Coagulation Guideline for Unexplained Bleeding Disorders on the Reverse Side) (Refer to Coagulation Guideline for Unexplained Bleeding Disorders on the Reverse Side)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Factor XIII and Fibrin Clot Properties in Acute Venous Thromboembolism
International Journal of Molecular Sciences Review Factor XIII and Fibrin Clot Properties in Acute Venous Thromboembolism Michał Z ˛abczyk 1,2 , Joanna Natorska 1,2 and Anetta Undas 1,2,* 1 John Paul II Hospital, 31-202 Kraków, Poland; [email protected] (M.Z.); [email protected] (J.N.) 2 Institute of Cardiology, Jagiellonian University Medical College, 31-202 Kraków, Poland * Correspondence: [email protected]; Tel.: +48-12-614-30-04; Fax: +48-12-614-21-20 Abstract: Coagulation factor XIII (FXIII) is converted by thrombin into its active form, FXIIIa, which crosslinks fibrin fibers, rendering clots more stable and resistant to degradation. FXIII affects fibrin clot structure and function leading to a more prothrombotic phenotype with denser networks, characterizing patients at risk of venous thromboembolism (VTE). Mechanisms regulating FXIII activation and its impact on fibrin structure in patients with acute VTE encompassing pulmonary embolism (PE) or deep vein thrombosis (DVT) are poorly elucidated. Reduced circulating FXIII levels in acute PE were reported over 20 years ago. Similar observations indicating decreased FXIII plasma activity and antigen levels have been made in acute PE and DVT with their subsequent increase after several weeks since the index event. Plasma fibrin clot proteome analysis confirms that clot-bound FXIII amounts associated with plasma FXIII activity are decreased in acute VTE. Reduced FXIII activity has been associated with impaired clot permeability and hypofibrinolysis in acute PE. The current review presents available studies on the role of FXIII in the modulation of fibrin clot properties during acute PE or DVT and following these events. -

Protein S Deficiency Presenting with Hemorrhage in a Term Neonate
: Curre re nt a R C e Ayari et al., Health Care Current Reviews 2018, 6:1 h v t i l e a w DOI: 10.4172/2375-4273.1000219 e s H Health Care: Current Reviews ISSN: 2375-4273 Review Article Open Access Protein S Deficiency Presenting with Hemorrhage in a Term Neonate Fairouz Ayari*, Takoua Bensmail, Essid Latifa, Wiem Barbaria and Samia Kacem Neonatology Intensive Care Unit of the Maternity and Neonatology Center, Tunis, Tunisia Abstract Unexplained bleeding symptoms in otherwise healthy full-term usually present a diagnostic challenge for treating physicians requiring prompt and accurate laboratory investigations to ensure appropriate treatment and possibly avoid long-term morbidity. We report a case of a term neonate with severe protein S deficiency manifested by systemic hemorrhage and multiple organ failure at 9 days of age. We review how protein S influences the coagulation and the fibrinolytic pathways, discussing therapeutic approaches of neonates with purpura fulminans. Keywords: Protein S deficiency; Blood sample; Thrombophilic dis- resuscitation with 20 ml/kg bodyweight (BW) saline solution and, after order blood sampling, intravenous administration of 10 mg vitamin K, 20 ml/kg BW fresh frozen plasma, 20 ml/kg BW packed red blood cells Introduction (5 transfusion cycles), 20 mg/kg BW Phenobarbital and vasoactive Protein S (PS) is an antithrombotic plasma protein that acts mainly drugs. Cerebral ultrasound revealed intraventricular haemorrhage, as a cofactor of activated protein C (APC) anticoagulant activity in the abdominal ultrasound showed splenic hemorrhage and cardiac degradation of factor Va and activated factor VIII [1]. PS circulates in ultrasound showed a floating intracardiac thrombus. -

Protein C Deficiency
Protein C deficiency Description Protein C deficiency is a disorder that increases the risk of developing abnormal blood clots; the condition can be mild or severe. Individuals with mild protein C deficiency are at risk of a type of blood clot known as a deep vein thrombosis (DVT). These clots occur in the deep veins of the arms or legs, away from the surface of the skin. A DVT can travel through the bloodstream and lodge in the lungs, causing a life-threatening blockage of blood flow known as a pulmonary embolism (PE). While most people with mild protein C deficiency never develop abnormal blood clots, certain factors can add to the risk of their development. These factors include increased age, surgery, inactivity, or pregnancy. Having another inherited disorder of blood clotting in addition to protein C deficiency can also influence the risk of abnormal blood clotting. In severe cases of protein C deficiency, infants develop a life-threatening blood clotting disorder called purpura fulminans soon after birth. Purpura fulminans is characterized by the formation of blood clots in the small blood vessels throughout the body. These blood clots block normal blood flow and can lead to localized death of body tissue ( necrosis). Widespread blood clotting uses up all available blood clotting proteins. As a result, abnormal bleeding occurs in various parts of the body, which can cause large, purple patches on the skin. Individuals who survive the newborn period may experience recurrent episodes of purpura fulminans. Frequency Mild protein C deficiency affects approximately 1 in 500 individuals. Severe protein C deficiency is rare and occurs in an estimated 1 in 4 million newborns. -

Section 8: Hematology CHAPTER 47: ANEMIA
Section 8: Hematology CHAPTER 47: ANEMIA Q.1. A 56-year-old man presents with symptoms of severe dyspnea on exertion and fatigue. His laboratory values are as follows: Hemoglobin 6.0 g/dL (normal: 12–15 g/dL) Hematocrit 18% (normal: 36%–46%) RBC count 2 million/L (normal: 4–5.2 million/L) Reticulocyte count 3% (normal: 0.5%–1.5%) Which of the following caused this man’s anemia? A. Decreased red cell production B. Increased red cell destruction C. Acute blood loss (hemorrhage) D. There is insufficient information to make a determination Answer: A. This man presents with anemia and an elevated reticulocyte count which seems to suggest a hemolytic process. His reticulocyte count, however, has not been corrected for the degree of anemia he displays. This can be done by calculating his corrected reticulocyte count ([3% × (18%/45%)] = 1.2%), which is less than 2 and thus suggestive of a hypoproliferative process (decreased red cell production). Q.2. A 25-year-old man with pancytopenia undergoes bone marrow aspiration and biopsy, which reveals profound hypocellularity and virtual absence of hematopoietic cells. Cytogenetic analysis of the bone marrow does not reveal any abnormalities. Despite red blood cell and platelet transfusions, his pancytopenia worsens. Histocompatibility testing of his only sister fails to reveal a match. What would be the most appropriate course of therapy? A. Antithymocyte globulin, cyclosporine, and prednisone B. Prednisone alone C. Supportive therapy with chronic blood and platelet transfusions only D. Methotrexate and prednisone E. Bone marrow transplant Answer: A. Although supportive care with transfusions is necessary for treating this patient with aplastic anemia, most cases are not self-limited. -

Protein C and S Deficiency in Deep Vein Thrombosis Patients Referred to Iranian Blood Transfusion Organization, Kermanshah
Protein C and S Deficiency in Deep Vein Thrombosis Patients Referred to Iranian Blood Transfusion Organization, Kermanshah Mehrdad Payandeh, 1 Mohammad Erfan Zare, 1, 2 Atefeh Nasir Kansestani, 1, 2 Kamran Ma nsouri, 1, 3 Zohreh Rahimi, 1, 4 Amir Hossein Hashemian, 5 Ebrahim Soltanian, 6 Hoshang Yousefi, 6 1Medical Biology Research Center, Kermanshah University of Medical Sciences, Kermanshah, Iran 2Student Research Committee, Kermanshah University of Medical Scien ces, Kermanshah, Iran 3Department of Molecular Medicine, School of advanced Medical Technologies, Tehran University of Medical Sciences, Tehran, Iran 4Department of Biochemistry, School of Medicine, Kermanshah University of Medical Sciences, Kermanshah, Ir an 5Department of Biostatistics, Faculty of Public Health, Kermanshah University of Medical Sciences, Kermanshah, Iran 6Research Center of Iranian Blood Transfusion Organization, Kermanshah, Iran Corresponding Author : Mohammad Erfan Zare, BSC student of M edical Lab Sciences. Medical Biology Research Center, P.O.Box: 1568, Sorkheh Lizheh, Kermanshah University of Medical Sciences, Kermanshah, Iran. E-mail : [email protected] Tel: +98 831 4276473 Fax: +98 831 4276471 Abstract Introduction: Normal homeostas is system has several inhibitor mechanisms in front of the amplifier’s natural clotting enzyme to prevent fibrin clots in the vessels. The main inhibitors of coagulation pathway are antithrombin (AT), protein C and protein S. Patients with hereditary defic iency of coagulation inhibitors are susceptible to venous thromboembolism (VTE). One of the major clinical manifestations of VTE is deep vein thrombosis (DVT). The present study has investigated the frequency of protein C and S deficiency among DVT patients that by using of these results and results from our previous study; we determined the most important hereditary risk factors for DVT in the Kermanshah Province of Iran with the Kurdish ethnic background. -
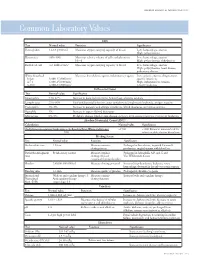
Common Laboratory Values
AmericAn AcAdemy of PediAtric dentistry Reference Manual 2006-2007 Resource Section 251 Common LaboratoryCommon Values Laboratory Values CBC Test Normal value Function Significance Hemoglobin 12-18 g/100 mL Measures oxygen carrying capacity of blood Low: hemorrhage, anemia High: polycythemia Hematocrit 35%-50% Measures relative volume of cells and plasma in Low: hemorrhage, anemia blood High: polycythemia, dehydration Red blood cell 4-6 million/mm3 Measures oxygen-carrying capacity of blood Low: hemorrhage, anemia High: polycythemia, heart disease, pulmonary disease White blood cell Measures host defense against inflammatory agents Low: aplastic anemia, drug toxicity, Infant 8,000-15,000/mm3 specific infections 4-7 y 6,000-15,000/mm3 High: inflammation, trauma, 8-18 y 4,500-13,500/mm3 toxicity, leukemia Differential Count Test Normal value Significance Neutrophils 54%-62% Increase in bacterial infections, hemorrhage, diabetic acidosis Lymphocytes 25%-30% Viral and bacterial infection, acute and chronic lymphocytic leukemia, antigen reaction Eosinophils 1%-3% Increase in parasitic and allergic conditions, blood dyscrasias, pernicious anemia Basophils 1% Increase in types of blood dyscrasias Monocytes 0%-9% Hodgkin’s disease, lipid storage disease, recovery from severe infections, monocytic leukemia Absolute Neutrophil Count (ANC) Calculation Normal value Significance (% Polymorphonuclear Leukocytes + % Bands)×Total White Cell Count >1500 <1000 Patient at increased risk for 100 infection; defer elective dental care Bleeding Screen Test -

Update on Antithrombin I (Fibrin)
©2007 Schattauer GmbH,Stuttgart AnniversaryIssueContribution Update on antithrombinI(fibrin) Michael W. Mosesson 1957–2007) The Blood Research Institute,BloodCenter of Wisconsin, Milwaukee,Wisconsin, USA y( Summary AntithrombinI(fibrin) is an important inhibitor of thrombin exosite 2.Thelatterreaction results in allostericchanges that generation that functions by sequestering thrombin in the form- down-regulate thrombin catalytic activity. AntithrombinIdefi- Anniversar ingfibrin clot,and also by reducing the catalytic activity of fibrin- ciency (afibrinogenemia), defectivethrombin binding to fibrin th boundthrombin.Thrombin binding to fibrin takesplace at two (antithrombin Idefect) found in certain dysfibrinogenemias (e.g. 50 classesofnon-substrate sites: 1) in thefibrin Edomain (two per fibrinogen Naples 1), or areduced plasma γ ’ chain content (re- molecule) throughinteractionwith thrombin exosite 1; 2) at a ducedantithrombin Iactivity),predispose to intravascular singlesite on each γ ’ chain through interaction with thrombin thrombosis. Keywords Fibrinogen,fibrin, thrombin, antithrombin I ThrombHaemost 2007; 98: 105–108 Introduction meric with respecttoits γ chains,and accounts for ~85% of human plasma fibrinogen. Thrombinbinds to its substrate, fibrinogen, through an anion- Low-affinity thrombin binding activity reflects thrombin ex- binding sitecommonlyreferred to as ‘exosite 1’ (1,2). Howell osite1bindinginEdomain of fibrin, as recentlydetailedbyana- recognized nearly acenturyago that the fibrin clot itself exhibits lysesofthrombin-fibrin -

Prolonged Partial Thromboplastin Time Without Bleeding History; Fletcher Factor Deficiency
Prolonged Partial Thromboplastin Time Without Bleeding History; Fletcher Factor Deficiency Celalettin ÜSTÜN*, Anand JILLELLA*, Linda HENDRIKS*, Mary JONAH**, Ferdane KUTLAR*, Russell BURGESS*, Abdullah KUTLAR* * Section of Hematology Oncology, Department of Medicine, Medical College of Georgia, ** Department of Pathology, Medical College of Georgia, Augusta, USA ABSTRACT A 67-year-old patient was admitted to the hospital to perform an esophagogastrectomy because a lesion at the lower esophagus was strongly suspicious for cancer. Her medical history and her family his- tory were negative for bleeding tendency or thrombosis. Her activated partial thromboplastin time (aPTT) was prolonged (44 s) whereas her prothrombin time (PT) was normal (11 s) presurgery. Mixing of her plasma with normal plasma corrected her prolonged aPTT (27.9 s). Prolonged incubation shortened the patient’s aPTT (36.3 s). Fletcher factor activity was found to be 50%. The patient underwent an esopha- gogastrectomy without bleeding complications under spinal anesthesia. Fletcher factor deficiency, a ra- re disorder, should be considered in patients who have no history of bleeding tendency with a prolonged aPTT. Surgical interventions are safe in these patients. Key Words: aPTT, Surgery, Fletcher factor, Prekallikrein. Turk J Haematol 2002;19(3): 417-419 Received: 20.06.2001 Accepted: 28.07.2001 INTRODUCTION unt[2]. Hematologists are frequently consulted for preoperative coagulation abnormalities. Preoperative evaluation of hemostasis is cru- cial to assess the risk of per-and peri-operative Prolonged aPTT is not an uncommon abnor- bleeding. The most effective screening method is mality encountered during preoperative evaluati- to obtain a thorough history of bleeding[1]. on. It may indicate the presence of antiphospholi- Preoperative screening tests mostly include acti- pid antibodies or a factor deficiency in the intrinsic vated partial thromboplastin time (aPTT), proth- and/or common pathways of blood coagulation. -

The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target
Thrombosis and Circulation Open Access Cimmino et al., J Thrombo Cir 2017, 3:1 Review Article Open Access The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target? Giovanni Cimmino*, Salvatore Fischetti and Paolo Golino Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, Naples, Italy *Corresponding author: Giovanni Cimmino, MD, PhD, Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, via Leonardo Bianchi, 180131 Naples, Italy. Tel: +39-081-7064175, Fax: +39-081-7064234; E-mail: [email protected] Received date: Dec 28, 2016, Accepted date: Jan 27, 2017, Published date: Jan 31, 2017 Copyright: © 2017 Giovanni C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Acute thrombus formation is the pathophysiological substrate underlying several clinical conditions, such as acute coronary syndrome (ACS) and stroke. Activation of coagulation cascade is a key step of the thrombotic process: vessel injury results in exposure of the glycoprotein tissue factor (TF) to the flowing blood. Once exposed, TF binds factor VII/VIIa (FVII/FVIIa) and in presence of calcium ions, it forms a tertiary complex able to activate FX to FXa, FIX to FIXa, and FVIIa itself. The final step is thrombin formation at the site of vessel injury with subsequent platelet activation, fibrinogen to fibrin conversion and ultimately thrombus formation. Platelets are the key cells in primary hemostasis. -

The Plasmin–Antiplasmin System: Structural and Functional Aspects
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Bern Open Repository and Information System (BORIS) Cell. Mol. Life Sci. (2011) 68:785–801 DOI 10.1007/s00018-010-0566-5 Cellular and Molecular Life Sciences REVIEW The plasmin–antiplasmin system: structural and functional aspects Johann Schaller • Simon S. Gerber Received: 13 April 2010 / Revised: 3 September 2010 / Accepted: 12 October 2010 / Published online: 7 December 2010 Ó Springer Basel AG 2010 Abstract The plasmin–antiplasmin system plays a key Plasminogen activator inhibitors Á a2-Macroglobulin Á role in blood coagulation and fibrinolysis. Plasmin and Multidomain serine proteases a2-antiplasmin are primarily responsible for a controlled and regulated dissolution of the fibrin polymers into solu- Abbreviations ble fragments. However, besides plasmin(ogen) and A2PI a2-Antiplasmin, a2-Plasmin inhibitor a2-antiplasmin the system contains a series of specific CHO Carbohydrate activators and inhibitors. The main physiological activators EGF-like Epidermal growth factor-like of plasminogen are tissue-type plasminogen activator, FN1 Fibronectin type I which is mainly involved in the dissolution of the fibrin K Kringle polymers by plasmin, and urokinase-type plasminogen LBS Lysine binding site activator, which is primarily responsible for the generation LMW Low molecular weight of plasmin activity in the intercellular space. Both activa- a2M a2-Macroglobulin tors are multidomain serine proteases. Besides the main NTP N-terminal peptide of Pgn physiological inhibitor a2-antiplasmin, the plasmin–anti- PAI-1, -2 Plasminogen activator inhibitor 1, 2 plasmin system is also regulated by the general protease Pgn Plasminogen inhibitor a2-macroglobulin, a member of the protease Plm Plasmin inhibitor I39 family. -

Cutaneous Findings in Patients on Anticoagulants Caleb Creswell, MD Dermatology Specialists Disclosure Information
Cutaneous findings in patients on Anticoagulants Caleb Creswell, MD Dermatology Specialists Disclosure Information • I have no financial relationships to disclose Objectives 1) Identify underlying causes of actinic or senile purpura 2) Recognize coumadin skin necrosis and understand proper treatment 3) Recognize heparin skin necrosis and understand that underlying HIT is often present Actinic (Senile) Purpura • Common on forearms of elderly individuals • Most important factor is chronic sun exposure – Thins dermal collagen and blood vessel walls • Anticoagulants may exacerbate but are rarely the main culprit Actinic Purpura Actinic Purpura Leukocytoclastic Vasculitis • Don’t mistake LCV for actinic purpura Ecchymoses • No topical agents have been shown to speed resorption of RBCs and hemosiderin • Pulsed-dye Laser can help Coumadin Induced Skin Necrosis • Coumadin: Occurs between 3-5 days after initiating therapy – Due to transient protein C deficiency – Increased risk with intrinsic protein C deficiency – Occurs in areas with significant adipose tissue – Treatment: Heparinize and continue coumadin Coumadin Induced Skin Necrosis Other Coumadin Skin Reactions • Extremely rare cause of morbilliform drug rash • Can cause leukocytoclastic vasculitis – Can occur weeks to months after starting medication Photo of Morbilliform CADR Leukocytoclastic Vasculitis Heparin Induced Skin Necrosis • Heparin: Occurs 1-14 days after starting – Often starts at injection site and spreads – Due to HIT Type II (Thrombocytopenia will be present) Heparin Induced -

RIASTAP®, Fibrinogen Concentrate (Human) Lyophilized Powder for Solution for Intravenous Injection
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------------CONTRAINDICATIONS ------------------------------------ These highlights do not include all the information needed to use RIASTAP • Known anaphylactic or severe systemic reactions to human plasma-derived products (4). safely and effectively. See full prescribing information for RIASTAP. ---------------------------------WARNINGS AND PRECAUTIONS---------------------------- RIASTAP®, Fibrinogen Concentrate (Human) • Monitor patients for early signs of anaphylaxis or hypersensitivity reactions and if necessary, discontinue administration and institute appropriate treatment (5.1). Lyophilized Powder for Solution for Intravenous Injection • Thrombotic events have been reported in patients receiving RIASTAP. Weigh the benefits of administration versus the risks of thrombosis (5.2). Initial U.S. Approval: 2009 • Because RIASTAP is made from human blood, it may carry a risk of transmitting ------------------------------------RECENT MAJOR CHANGES--------------------------------- infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent Indications and Usage (1) 06/2021 and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent (5.3). Dosage and Administration (2.2) 07/2020 -------------------------------------ADVERSE REACTIONS-------------------------------------- ----------------------------------INDICATIONS AND USAGE----------------------------------- • The most serious adverse reactions observed are thrombotic episodes (pulmonary RIASTAP, Fibrinogen