Targeting Coagulation Activation in Severe COVID-19 Pneumonia: Lessons from Bacterial Pneumonia and Sepsis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Rare Coagulation Disorders
Treatment OF HEMOPHILIA April 2006 · No. 39 THE RARE COAGULATION DISORDERS Paula HB Bolton-Maggs Department of Haematology Manchester Royal Infirmary Manchester, United Kingdom Published by the World Federation of Hemophilia (WFH) © World Federation of Hemophilia, 2006 The WFH encourages redistribution of its publications for educational purposes by not-for-profit hemophilia organizations. In order to obtain permission to reprint, redistribute, or translate this publication, please contact the Communications Department at the address below. This publication is accessible from the World Federation of Hemophilia’s web site at www.wfh.org. Additional copies are also available from the WFH at: World Federation of Hemophilia 1425 René Lévesque Boulevard West, Suite 1010 Montréal, Québec H3G 1T7 CANADA Tel. : (514) 875-7944 Fax : (514) 875-8916 E-mail: [email protected] Internet: www.wfh.org The Treatment of Hemophilia series is intended to provide general information on the treatment and management of hemophilia. The World Federation of Hemophilia does not engage in the practice of medicine and under no circumstances recommends particular treatment for specific individuals. Dose schedules and other treatment regimes are continually revised and new side effects recognized. WFH makes no representation, express or implied, that drug doses or other treatment recommendations in this publication are correct. For these reasons it is strongly recommended that individuals seek the advice of a medical adviser and/or to consult printed instructions provided by the pharmaceutical company before administering any of the drugs referred to in this monograph. Statements and opinions expressed here do not necessarily represent the opinions, policies, or recommendations of the World Federation of Hemophilia, its Executive Committee, or its staff. -
FDA Approves ZONTIVITY™ (Vorapaxar), First-In-Class PAR-1
NEWS RELEASE FDA Approves ZONTIVITY™ (vorapaxar), First-in-Class PAR-1 Antagonist, for the Reduction of Thrombotic Cardiovascular Events in Patients with a History of Heart Attack or with Peripheral Arterial Disease 5/12/2014 ZONTIVITY Added to Standard of Care Demonstrated Long-Term Benet Through Three Years Merck (NYSE:MRK), known as MSD outside the United States and Canada, today announced that the U.S. Food and Drug Administration (FDA) has approved ZONTIVITY™ (vorapaxar) for the reduction of thrombotic cardiovascular events in patients with a history of heart attack (myocardial infarction) or in patients with narrowing of leg arteries, called peripheral arterial disease (PAD). For patients with a history of heart attack or with PAD who had no history of stroke or transient ischemic attack (TIA), ZONTIVITY added to standard of care produced a signicant 17 percent relative risk reduction over the three years of the study for the combined events of cardiovascular (CV) death, myocardial infarction (MI), stroke, and urgent coronary revascularization (UCR) [event rate 10.1 percent vs. 11.8 percent for placebo]. For the key secondary composite ecacy endpoint of CV death, MI and stroke alone, ZONTIVITY produced a signicant 20 percent relative risk reduction in these patients [7.9 percent vs. 9.5 percent for placebo]. These results were driven by an 18 percent relative risk reduction in MI [5.4 percent vs. 6.4 percent for placebo] and a 33 percent relative risk reduction in rst stroke [1.2 percent vs. 1.6 percent for placebo]. The prescribing information for ZONTIVITY includes a boxed warning regarding bleeding risk. -

The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target
Thrombosis and Circulation Open Access Cimmino et al., J Thrombo Cir 2017, 3:1 Review Article Open Access The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target? Giovanni Cimmino*, Salvatore Fischetti and Paolo Golino Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, Naples, Italy *Corresponding author: Giovanni Cimmino, MD, PhD, Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, via Leonardo Bianchi, 180131 Naples, Italy. Tel: +39-081-7064175, Fax: +39-081-7064234; E-mail: [email protected] Received date: Dec 28, 2016, Accepted date: Jan 27, 2017, Published date: Jan 31, 2017 Copyright: © 2017 Giovanni C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Acute thrombus formation is the pathophysiological substrate underlying several clinical conditions, such as acute coronary syndrome (ACS) and stroke. Activation of coagulation cascade is a key step of the thrombotic process: vessel injury results in exposure of the glycoprotein tissue factor (TF) to the flowing blood. Once exposed, TF binds factor VII/VIIa (FVII/FVIIa) and in presence of calcium ions, it forms a tertiary complex able to activate FX to FXa, FIX to FIXa, and FVIIa itself. The final step is thrombin formation at the site of vessel injury with subsequent platelet activation, fibrinogen to fibrin conversion and ultimately thrombus formation. Platelets are the key cells in primary hemostasis. -

Zontivity (Vorapaxar)
HIGHLIGHTS OF PRESCRIBING INFORMATION antiplatelet drugs or with ZONTIVITY as the only antiplatelet These highlights do not include all the information needed to use agent. (2.2) ZONTIVITY safely and effectively. See full prescribing information for ZONTIVITY. --------------------- DOSAGE FORMS AND STRENGTHS --------------------- Tablets: 2.08 mg vorapaxar. (3) ZONTIVITY™ (vorapaxar) Tablets 2.08 mg*, for oral use *Equivalent to 2.5 mg vorapaxar sulfate ------------------------------- CONTRAINDICATIONS ------------------------------- Initial U.S. Approval: 2014 History of stroke, TIA, or ICH. (4.1) Active pathologic bleeding. (4.2) WARNING: BLEEDING RISK See full prescribing information for complete boxed warning. ----------------------- WARNINGS AND PRECAUTIONS ----------------------- • Do not use ZONTIVITY in patients with a history of stroke, Like other antiplatelet agents, ZONTIVITY increases the risk of transient ischemic attack (TIA), or intracranial hemorrhage (ICH); bleeding. (5.1) or active pathological bleeding. (4.1, 4.2) Avoid use with strong CYP3A inhibitors or inducers. (5.2) • Antiplatelet agents, including ZONTIVITY, increase the risk of bleeding, including ICH and fatal bleeding. (5.1) ------------------------------ ADVERSE REACTIONS ------------------------------ Bleeding, including life-threatening and fatal bleeding, is the most ----------------------------INDICATIONS AND USAGE ---------------------------- commonly reported adverse reaction. (6.1) ZONTIVITY is a protease-activated receptor-1 (PAR-1) antagonist indicated for the reduction of thrombotic cardiovascular events in To report SUSPECTED ADVERSE REACTIONS, contact Merck patients with a history of myocardial infarction (MI) or with peripheral Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877 arterial disease (PAD). ZONTIVITY has been shown to reduce the rate 888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. of a combined endpoint of cardiovascular death, MI, stroke, and urgent coronary revascularization. -

Coagulation Factors Directly Cleave SARS-Cov-2 Spike and Enhance Viral Entry
bioRxiv preprint doi: https://doi.org/10.1101/2021.03.31.437960; this version posted April 1, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Coagulation factors directly cleave SARS-CoV-2 spike and enhance viral entry. Edward R. Kastenhuber1, Javier A. Jaimes2, Jared L. Johnson1, Marisa Mercadante1, Frauke Muecksch3, Yiska Weisblum3, Yaron Bram4, Robert E. Schwartz4,5, Gary R. Whittaker2 and Lewis C. Cantley1,* Affiliations 1. Meyer Cancer Center, Department of Medicine, Weill Cornell Medical College, New York, NY, USA. 2. Department of Microbiology and Immunology, Cornell University, Ithaca, New York, USA. 3. Laboratory of Retrovirology, The Rockefeller University, New York, NY, USA. 4. Division of Gastroenterology and Hepatology, Department of Medicine, Weill Cornell Medicine, New York, NY, USA. 5. Department of Physiology, Biophysics and Systems Biology, Weill Cornell Medicine, New York, NY, USA. *Correspondence: [email protected] bioRxiv preprint doi: https://doi.org/10.1101/2021.03.31.437960; this version posted April 1, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Summary Coagulopathy is recognized as a significant aspect of morbidity in COVID-19 patients. The clotting cascade is propagated by a series of proteases, including factor Xa and thrombin. Other host proteases, including TMPRSS2, are recognized to be important for cleavage activation of SARS-CoV-2 spike to promote viral entry. Using biochemical and cell-based assays, we demonstrate that factor Xa and thrombin can also directly cleave SARS-CoV-2 spike, enhancing viral entry. -
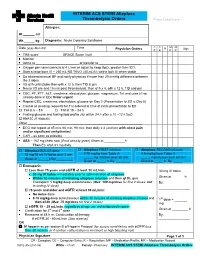
EXAMPLE Alteplase Thrombolytic Central Changes Noted
INTERIM ACS STEMI Alteplase Thrombolysis Orders Place Label Here Allergies: Ht. cm Wt. kg Diagnosis: Acute Coronary Syndrome C C M M Date (yyyy-Mon-dd) Time R Sign Physician Orders P E P R TIMI score ____________ GRACE Score (risk) ____________________ Monitor Admit to or transfer to _______________________ Oxygen per nasal cannula at 4 L/min or adjust to keep SpO2 greater than 92% Start a large bore IV – 250 mL NS TKVO (40 mL/h); saline lock IV when stable Do bilateral manual BP and notify physician if more than 20 mmHg difference between the 2 sides VS q1h until stable then q4h x 12 h, then TID & prn Neuro VS pre and 15 min post thrombolysis, then q1h x 4, q4h x 12 h, TID and prn CBC, PT, PTT, ALT, creatinine, electrolytes, glucose, magnesium, TnI and urea (if not already done in ED) Order urgent Repeat CBC, creatinine, electrolytes, glucose on Day 2 (Presentation to ED is Day 0) Cancel all pending requests for TnI ordered at time of initial presentation to ED TnI at 6 – 8 h TnI at 18 – 24 h Fasting glucose and fasting lipid profile (do within 24 h after a 10 –12 h fast) HbA1C (if diabetic) Other _______________________________________________________________ ECG stat repeat at 45 min, 60 min, 90 min: then daily x 3 (and prn with chest pain and/or significant arrhythmias) CXR – as soon as possible ASA – 162 mg chew now (if not already given) Given at h Then EC ASA 81 mg daily. Alteplase BOLUS dose Alteplase FIRST infusion Alteplase SECOND infusion 15 mg/15 mL IV bolus over 2 min 0.75 mg/kg from Table A 0.5 mg/kg from Table A _____ mg infusion over 30 min _____ mg infusion over 60 min Given at ______h By:_________ Given at _____ h By: ________ Given at _____ h By: _____ Enoxaparin Less than 75 years and eGFR at least 30 mL/min 30 mg IV bolus 30 mg IV bolus immediately prior to administration of alteplase Within 30 minutes of initiating alteplase infusion and then q12h, give Given at _______h Enoxaparin 1 mg/kg deep subcutaneous (Max. -

ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent
ALTEPLASE: Class: Thrombolytic Agent (Fibrinolytic Agent ). Indications: - Management of acute myocardial infarction for the lysis of thrombi in coronary arteries; management of acute ischemic stroke -Acute myocardial infarction (AMI): Chest pain ≥20 minutes, ≤12-24 hours; S-T elevation ≥0.1 mV in at least two ECG leads -Acute pulmonary embolism (APE): Age ≤75 years: Documented massive pulmonary embolism by pulmonary angiography or echocardiography or high probability lung scan with clinical shock . -Restoration of central venous catheter function *Unlabeled/Investigational :Acute peripheral arterial occlusive disease. Dosage: -Coronary artery thrombi: Front loading dose (weight-based): -Patients >67 kg: Total dose: 100 mg over 1.5 hours; infuse 15 mg over 1-2 minutes. Infuse 50 mg over 30 minutes. Infuse remaining 35 mg of alteplase over the next hour. Maximum total dose: 100 mg -Patients ≤67 kg: Infuse 15 mg I.V. bolus over 1-2 minutes, then infuse 0.75 mg/kg (not to exceed 50 mg) over next 30 minutes, followed by 0.5 mg/kg over next 60 minutes (not to exceed 35 mg) Maximum total dose: 100 mg. See “Notes.” Note: Concurrently, begin heparin 60 units/kg bolus (maximum: 4000 units) followed by continuous infusion of 12 units/kg/hour (maximum: 1000 units/hour) and adjust to aPTT target of 1.5-2 times the upper limit of control. Note: Thrombolytic should be administered within 30 minutes of hospital arrival. Administer concurrent aspirin, clopidogrel, and anticoagulant therapy (ie, unfractionated heparin, enoxaparin, or fondaparinux) with alteplase (O’Gara, 2013). -Acute massive or submassive pulmonary embolism: I.V. (Activase®): 100 mg over 2 hours; may be administered as a 10 mg bolus followed by 90 mg over 2 hours as was done in patients with submassive PE (Konstantinides, 2002). -

Blood Coagulation Factor X Exerts Differential Effects on Adenovirus Entry Into Human Lymphocytes
viruses Article Blood Coagulation Factor X Exerts Differential Effects on Adenovirus Entry into Human Lymphocytes James S. Findlay 1, Graham P. Cook 2 and G. Eric Blair 1,* ID 1 School of Molecular and Cellular Biology, University of Leeds, Leeds LS2 9JT, UK; jsfi[email protected] 2 Leeds Institute of Cancer and Pathology, University of Leeds, St. James’s University Hospital, Leeds LS9 7TF, UK; [email protected] * Correspondence: [email protected]; Tel.: +44-113-343-3128 Received: 5 December 2017; Accepted: 30 December 2017; Published: 3 January 2018 Abstract: It has been proposed that blood coagulation factors, principally factor X (FX), enhance the uptake of human adenovirus type 5 (Ad5) into cultured epithelial cells by bridging the viral hexon capsid protein and cell-surface heparan sulphate proteoglycans (HSPGs). We studied the effects of FX on Ad transduction of lymphoid cell lines (NK92MI, a natural killer cell line; Daudi, a B-cell line and Jurkat, a T-cell line) as well as primary peripheral blood lymphocytes (PBL) and HeLa epithelial cells using either replication-deficient Ad5, or a derivative in which the Ad5 fiber was replaced with that of another Ad type, Ad35, termed Ad5F35. PBL and NK92MI were resistant to Ad5 transduction. Transduction of Jurkat and Daudi cells by Ad5 was reduced by FX but without discernible effects on cell-surface Ad5 binding. FX reduced virus binding and transduction of all lymphoid cell lines by Ad5F35, as well as transduction of the T- and Natural Killer (NK)-cell populations of PBL. Flow cytometry analysis showed that all lymphoid cell lines were negative for HSPG components, in contrast to HeLa cells. -

RIASTAP®, Fibrinogen Concentrate (Human) Lyophilized Powder for Solution for Intravenous Injection
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------------CONTRAINDICATIONS ------------------------------------ These highlights do not include all the information needed to use RIASTAP • Known anaphylactic or severe systemic reactions to human plasma-derived products (4). safely and effectively. See full prescribing information for RIASTAP. ---------------------------------WARNINGS AND PRECAUTIONS---------------------------- RIASTAP®, Fibrinogen Concentrate (Human) • Monitor patients for early signs of anaphylaxis or hypersensitivity reactions and if necessary, discontinue administration and institute appropriate treatment (5.1). Lyophilized Powder for Solution for Intravenous Injection • Thrombotic events have been reported in patients receiving RIASTAP. Weigh the benefits of administration versus the risks of thrombosis (5.2). Initial U.S. Approval: 2009 • Because RIASTAP is made from human blood, it may carry a risk of transmitting ------------------------------------RECENT MAJOR CHANGES--------------------------------- infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent Indications and Usage (1) 06/2021 and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent (5.3). Dosage and Administration (2.2) 07/2020 -------------------------------------ADVERSE REACTIONS-------------------------------------- ----------------------------------INDICATIONS AND USAGE----------------------------------- • The most serious adverse reactions observed are thrombotic episodes (pulmonary RIASTAP, Fibrinogen -

Urokinase and Urokinase Receptor in the Urinary Tract of the Dog Trina Racquel Bailey Louisiana State University and Agricultural and Mechanical College
Louisiana State University LSU Digital Commons LSU Master's Theses Graduate School 2005 Urokinase and urokinase receptor in the urinary tract of the dog Trina Racquel Bailey Louisiana State University and Agricultural and Mechanical College Follow this and additional works at: https://digitalcommons.lsu.edu/gradschool_theses Part of the Veterinary Medicine Commons Recommended Citation Bailey, Trina Racquel, "Urokinase and urokinase receptor in the urinary tract of the dog" (2005). LSU Master's Theses. 1457. https://digitalcommons.lsu.edu/gradschool_theses/1457 This Thesis is brought to you for free and open access by the Graduate School at LSU Digital Commons. It has been accepted for inclusion in LSU Master's Theses by an authorized graduate school editor of LSU Digital Commons. For more information, please contact [email protected]. UROKINASE AND UROKINASE RECEPTOR IN THE URINARY TRACT OF THE DOG A Thesis Submitted to the Graduate Faculty of the Louisiana State University and Agricultural and Mechanical College in partial fulfillment of the requirements for the degree of Master of Science In The Interdepartmental Program in Veterinary Medical Sciences through the Department of Veterinary Clinical Sciences by Trina Racquel Bailey BSc, Doctor of Veterinary Medicine Atlantic Veterinary College, University of Prince Edward Island, 2000 December 2005 To my husband John, who has been there to help me through it all. To my son Ewan, who makes everything worthwhile. To my family and family in law for all their love, help and support. To Dude, Bailey, Sarah, Scamp, Ellie, Abby, and all the other wonderful animals who have been there for me to love and have allowed me to learn. -

Platelet Surface Glycoproteins. Studies on Resting and Activated Platelets and Platelet Membrane Microparticles in Normal Subjec
Platelet surface glycoproteins. Studies on resting and activated platelets and platelet membrane microparticles in normal subjects, and observations in patients during adult respiratory distress syndrome and cardiac surgery. J N George, … , N Kieffer, P J Newman J Clin Invest. 1986;78(2):340-348. https://doi.org/10.1172/JCI112582. Research Article The accurate definition of surface glycoprotein abnormalities in circulating platelets may provide better understanding of bleeding and thrombotic disorders. Platelet surface glycoproteins were measured on intact platelets in whole blood and platelet membrane microparticles were assayed in cell-free plasma using 125I-monoclonal antibodies. The glycoproteins (GP) studied were: GP Ib and GP IIb-IIIa, two of the major intrinsic plasma membrane glycoproteins; GMP-140, an alpha- granule membrane glycoprotein that becomes exposed on the platelet surface following secretion; and thrombospondin (TSP), an alpha-granule secreted glycoprotein that rebinds to the platelet surface. Thrombin-induced secretion in normal platelets caused the appearance of GMP-140 and TSP on the platelet surface, increased exposure of GP IIb-IIIa, and decreased antibody binding to GP Ib. Patients with adult respiratory distress syndrome had an increased concentration of GMP-140 and TSP on the surface of their platelets, demonstrating in vivo platelet secretion, but had no increase of platelet microparticles in their plasma. In contrast, patients after cardiac surgery with cardiopulmonary bypass demonstrated changes consistent with membrane fragmentation without secretion: a decreased platelet surface concentration of GP Ib and GP IIb with no increase of GMP-140 and TSP, and an increased plasma concentration of platelet membrane microparticles. These methods will help to define acquired abnormalities of platelet surface glycoproteins. -

ACTIVASE (Alteplase) for Injection, for Intravenous Use Initial U.S
Application 103172 This document contains: Label for ACTIVASE [Supplement 5203, Action Date 02/13/2015] Also available: Label for CATHFLO ACTIVASE [Supplement 5071, Action Date 01/04/2005] HIGHLIGHTS OF PRESCRIBING INFORMATION Acute Ischemic Stroke These highlights do not include all the information needed to use • Current intracranial hemorrhage. (4.1) ACTIVASE safely and effectively. See full prescribing information for • Subarachnoid hemorrhage. (4.1) ACTIVASE. Acute Myocardial Infarction or Pulmonary Embolism • History of recent stroke. (4.2) ACTIVASE (alteplase) for injection, for intravenous use Initial U.S. Approval: 1987 -----------------------WARNINGS AND PRECAUTIONS----------------------- • Increases the risk of bleeding. Avoid intramuscular injections. Monitor for ---------------------------INDICATIONS AND USAGE-------------------------- bleeding. If serious bleeding occurs, discontinue Activase. (5.1) Activase is a tissue plasminogen activator (tPA) indicated for the treatment of • Monitor patients during and for several hours after infusion for orolingual • Acute Ischemic Stroke (AIS). (1.1) angioedema. If angioedema develops, discontinue Activase. (5.2) • Acute Myocardial Infarction (AMI) to reduce mortality and incidence of • Cholesterol embolism has been reported rarely in patients treated with heart failure. (1.2) thrombolytic agents. (5.3) Limitation of Use in AMI: the risk of stroke may be greater than the benefit • Consider the risk of reembolization from the lysis of underlying deep in patients at low risk of death