Facial Palsy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recognizing When a Child's Injury Or Illness Is Caused by Abuse
U.S. Department of Justice Office of Justice Programs Office of Juvenile Justice and Delinquency Prevention Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE U.S. Department of Justice Office of Justice Programs 810 Seventh Street NW. Washington, DC 20531 Eric H. Holder, Jr. Attorney General Karol V. Mason Assistant Attorney General Robert L. Listenbee Administrator Office of Juvenile Justice and Delinquency Prevention Office of Justice Programs Innovation • Partnerships • Safer Neighborhoods www.ojp.usdoj.gov Office of Juvenile Justice and Delinquency Prevention www.ojjdp.gov The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs, which also includes the Bureau of Justice Assistance; the Bureau of Justice Statistics; the National Institute of Justice; the Office for Victims of Crime; and the Office of Sex Offender Sentencing, Monitoring, Apprehending, Registering, and Tracking. Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE NCJ 243908 JULY 2014 Contents Could This Be Child Abuse? ..............................................................................................1 Caretaker Assessment ......................................................................................................2 Injury Assessment ............................................................................................................4 Ruling Out a Natural Phenomenon or Medical Conditions -

Nasolabial and Forehead Flap Reconstruction of Contiguous Alar
Journal of Plastic, Reconstructive & Aesthetic Surgery (2017) 70, 330e335 Nasolabial and forehead flap reconstruction of contiguous alareupper lip defects Jonathan A. Zelken a,b, Sashank K. Reddy c, Chun-Shin Chang a, Shiow-Shuh Chuang a, Cheng-Jen Chang a, Hung-Chang Chen a, Yen-Chang Hsiao a,* a Department of Plastic and Reconstructive Surgery, Chang Gung Memorial Hospital, College of Medicine, Chang Gung University, Taipei, Taiwan b Department of Plastic and Reconstructive Surgery, Breastlink Medical Group, Laguna Hills, CA, USA c Department of Plastic and Reconstructive Surgery, Johns Hopkins Hospital, Baltimore, MD, USA Received 4 May 2016; accepted 31 October 2016 KEYWORDS Summary Background: Defects of the nasal ala and upper lip aesthetic subunits can be Nasal reconstruction; challenging to reconstruct when they occur in isolation. When defects incorporate both Nasolabial flap; the subunits, the challenge is compounded as subunit boundaries also require reconstruc- Rhinoplasty; tion, and local soft tissue reservoirs alone may provide inadequate coverage. In such cases, Forehead flap we used nasolabial flaps for upper lip reconstructionandaforeheadflapforalarrecon- struction. Methods: Three men and three women aged 21e79 years (average, 55 years) were treated for defects of the nasal ala and upper lip that resulted from cancer (n Z 4) and trauma (n Z 2). Unaffected contralateral subunits dictated the flap design. The upper lip subunit was excised and replaced with a nasolabial flap. The flap, depending on the contralateral reference, determined accurate alar base position. A forehead flap resurfaced or replaced the nasal ala. Autologous cartilage was used in every case to fortify the forehead flap reconstruction. Results: Patients were followed for 25.6 months (range, 1e4 years). -

Primary Lateral Sclerosis, Upper Motor Neuron Dominant Amyotrophic Lateral Sclerosis, and Hereditary Spastic Paraplegia
brain sciences Review Upper Motor Neuron Disorders: Primary Lateral Sclerosis, Upper Motor Neuron Dominant Amyotrophic Lateral Sclerosis, and Hereditary Spastic Paraplegia Timothy Fullam and Jeffrey Statland * Department of Neurology, University of Kansas Medical Center, Kansas, KS 66160, USA; [email protected] * Correspondence: [email protected] Abstract: Following the exclusion of potentially reversible causes, the differential for those patients presenting with a predominant upper motor neuron syndrome includes primary lateral sclerosis (PLS), hereditary spastic paraplegia (HSP), or upper motor neuron dominant ALS (UMNdALS). Differentiation of these disorders in the early phases of disease remains challenging. While no single clinical or diagnostic tests is specific, there are several developing biomarkers and neuroimaging technologies which may help distinguish PLS from HSP and UMNdALS. Recent consensus diagnostic criteria and use of evolving technologies will allow more precise delineation of PLS from other upper motor neuron disorders and aid in the targeting of potentially disease-modifying therapeutics. Keywords: primary lateral sclerosis; amyotrophic lateral sclerosis; hereditary spastic paraplegia Citation: Fullam, T.; Statland, J. Upper Motor Neuron Disorders: Primary Lateral Sclerosis, Upper 1. Introduction Motor Neuron Dominant Jean-Martin Charcot (1825–1893) and Wilhelm Erb (1840–1921) are credited with first Amyotrophic Lateral Sclerosis, and describing a distinct clinical syndrome of upper motor neuron (UMN) tract degeneration in Hereditary Spastic Paraplegia. Brain isolation with symptoms including spasticity, hyperreflexia, and mild weakness [1,2]. Many Sci. 2021, 11, 611. https:// of the earliest described cases included cases of hereditary spastic paraplegia, amyotrophic doi.org/10.3390/brainsci11050611 lateral sclerosis, and underrecognized structural, infectious, or inflammatory etiologies for upper motor neuron dysfunction which have since become routinely diagnosed with the Academic Editors: P. -

Pharnygeal Arch Set - Motor USMLE, Limited Edition > Neuroscience > Neuroscience
CNs 5, 7, 9, 10 - Pharnygeal Arch Set - Motor USMLE, Limited Edition > Neuroscience > Neuroscience PHARYNGEAL ARCH SET, CNS 5, 7, 9, 10 • They are derived from the pharyngeal (aka branchial) arches • They have special motor and autonomic motor functions CRANIAL NERVES EXIT FROM THE BRAINSTEM CN 5, the trigeminal nerve exits the mid/lower pons.* CN 7, the facial nerve exits the pontomedullary junction.* CN 9, the glossopharyngeal nerve exits the lateral medulla.* CN 10, the vagus nerve exits the lateral medulla.* CRANIAL NERVE NUCLEI AT BRAINSTEM LEVELS Midbrain • The motor trigeminal nucleus of CN 5. Nerve Path: • The motor division of the trigeminal nerve passes laterally to enter cerebellopontine angle cistern. Pons • The facial nucleus of CN 7. • The superior salivatory nucleus of CN 7. Nerve Path: • CN 7 sweeps over the abducens nucleus as it exits the brainstem laterally in an internal genu, which generates a small bump in the floor of the fourth ventricle: the facial colliculus • Fibers emanate from the superior salivatory nucleus, as well. Medulla • The dorsal motor nucleus of the vagus, CN 10 • The inferior salivatory nucleus, CN 9 1 / 3 • The nucleus ambiguus, CNs 9 and 10. Nerve Paths: • CNs 9 and 10 exit the medulla laterally through the post-olivary sulcus to enter the cerebellomedullary cistern. THE TRIGEMINAL NERVE, CN 5  • The motor division of the trigeminal nerve innervates the muscles of mastication • It passes ventrolaterally through the cerebellopontine angle cistern and exits through foramen ovale as part of the mandibular division (CN 5[3]). Clinical Correlation - Trigeminal Neuropathy THE FACIAL NERVE, CN 7  • The facial nucleus innervates the muscles of facial expression • It spans from the lower pons to the pontomedullary junction. -
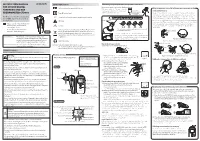
Instruction Manual for Citizen Digital Forehead And
INSTRUCTION MANUAL Symbol Explanations Measuring body temperature (temperature detection) Remove the probe cap and check the probe tip. FOR CITIZEN DIGITAL Refer to instruction manual before use. How to measure correctly in the ear measurement mode * When using it for the first time, open the FOREHEAD AND EAR battery cap and remove the insulation Open the Temperature basics battery cap to THERMOMETER CTD710 Type BF applied part sheet under the battery cap. remove the All objects radiate heat. This device consists of a probe with a built-in insulation sheet. infrared sensor that measures body temperature by detecting the heat Thank you very much for purchasing IP22 Classification for water ingress and particulate matter. radiated by the eardrum and surrounding tissue. Figure 4 shows the the CITIZEN digital forehead and ear Keeping the probe window clean tortuous anatomy of a normal ear canal. As shown in Figure 5, hold the thermometer. Warning Probe window ear and gently pull it back at an angle or pull it straight back to straighten out the ear canal. The shape of the ear canal differs from individual, check • Please read all of the information in before measurement. Accurate temperature measurements make it this instruction manual before Caution essential to straighten the ear canal so that the probe tip directly faces operating the device. the eardrum. • Be sure to have this instruction Indicates this device is subject to the Waste Electrical and Dirt in the probe window will impact the accuracy of temperature detection. External auditory manual to hand during use. 1902LA Electronic Equipment Directive in the European Union. -

Ganglioneuroma of the Sacrum
https://doi.org/10.14245/kjs.2017.14.3.106 KJS Print ISSN 1738-2262 On-line ISSN 2093-6729 CASE REPORT Korean J Spine 14(3):106-108, 2017 www.e-kjs.org Ganglioneuroma of the Sacrum Donguk Lee1, Presacral ganglioneuromas are extremely rare benign tumors and fewer than 20 cases have been reported in the literature. Ganglioneuromas are difficult to be differentiated preoperatively Woo Jin Choe1, from tumors such as schwannomas, meningiomas, and neurofibromas with imaging modalities. 2 So Dug Lim The retroperitoneal approach for resection of presacral ganglioneuroma was performed for gross total resection of the tumor. Recurrence and malignant transformation of these tumors is rare. 1 Departments of Neurosurgery and Adjuvant chemotherapy or radiation therapy is not indicated because of their benign nature. 2Pathology, Konkuk University Medical Center, Konkuk University We report a case of a 47-year-old woman with a presacral ganglioneuroma. School of Medicine, Seoul, Korea Key Words: Ganglioneuroma, Presacral, Anterior retroperitoneal approach Corresponding Author: Woo Jin Choe Department of Neurosurgery, Konkuk University Medical Center, displacing the left sacral nerve roots, without 120-1 Neungdong-ro, Gwangjin-gu, INTRODUCTION Seoul 05030, Korea any evidence of bony invasion (Fig. 2). We performed surgery via anterior retrope- Tel: +82-2-2030-7625 Ganglioneuroma is an uncommon benign tu- ritoneal approach and meticulous adhesiolysis Fax: +82-2-2030-7359 mor of neural crest origin which is mainly loca- was necessary because of massive abdominal E-mail: [email protected] lized in the posterior mediastinum, retroperito- adhesion due to the previous gynecologic sur- 1,6) Received: August 16, 2017 neum, and adrenal gland . -

ALS and Other Motor Neuron Diseases Can Represent Diagnostic Challenges
Review Article Address correspondence to Dr Ezgi Tiryaki, Hennepin ALS and Other Motor County Medical Center, Department of Neurology, 701 Park Avenue P5-200, Neuron Diseases Minneapolis, MN 55415, [email protected]. Ezgi Tiryaki, MD; Holli A. Horak, MD, FAAN Relationship Disclosure: Dr Tiryaki’s institution receives support from The ALS Association. Dr Horak’s ABSTRACT institution receives a grant from the Centers for Disease Purpose of Review: This review describes the most common motor neuron disease, Control and Prevention. ALS. It discusses the diagnosis and evaluation of ALS and the current understanding of its Unlabeled Use of pathophysiology, including new genetic underpinnings of the disease. This article also Products/Investigational covers other motor neuron diseases, reviews how to distinguish them from ALS, and Use Disclosure: Drs Tiryaki and Horak discuss discusses their pathophysiology. the unlabeled use of various Recent Findings: In this article, the spectrum of cognitive involvement in ALS, new concepts drugs for the symptomatic about protein synthesis pathology in the etiology of ALS, and new genetic associations will be management of ALS. * 2014, American Academy covered. This concept has changed over the past 3 to 4 years with the discovery of new of Neurology. genes and genetic processes that may trigger the disease. As of 2014, two-thirds of familial ALS and 10% of sporadic ALS can be explained by genetics. TAR DNA binding protein 43 kDa (TDP-43), for instance, has been shown to cause frontotemporal dementia as well as some cases of familial ALS, and is associated with frontotemporal dysfunction in ALS. Summary: The anterior horn cells control all voluntary movement: motor activity, res- piratory, speech, and swallowing functions are dependent upon signals from the anterior horn cells. -
Facial Nerve Disorders Cn7 (1)
FACIAL NERVE DISORDERS CN7 (1) Facial Nerve Disorders Last updated: January 18, 2020 FACIAL PALSY .......................................................................................................................................... 1 ETIOLOGY .............................................................................................................................................. 1 GUIDE TO LESION SITE LOCALIZATION ................................................................................................... 2 CLINICAL GRADING OF SEVERITY .......................................................................................................... 2 House-Brackmann grading scale ........................................................................................... 2 CLINICO-ANATOMICAL SYNDROMES ..................................................................................................... 2 Supranuclear (Central) Palsy ................................................................................................. 2 Nuclear Lesion ...................................................................................................................... 3 Cerebellopontine Angle Syndrome ....................................................................................... 3 Facial Canal Syndrome ......................................................................................................... 3 Stylomastoid Foramen Syndrome ........................................................................................ -

Downloaded 09/30/21 01:49 PM UTC NF2 Patients There Were Often Multiple Meningiomas
Neurosurg Focus 4 (3):Article 1, 1998 Neurofibromatosis type 2 and central neurofibromatosis Leonard I. Malis, M.D. The Mount Sinai School of Medicine, New York City, New York Neurofibromatosis type 2 (NF2) is a rare disease, affecting only approximately 1000 patients in the entire United States. The diagnosis requires the presence of bilateral acoustic neuromas, but many other tumors of the nervous system are also present. It is a very different disease from von Recklinghausen's neurofibromatosis, NF1. The remarkable genetic research in recent years has defined the origin of NF2 to be the lack of a specific suppressor protein, known as Merlin. While we await a method to replace this protein, the neurosurgical care of these patients is a formidable problem. The author reviews his personal series of 41 patients with NF2 treated during the past 30 years and presents 10 cases in detail to demonstrate their considerable range of differences and the treatment problems they have posed. Key Words * neurofibromatosis type 2 * bilateral acoustic neurofibromatosis * central neurofibromatosis * bilateral acoustic neuromas * bilateral vestibular schwannomas * Merlin * schwannomin This review is based on my personal series of 41 surgically treated patients with neurofibromatosis type 2 (NF2). The patients were cared for in the microsurgical era between 1970 and 1995 and received minimum follow-up care of 3 years (median 12 years). All of these people were referred because of bilateral acoustic neuromas. This was a quite young group, with the average age only 20 years, much younger than my patients with solitary acoustic neuromas. The youngest patient was 8 years old and the oldest 40 years old when first referred. -

The Clinical Treatment and Outcome of Cerebellopontine Angle
www.nature.com/scientificreports OPEN The clinical treatment and outcome of cerebellopontine angle medulloblastoma: a retrospective study of 15 cases Tao Wu 1,4, Pei-ran Qu3,4, Shun Zhang2, Shi-wei Li1, Jing Zhang1, Bo Wang2, Pinan Liu 1,2, Chun-de Li1,2 & Fu Zhao 1,2 ✉ Medulloblastoma (MB) is the most common malignant pediatric brain tumor arising in the cerebellum or the 4th ventricle. Cerebellopontine angle (CPA) MBs are extremely rare tumors, with few cases previously described. In this study, we sought to describe the clinical characteristics, molecular features and outcomes of CPA MB. We retrospectively reviewed a total of 968 patients who had a histopathological diagnosis of MB at the Beijing Neurosurgical Institute between 2002 and 2016. The demographic characteristics, clinical manifestations and radiological features were retrospectively analyzed. Molecular subgroup was evaluated by the expression profling array or immunohistochemistry. Overall survival (OS) and progression-free survival (PFS) were calculated using Kaplan-Meier analysis. In this study, 15 patients (12 adults and 3 children) with a mean age at diagnosis of 25.1 years (range 4–45 years) were included. CPA MBs represented 1.5% of the total cases of MB (15/968). Two molecular subgroups were identifed in CPA MBs: 5 WNT-MBs (33%) and 10 SHH-MBs (67%). CPA WNT-MBs had the extracerebellar growth with the involvement of brainstem (P = 0.002), whereas CPA SHH-MBs predominantly located within the cerebellar hemispheres (P = 0.004). The 5-year OS and PFS rates for CPA MB were 80.0% ± 10.3% and 66.7% ± 12.2%, respectively. -

Diagnostic Value of Preoperative Inflammatory Markers in Patients with Glioma: a Multicenter Cohort Study
CLINICAL ARTICLE J Neurosurg 129:583–592, 2018 Diagnostic value of preoperative inflammatory markers in patients with glioma: a multicenter cohort study *Shi-hao Zheng, MD,1 Jin-lan Huang, PhD,2,4 Ming Chen, MD,3 Bing-long Wang, BS,2 Qi-shui Ou, PhD,2 and Sheng-yue Huang, BS1 1Department of Neurosurgery, Fujian Provincial Hospital; 2Department of Clinical Laboratory, First Affiliated Hospital of Fujian Medical University, Fuzhou, Fujian; 3Department of Neurosurgery, Xin Hua Hospital, Affiliated with Shanghai Jiao Tong University School of Medicine, Shanghai; and 4Laboratory Medicine Center, Nanfang Hospital, Southern Medical University, Guangzhou, Guangdong, People’s Republic of China OBJECTIVE Glioma is the most common form of brain tumor and has high lethality. The authors of this study aimed to elucidate the efficiency of preoperative inflammatory markers, including neutrophil/lymphocyte ratio (NLR), derived NLR (dNLR), platelet/lymphocyte ratio (PLR), lymphocyte/monocyte ratio (LMR), and prognostic nutritional index (PNI), and their paired combinations as tools for the preoperative diagnosis of glioma, with particular interest in its most aggressive form, glioblastoma (GBM). METHODS The medical records of patients newly diagnosed with glioma, acoustic neuroma, meningioma, or nonle- sional epilepsy at 3 hospitals between January 2011 and February 2016 were collected and retrospectively analyzed. The values of NLR, dNLR, PLR, LMR, and PNI were compared among patients suffering from glioma, acoustic neuroma, meningioma, and nonlesional epilepsy and healthy controls by using nonparametric tests. Correlations between NLR, dNLR, PLR, LMR, PNI, and tumor grade were analyzed. Receiver operating characteristic (ROC) curve analysis was performed to evaluate the diagnostic significance of NLR, dNLR, PLR, LMR, PNI, and their paired combinations for glioma, particularly GBM. -

A System for Studying Mechanisms of Neuromuscular Junction Development and Maintenance Valérie Vilmont1,‡, Bruno Cadot1, Gilles Ouanounou2 and Edgar R
© 2016. Published by The Company of Biologists Ltd | Development (2016) 143, 2464-2477 doi:10.1242/dev.130278 TECHNIQUES AND RESOURCES RESEARCH ARTICLE A system for studying mechanisms of neuromuscular junction development and maintenance Valérie Vilmont1,‡, Bruno Cadot1, Gilles Ouanounou2 and Edgar R. Gomes1,3,*,‡ ABSTRACT different animal models and cell lines (Chen et al., 2014; Corti et al., The neuromuscular junction (NMJ), a cellular synapse between a 2012; Lenzi et al., 2015) with the hope of recapitulating some motor neuron and a skeletal muscle fiber, enables the translation of features of neuromuscular diseases and understanding the triggers chemical cues into physical activity. The development of this special of one of their common hallmarks: the disruption of the structure has been subject to numerous investigations, but its neuromuscular junction (NMJ). The NMJ is one of the most complexity renders in vivo studies particularly difficult to perform. studied synapses. It is formed of three key elements: the lower motor In vitro modeling of the neuromuscular junction represents a powerful neuron (the pre-synaptic compartment), the skeletal muscle (the tool to delineate fully the fine tuning of events that lead to subcellular post-synaptic compartment) and the Schwann cell (Sanes and specialization at the pre-synaptic and post-synaptic sites. Here, we Lichtman, 1999). The NMJ is formed in a step-wise manner describe a novel heterologous co-culture in vitro method using rat following a series of cues involving these three cellular components spinal cord explants with dorsal root ganglia and murine primary and its role is basically to ensure the skeletal muscle functionality.