Guidelines for Burn Care Under Austere Conditions: Special Etiologies: Blast, Radiation, and Chemical Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recognizing When a Child's Injury Or Illness Is Caused by Abuse
U.S. Department of Justice Office of Justice Programs Office of Juvenile Justice and Delinquency Prevention Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE U.S. Department of Justice Office of Justice Programs 810 Seventh Street NW. Washington, DC 20531 Eric H. Holder, Jr. Attorney General Karol V. Mason Assistant Attorney General Robert L. Listenbee Administrator Office of Juvenile Justice and Delinquency Prevention Office of Justice Programs Innovation • Partnerships • Safer Neighborhoods www.ojp.usdoj.gov Office of Juvenile Justice and Delinquency Prevention www.ojjdp.gov The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs, which also includes the Bureau of Justice Assistance; the Bureau of Justice Statistics; the National Institute of Justice; the Office for Victims of Crime; and the Office of Sex Offender Sentencing, Monitoring, Apprehending, Registering, and Tracking. Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE NCJ 243908 JULY 2014 Contents Could This Be Child Abuse? ..............................................................................................1 Caretaker Assessment ......................................................................................................2 Injury Assessment ............................................................................................................4 Ruling Out a Natural Phenomenon or Medical Conditions -
Protecting Workers from Cold Stress
QUICK CARDTM Protecting Workers from Cold Stress Cold temperatures and increased wind speed (wind chill) cause heat to leave the body more quickly, putting workers at risk of cold stress. Anyone working in the cold may be at risk, e.g., workers in freezers, outdoor agriculture and construction. Common Types of Cold Stress Hypothermia • Normal body temperature (98.6°F) drops to 95°F or less. • Mild Symptoms: alert but shivering. • Moderate to Severe Symptoms: shivering stops; confusion; slurred speech; heart rate/breathing slow; loss of consciousness; death. Frostbite • Body tissues freeze, e.g., hands and feet. Can occur at temperatures above freezing, due to wind chill. May result in amputation. • Symptoms: numbness, reddened skin develops gray/ white patches, feels firm/hard, and may blister. Trench Foot (also known as Immersion Foot) • Non-freezing injury to the foot, caused by lengthy exposure to wet and cold environment. Can occur at air temperature as high as 60°F, if feet are constantly wet. • Symptoms: redness, swelling, numbness, and blisters. Risk Factors • Dressing improperly, wet clothing/skin, and exhaustion. For Prevention, Your Employer Should: • Train you on cold stress hazards and prevention. • Provide engineering controls, e.g., radiant heaters. • Gradually introduce workers to the cold; monitor workers; schedule breaks in warm areas. For more information: U.S. Department of Labor www.osha.gov (800) 321-OSHA (6742) 2014 OSHA 3156-02R QUICK CARDTM How to Protect Yourself and Others • Know the symptoms; monitor yourself and co-workers. • Drink warm, sweetened fluids (no alcohol). • Dress properly: – Layers of loose-fitting, insulating clothes – Insulated jacket, gloves, and a hat (waterproof, if necessary) – Insulated and waterproof boots What to Do When a Worker Suffers from Cold Stress For Hypothermia: • Call 911 immediately in an emergency. -

Management of Specific Wounds
7 Management of Specific Wounds Bite Wounds 174 Hygroma 234 Burns 183 Snakebite 239 Inhalation Injuries 195 Brown Recluse Spider Bites 240 Chemical Burns 196 Porcupine Quills 240 Electrical Injuries 197 Lower Extremity Shearing Wounds 243 Radiation Injuries 201 Plate 10: Pipe Insulation Protective Frostbite 204 Device: Elbow 248 Projectile Injuries 205 Plate 11: Pipe Insulation to Protect Explosive Munitions: Ballistic, the Greater Trochanter 250 Blast, and Thermal Injuries 227 Plate 12: Vacuum Drain Impalement Injuries 227 Management of Elbow Pressure Ulcers 228 Hygromas 252 Atlas of Small Animal Wound Management and Reconstructive Surgery, Fourth Edition. Michael M. Pavletic. © 2018 John Wiley & Sons, Inc. Published 2018 by John Wiley & Sons, Inc. Companion website: www.wiley.com/go/pavletic/atlas 173 174 Atlas of Small Animal Wound Management and Reconstructive Surgery BITE WOUNDS to the skin. Wounds may be covered by a thick hair coat and go unrecognized. The skin and underlying Introduction issues can be lacerated, stretched, crushed, and avulsed. Circulatory compromise from the division of vessels and compromise to collateral vascular channels can result in Bite wounds are among the most serious injuries seen in massive tissue necrosis. It may take several days before small animal practice, and can account for 10–15% of all the severity of tissue loss becomes evident. All bites veterinary trauma cases. The canine teeth are designed are considered contaminated wounds: the presence of for tissue penetration, the incisors for grasping, and the bacteria in the face of vascular compromise can precipi- molars/premolars for shearing tissue. The curved canine tate massive infection. teeth of large dogs are capable of deep penetration, whereas the smaller, straighter canine teeth of domestic cats can penetrate directly into tissues, leaving a rela- tively small cutaneous hole. -
Training for Radiation Emergencies: First Responder Operations
TRAINING FOR RADIATION EMERGENCIES: FIRST RESPONDER OPERATIONS STUDENT TEXT Developed by THE INTERNATIONAL ASSOCIATION OF FIRE FIGHTERS ® Alfred K. Whitehead Vincent J. Bollon General President General Secretary-Treasurer Copyright © 1998 International Association of Fire Fighters 1750 New York Avenue, N.W. Washington, D.C. 20006 THE INTERNATIONAL ASSOCIATION OF FIRE FIGHTERS ® Alfred K. Whitehead Vincent J. Bollon General President General Secretary-Treasurer Bradley M. Sant, Director Hazardous Materials Training The IAFF acknowledges the Hazardous Materials Training staff: Kimberly Lockhart, Michael Lucey, Diane Dix Massa, A. Christopher Miklovis, Carol Mintz, Michael Schaitberger, Scott Solomon, Linda Voelpel Casey, and consultants Jo Griffith, Eric Lamar, and Margaret Veroneau for their work in developing this manual. In addition, the IAFF thanks Paul Deane,Tommy Erickson, and Charlie Wright for their contributions to this project. Notice This manual was prepared as an account of work sponsored by an agency of the United States Government. Neither the United States government nor any agency thereof, nor any of their employees, nor any of their contractors, subcontractors nor their employees, make any warranty, expressed or implied, or assume any legal liability or responsibility for the accuracy, completeness, or usefulness of any information, apparatus, product, or process disclosed, or represent that its use would not infringe upon privately-owned rights. Reference herein to any specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise, does not necessarily constitute or imply its endorsement, recommendation, or favoring by the United States Government or any agency thereof. The views and opinions of authors expressed herein do not necessarily state or reflect those of the United States Government or any agency thereof. -

Help Individuals with Spinal Cord Injury, Traumatic Brain Injury, And
Help Individuals with Spinal Cord Injury, Traumatic Brain Injury, and Burn Injury Stay Healthy during the COVID-19 Pandemic Model Systems Knowledge Translation Center (MSKTC) Xinsheng “Cindy” Cai, PhD MSKTC Project Director American Institutes for Research Disclosures • The contents of this presentation were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90DP0082). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this presentation do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government. 2 Learning Objectives • Use the free research-based resources developed by the Model Systems Knowledge Translation Center (MSKTC) to help individuals living with spinal cord injury (SCI), traumatic brain injury (TBI), and burn injury to stay healthy during the COVID-19 pandemic • Understand how the MSKTC has worked with Model System researchers to apply a knowledge translation (KT) framework to make these resources useful to the end-users • Understand principles in effectively communicating health information to support individuals with SCI, TBI, and burn injuries 3 Session Overview • Model Systems Knowledge Translation Center (MSKTC) background • Example MSKTC resources to help individuals with spinal cord injury (SCI), traumatic brain injury (TBI) and burn to stay healthy during the COVID-19 pandemic • KT strategies -

Chapter 32 FOREIGN BODIES of the HEAD, NECK, and SKULL BASE
Foreign Bodies of the Head, Neck, and Skull Base Chapter 32 FOREIGN BODIES OF THE HEAD, NECK, AND SKULL BASE RICHARD J. BARNETT, MD* INTRODUCTION PENETRATING NECK TRAUMA Anatomy Emergency Management Clinical Examination Investigations OPERATIVE VERSUS NONOPERATIVE MANAGEMENT Factors in the Deployed Setting Operative Management Postoperative Care PEDIATRIC INJURIES ORBITAL FOREIGN BODIES SUMMARY CASE PRESENTATIONS Case Study 32-1 Case Study 32-2 Case Study 32-3 Case Study 32-4 Case Study 32-5 Case Study 32-6 *Lieutenant Colonel, Medical Corps, US Air Force; Chief of Facial Plastic Surgery/Otolaryngology, Eglin Air Force Base Department of ENT, 307 Boatner Road, Suite 114, Eglin Air Force Base, Florida 32542-9998 423 Otolaryngology/Head and Neck Combat Casualty Care INTRODUCTION The mechanism and extent of war injuries are sig- other military conflicts. In a study done in Croatia with nificantly different from civilian trauma. Many of the 117 patients who sustained penetrating neck injuries, wounds encountered are unique and not experienced about a quarter of the wounds were from gunshots even at Role 1 trauma centers throughout the United while the rest were from shell or bomb shrapnel.1 The States. Deployed head and neck surgeons must be injury patterns resulting from these mechanisms can skilled at performing an array of evaluations and op- vary widely, and treating each injury requires thought- erations that in many cases they have not performed in ful planning to achieve a successful outcome. a prior setting. During a 6-month tour in Afghanistan, This chapter will address penetrating neck injuries all subspecialties of otolaryngology were encountered: in general, followed specifically by foreign body inju- head and neck (15%), facial plastic/reconstructive ries of the head, face, neck, and skull base. -

Radiation Burn / Dermatitis, Chemical Burn & Necrobiosis Lipodica Case Studies
Radiation Burn / Dermatitis, Chemical Burn & Necrobiosis Lipodica Case Studies By: Jeanne Alvarez, FNP, CWS, Independent Medical Associates, Bangor, ME Radiation Burn / Dermatitis Case Study 1: 63 year old female S/P lumpectomy with chemotherapy and radiation to the breast. She developed a burn to the area with noted dermatitis at the completion of radiation treatments. Area was very painful and blistered. Hydrofera Blue radiation dressing was applied and held in place with netting. There was significant pain reduction reported within hours of application. Wounds healed in 17 days of starting therapy. Started Healed in 17 Days Radiation Burn / Dermatitis Case Study 2: 85 year old male S/P excision of Squamous cell carcinoma of the right temple x 2, the second excision prompted the surgeon to treat area with radiation. The radiation caused the patient’s skin to burn and develop a dermatitis surrounding the wound. Started Hydrofera Blue on patient and he healed in 83 days. Started Healed in 83 Days Chemical Burn Necrobiosis Lipodica Case Study 1: 57 year old male spraying Case Study 1: 48 year old female with wounds on shins. Wounds present for 3 years. insecticide containing the cyhalothrin, Treated at wound care center and given diagnosis of pyoderma gangrenosum, tried came into contact with hands and arms. multiple treatments resulting in thick black and flesh colored eschar which festered and Flushed area with water after contact. drained on regular basis. Wounds did not resemble pyoderma gangrenosum, debrided Within 24 hours of exposure, developed eschar and obtained biopsy, which provided diagnosis of necrobiosis lipodica. Work-up for painful 10/10 blisters. -

Child Abuse: Skin Markers and Differential Diagnosis
527 527 REVISÃO L Violência contra a criança: indicadores dermatológicos e diagnósticos diferenciais* Child abuse: skin markers and differential diagnosis Roberta Marinho Falcão Gondim 1 Daniel Romero Muñoz 2 Valeria Petri 3 Resumo: As denúncias de abuso contra a criança têm sido frequentes e configuram grave problema de saúde pública. O tema é desconfortável para muitos médicos, seja pelo treinamento insuficiente, seja pelo desconhecimento das dimensões do problema. Uma das formas mais comuns de violência contra a criança é o abuso físico. Como órgão mais exposto e extenso, a pele é o alvo mais sujeito aos maus- tratos. Equimoses e queimaduras são os sinais mais visíveis. Médicos (pediatras, clínicos-gerais e derma- tologistas) costumam ser os primeiros profissionais a observar e reconhecer sinais de lesões não aciden- tais ou intencionais. Os dermatologistas podem auxiliar na distinção entre lesões traumáticas inten- cionais, acidentais e doenças cutâneas que mimetizam maus-tratos. Palavras-chave: Contusões; Equimose; Queimaduras; Violência doméstica; Violência sexual Abstract: Reports of child abuse have increased significantly. The matter makes most physicians uncom- fortable for two reasons: a) Little guidance or no training in recognizing the problem; b - Not under- standing its true dimension. The most common form of child violence is physical abuse. The skin is the largest and frequently the most traumatized organ. Bruises and burns are the most visible signs. Physicians (pediatricians, general practitioners and dermatologists) -

Bruises- Wounds
Henry Shih OD, MD Medical Director Austin Emergency Center- Anderson Mill 13435 US Highway 183 North Suite 311 Austin, TX 78750 512-614-1200 BRUISES- http://austiner.com/ What are bruises? — Bruises happen when blood vessels under the skin break, but the skin isn’t cut. Blood leaks into the tissues under the skin. Bruises start off red in color, and then turn blue or purple. As they heal, bruises can turn green and yellow. Most bruises heal in 1 to 2 weeks, but some take longer. How are bruises treated? — A bruise will get better on its own. But to feel better and help your bruise heal, you can: o Put a cold gel pack, bag of ice, or bag of frozen vegetables on the injured area every 1 to 2 hours, for 15 minutes each time. Put a thin towel between the ice (or other cold object) and your skin. Use the ice (or other cold object) for at least 6 hours after your injury. Some people find it helpful to ice longer, even up to 2 days after their injury. o Raise the area, if possible – Raising the area above the level of your heart helps to reduce swelling. o Take medicine to reduce the pain and swelling – To treat pain, you can take Tylenol. To treat pain and swelling, you can take ibuprofen (sample brand names: Advil, Motrin). But people who have certain conditions or take certain medicines should not take ibuprofen. If you are unsure, ask your doctor or nurse if you can take ibuprofen. -
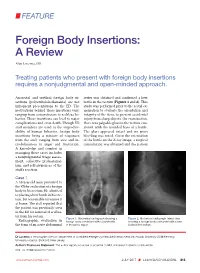
Foreign Body Insertions: a Review
FEATURE Foreign Body Insertions: A Review Alan Lucerna, DO Treating patients who present with foreign body insertions requires a nonjudgmental and open-minded approach. Anorectal and urethral foreign body in- series was obtained and confirmed a beer sertions (polyembolokoilamania) are not bottle in the rectum (Figures 1 and 2). This infrequent presentations to the ED. The study was performed prior to the rectal ex- motivations behind these insertions vary, amination to evaluate the orientation and ranging from autoeroticism to reckless be- integrity of the item, to prevent accidental havior. These insertions can lead to major injury from sharp objects. On examination, complications and even death. Though ED there was palpable glass in the rectum con- staff members are used to the unpredict- sistent with the rounded base of a bottle. ability of human behavior, foreign body The glass appeared intact and no gross insertions bring a mixture of responses bleeding was noted. Given the orientation from the staff, ranging from awe and in- of the bottle on the X-ray image, a surgical credulousness to anger and frustration. consultation was obtained and the patient A knowledge and comfort in managing these cases includes a nonjudgmental triage assess- ment, collective professional- ism, and self-awareness of the staff’s reaction. Case 1 A 58-year-old man presented to the ED for evaluation of a foreign body in his rectum. He admitted to placing a beer bottle in his rec- tum, but was unable to remove it at home. The staff reported that the patient was previously seen in the ED for removal of a vibra- tor from his rectum. -

Foreign Rectal Body – Systematic Review and Meta-Analysis
REVIEW 61 Foreign rectal body – Systematic review and meta-analysis M. Ploner1, A. Gardetto2, F. Ploner3, M. Scharl4, S. Shoap5, H. C. Bäcker5 (1) Department of Anesthesiology and Intensiver Care, Cantonal Spital Lucerne, Lucerne, Switzerland ; (2) Department of Plastic Surgery, Hospital Sterzing, Sterzing, South Tirol, Italy ; (3) Department of Anesthesiology and Emergency Medicine, Hospital Sterzing, South Tirol, Italy ; (4) Department of Gastroenterology and Hepatology, University Hospital Zurich, University of Zurich, Swetzerland ; (5) Department of Orthopaedic Surgery, Columbia University Medical Center, New York, USA. Abstract instrumentation (7). The most common complication is a rectal injury, which can result from a variety of agents and Background : Self-inserted foreign rectal bodies are an objects (8). Often, nonsurgical removal of foreign bodies infrequent occurrence, however they present a serious dilemma to the surgeon, due to the variety of objects, and the difficulty of has been described to be successful – in 11% to 65% – extraction. The purpose of this study is to give a comprehensive (9), however, in many situations, a surgical treatment review of the literature regarding the epidemiology, diagnostic may be essential. There have been a variety of algorithms tools and therapeutic approaches of foreign rectal body insertion. Methods : A comprehensive systematic literature review on introduced for the management of extraction, however, Pubmed/ Medline and Google for ‘foreign bodies’ was performed because of the diversity of foreign bodies, improvisation, on January 14th 2018. A meta-analysis was carried out to evaluate as well creativity of the treating emergency physician the epidemiology, diagnostics and therapeutic techniques. 1,551 abstracts were identified, of which 54 articles were included. -
NEISS Coding Manual January 2018
NNEEIISSSS CCooddiinngg MMaannuuaall JJaannuuaarryy 22001188 NEISS – National Electronic Injury Surveillance System January 2018 Table of Contents Introduction ................................................................................................................................................. 1 General Instructions ................................................................................................................................... 1 General NEISS Reporting Rule .................................................................................................................. 1 Do Report .................................................................................................................................................. 1 Definitions .............................................................................................................................................. 2 Do Not Report ........................................................................................................................................... 3 Specific Coding Instructions ..................................................................................................................... 4 Medical Information Codes ........................................................................................................................ 4 Date of Treatment ..................................................................................................................................... 4 (8 spaces).................................................................................................................................................