not covered by your Medicare Prescription Drug Beneft. It does not apply to medications used in the inpatient setting or medical ofces. Te formulary is a continually reviewed and revised list of preferred drugs based on safety, clinical efcacy, and cost-efectiveness. Te formulary is updated on a monthly basis and is efective the frst of every month. Tese updates may include, and are not limited to, the following: (i) removal of drugs and/or dosage forms, (ii) changes in tier placement of a drug that results in an increase in cost sharing, and (iii) any changes of utilization management restrictions, including any additions of these restrictions. Updated documents are available online at: lacare.org/members/getting-care/pharmacy-services. If you have questions about your pharmacy coverage, call Customer Solutions Center at 1-888-839-9909 (TTY 711), available 24 hours a day, 7 days a week. -

Trends in Cigarette Smoking Cessation in the United States
Tobacco Control 1993; 2 (suppl): S3-S16 S3 SESSION I TRENDS IN CESSATION Tob Control: first published as 10.1136/tc.2.suppl1.S4 on 1 January 1993. Downloaded from Introduction Saul Shiftman I'm happy to welcome you here on behalf of of the National Heart, Lung and Blood the Planning Committee. It's a pleasure to see Institute's Smoking Education Program, this actually happening after almost a year of whose job it is to translate findings from planning, and I'm looking forward to the next intervention research into community action day and a half. and education programmes; he was formerly We have 2454 days left until the year 2000, the director of smoking intervention with the at which point the national goals are to have a American Heart Association. smoking prevalence of 15%. We're now at Dr Ellen Gritz is a long-time colleague of roughly 25 %. Put another way, we are 81 % of mine, although I hesitate to remind her in the way to the year 2000 from 1964, the year of public that she and I first started working the first Surgeon General's report, and we together a little over 20 years ago in Los have cut smoking prevalence roughly by half. Angeles. She is certainly one of the leading So we're doing pretty well but still have a bit experts in smoking and smoking cessation, and further to go. has particular interests in smoking among In this morning's panel, we'll be discussing women and in special populations. where we're going and how we're going to get Our last panellist, Dr Patrick O'Malley is there in terms of smoking cessation. -
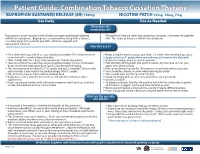
Bupropion + Patch
Patient Guide: Combination Tobacco Cessation Therapy BUPROPION SUSTAINED RELEASE (SR) 150mg NICOTINE PATCH 21mg, 14mg, 7mg Use Daily Use As Needed What does this medication do? Bupropion is a non-nicotine aid that helps you quit smoking by reducing The patch will release small, but continuous amounts of nicotine through the withdrawal symptoms. Bupropion is recommended along with a tobacco skin. This helps to decrease withdrawal symptoms. cessation program to provide you with additional support and educational materials. How do I use it? BUPROPION SUSTAINED RELEASE (SR) 150mg NICOTINE PATCH 21mg, 14mg, 7mg Set a date when you intend to stop smoking (quit date). The medicine needs Begin using the patch on your quit date, 1-2 weeks after starting bupropion. to be started 1-2 weeks before that date. Apply only one (1) patch when you wake up and remove the old patch. Take 1 tablet daily for 3 days, then increase to 1 tablet twice daily. If you miss a dose, use it as soon as you can. Take at a similar time each day, allowing approximately 8 hours in between Peel the back off the patch and put it on clean, dry, hair-free skin on your doses. Don’t take bupropion past 5pm to avoid trouble sleeping. upper arm, chest or back. This medicine may be taken for 7-12 weeks and up to 6 months. Discuss with Press patch firmly in place for 10 seconds so it will stick well to your skin. your provider if you need to be treated longer than 12 weeks. -
Use of Non Cigarette Tobacco Products (NCTP) Smokeless
Non Cigarette Tobacco Products (NCTP) and Electronic cigarettes (e-cigs) Michael V. Burke EdD Asst: Professor of Medicine Nicotine Dependence Center Mayo Clinic, Rochester, MN Email: [email protected] ©2011 MFMER | slide-1 Goals & Objectives • Review NCTP definitions & products • Discuss prevalence/trends of NCTP • Discuss NCTP and addiction • Review recommended treatments for NCTP ©2011 MFMER | slide-2 NCTP Definitions & Products ©2011 MFMER | slide-3 Pipes ©2011 MFMER | slide-4 Cigars Images from www.trinketsandtrash.org ©2011 MFMER | slide-5 Cigar Definition U.S. Department of Treasury (1996): Cigar “Any roll of tobacco wrapped in leaf tobacco or any substance containing tobacco.” vs. Cigarette “Any roll of tobacco wrapped in paper or in any substance not containing tobacco.” ©2011 MFMER | slide-6 NCI Monograph 9. Cigars: Health Effects and Trends. ©2011 MFMER | slide-7 ©2011 MFMER | slide-8 Smokeless Tobacco Chewing tobacco • Loose leaf (i.e., Redman) • Plugs • Twists Snuff • Moist (i.e., Copenhagen, Skoal) • Dry (i.e., Honest, Honey bee, Navy, Square) ©2011 MFMER | slide-9 “Chewing Tobacco” = Cut tobacco leaves ©2011 MFMER | slide-10 “Snuff” = Moist ground tobacco ©2011 MFMER | slide-11 Type of ST Used in U.S. Chewing Tobacco Snuff National Survey on Drug Use and Health (NSDUH) ©2011 MFMER | slide-12 “Spitless Tobacco” – Star Scientific ©2011 MFMER | slide-13 RJ Reynold’s ©2011 MFMER | slide-14 “Swedish Style” ST ©2011 MFMER | slide-15 Phillip Morris (Altria) ©2011 MFMER | slide-16 New Product: “Fully Dissolvables” ©2011 MFMER -

Smoking Cessation: a Report of the Surgeon General – 2020
A SUMMARY OF SMOKING CESSATION: A REPORT OF THE SURGEON GENERAL – 2020 Smoking Cessation – The Role of Healthcare Professionals and Health Systems Smoking in the U.S. Key Findings from the 2020 Since the first Surgeon General’s report on smoking and health was Surgeon General’s Report released in 1964, cigarette smoking among U.S. adults has declined from nearly 43% to a low of nearly 14% in 2018. Despite this progress, smoking ` Smoking cessation reduces risk for many adverse health remains the leading cause of preventable disease and death in the U.S. effects, including poor reproductive health outcomes, Additionally, smoking-related illnesses continue to cost the nation more cardiovascular diseases, chronic obstructive pulmonary than $300 billion every year. disease (COPD), and cancer. Quitting smoking is also beneficial to those who have been diagnosed with heart Smoking Cessation Saves Lives disease and COPD. ` More than three out of five U.S. adults who have ever and Money smoked cigarettes have quit. Although a majority of cigarette smokers make a quit attempt each year, less Tobacco dependence is a chronic, relapsing condition driven by than one-third use cessation medications approved addiction to nicotine. But cessation treatment can help people quit. by the U.S. Food and Drug Administration (FDA) or The 2020 Surgeon General’s Report highlights the latest evidence on the behavioral counseling to support quit attempts. benefits of smoking cessation. The evidence is clear – one of the most important actions people can take to improve their health is to quit ` Considerable disparities exist in the prevalence of smoking, no matter how old they are or how long they’ve been smoking. -

Smoking Cessation for Persons with Mental Illnesses
Smoking Cessation for Persons with Mental Illnesses A Toolkit for Mental Health Providers Updated January 2009 Table of Contents Overview 1 Why Address This Issue? 1 2 Alarming Statistics 2 3 About this Toolkit: 2 Who is this toolkit for? How do I use this toolkit? 4 Provider Pull-Out: Quick Facts Tobacco Use and Mental Illness 1 Smoking and Mental Illness: 3 Biological Predispositions, Psychological Considerations, Social Considerations, Stigma 2 Specific Psychiatric and Co-occuring Mental Disorders: 4 Depression, Schizophrenia, Co-occuring Substance Abuse and Dependance, Other Psychiatric Disorders 3 Tobacco Industry Targeting 5 Assessment and Intervention Planning 1 Readiness to Quit and Stages of Change: 6 Stages of Change, The 5 A’s (Flowchart, Actions and Strategies), The 5 R’s (Addressing Tobacco Cessation for Tobacco User Unwilling to Quit) 2 Cultural Considerations: 12 Recommendations for Mental Health Clinicians, Resources 3 Example of a Clinic Screening 4 Example of a Quitline Referral Form 5 Provider Pull-Out: The 5A’s and 2A’s & R Models Smoking Cessation Treatment for Persons with Mental Illness 1 Key Findings 14 2 Components of Successful Intensive Intervention Programs 15 3 Behavioral Interventions for Smoking Cessation: 16 Overview, SANE program, More Elements of Successful Counseling 4 Prescribing Cessation Medications 18 5 Intervening with Specific Mental Disorders: 19 Depression, Schizophrenia, Bipolar Disorder, Anxiety Disorder, Substance Use Disorders 6 Peer-to-Peer Services 21 7 Smoke-Free Policies 22 8 Provider -

Transdermal Nicotine Maintenance Attenuates the Subjective And
Neuropsychopharmacology (2004) 29, 991–1003 & 2004 Nature Publishing Group All rights reserved 0893-133X/04 $25.00 www.neuropsychopharmacology.org Transdermal Nicotine Maintenance Attenuates the Subjective and Reinforcing Effects of Intravenous Nicotine, but not Cocaine or Caffeine, in Cigarette-Smoking Stimulant Abusers 1 1 ,1,2 Bai-Fang X Sobel , Stacey C Sigmon and Roland R Griffiths* 1Department of Psychiatry and Behavioral Science, Johns Hopkins University School of Medicine, Baltimore, MD, USA; 2Department of Neuroscience, Johns Hopkins University School of Medicine, Baltimore, MD, USA The effects of transdermal nicotine maintenance on the subjective, reinforcing, and cardiovascular effects of intravenously administered cocaine, caffeine, and nicotine were examined using double-blind procedures in nine volunteers with histories of using tobacco, caffeine, and cocaine. Each participant was exposed to two chronic drug maintenance phases (21 mg/day nicotine transdermal patch and placebo transdermal patch). Within each drug phase, the participant received intravenous injections of placebo, cocaine (15 and 30 mg/70 kg), caffeine (200 and 400 mg/70 kg), and nicotine (1.0 and 2.0 mg/70 kg) in mixed order across days. Subjective and cardiovascular data were collected before and repeatedly after drug or placebo injection. Reinforcing effects were also assessed after each injection with a Drug vs Money Multiple-Choice Form. Intravenous cocaine produced robust dose-related increases in subjective and reinforcing effects; these effects were not altered by nicotine maintenance. Intravenous caffeine produced elevations on several subjective ratings; nicotine maintenance did not affect these ratings. Under the placebo maintenance condition, intravenous nicotine produced robust dose-related subjective effects, with maximal increases similar to the high dose of cocaine; nicotine maintenance significantly decreased the subjective and reinforcing effects of intravenous nicotine. -

Building Capacity for Smoking Cessation and Treatment of Tobacco
BUILDING CAPACITY FOR SMOKING Chapter 5 CESSATION AND TREATMENT OF TOBACCO DEPENDENCE Future needs for capacity-building Considerable progress has been made in the provision of effective treatments for tobacco dependence, both behavioural and pharmacological. For many years, behavioural interventions were the only option. Although a combination of behavioural and pharmacological treatment produces the best outcomes, behavioural treatments alone can also be effective. It is critically important that a wide range of interventions be used both in general to support tobacco cessation and specifically to support those who wish to quit tobacco use even where medication is not available (Lando, 2002). Social support for quitting should be possible in all countries, even those with extremely limited resources (Lando, 2002). Success has proved possible from training lay facilitators to conduct group cessation clinics. Abstinence outcomes for those clinics compare favourably with outcomes obtained by doctoral students in counselling psychology. According to the United States Clinical Practice Guideline (United States Department of Health and Human Services, 2000), both social support as part of treatment (intra-treatment social support) and help in securing social support outside of treatment (extra-treatment social support) are especially effective in increasing quitting. All countries have lay persons who can provide informal social support for quitting and who can be trained to conduct more formal interventions. There would appear to be special challenges in countries where there are relatively few ex-smokers and where tobacco prevalence rates are high among health professionals (Lando, 2002). Ex-smokers can serve as role models in encouraging quitting, and can provide social support to individuals who are attempting to quit.