Platelet Surface Glycoproteins. Studies on Resting and Activated Platelets and Platelet Membrane Microparticles in Normal Subjec
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Platelet Membrane Glycoproteins: a Historical Review*
577 Platelet Membrane Glycoproteins: A Historical Review* Alan T. Nurden, PhD1 1 L’Institut de Rhythmologie et Modélisation Cardiaque (LIRYC), Address for correspondence Alan T. Nurden, PhD, L’Institut de Plateforme Technologique et d’Innovation Biomédicale (PTIB), Rhythmologie et Modélisation Cardiaque, Plateforme Technologique Hôpital Xavier Arnozan, Pessac, France et d’Innovation Biomédicale, Hôpital Xavier Arnozan, Avenue du Haut- Lévèque, 33600 Pessac, France (e-mail: [email protected]). Semin Thromb Hemost 2014;40:577–584. Abstract The search for the components of the platelet surface that mediate platelet adhesion and platelet aggregation began for earnest in the late 1960s when electron microscopy demonstrated the presence of a carbohydrate-rich, negatively charged outer coat that was called the “glycocalyx.” Progressively, electrophoretic procedures were developed that identified the major membrane glycoproteins (GP) that constitute this layer. Studies on inherited disorders of platelets then permitted the designation of the major effectors of platelet function. This began with the discovery in Paris that platelets of patients with Glanzmann thrombasthenia, an inherited disorder of platelet aggregation, Keywords lacked two major GP. Subsequent studies established the role for the GPIIb-IIIa complex ► platelet (now known as integrin αIIbβ3)inbindingfibrinogen and other adhesive proteins on ► inherited disorder activated platelets and the formation of the protein bridges that join platelets together ► membrane in the platelet aggregate. This was quickly followed by the observation that platelets of glycoproteins patients with the Bernard–Soulier syndrome, with macrothrombocytopenia and a ► Glanzmann distinct disorder of platelet adhesion, lacked the carbohydrate-rich, negatively charged, thrombasthenia GPIb. It was shown that GPIb, through its interaction with von Willebrand factor, ► Bernard–Soulier mediated platelet attachment to injured sites in the vessel wall. -

Surface Glycoproteomic Analysis of Hepatocellular Carcinoma Cells by Affinity Enrichment and Mass Spectrometric Identification
Glycoconj J (2012) 29:411–424 DOI 10.1007/s10719-012-9420-3 Surface glycoproteomic analysis of hepatocellular carcinoma cells by affinity enrichment and mass spectrometric identification Wei Mi & Wei Jia & Zhaobin Zheng & Jinglan Wang & Yun Cai & Wantao Ying & Xiaohong Qian Received: 14 April 2012 /Revised: 5 June 2012 /Accepted: 12 June 2012 /Published online: 1 July 2012 # Springer Science+Business Media, LLC 2012 Abstract Cell surface glycoproteins are one of the most surface-capturing (CSC) technique was an approach specif- frequently observed phenomena correlated with malignant ically targeted at membrane glycoproteins involving the growth. Hepatocellular carcinoma (HCC) is one of the most affinity capture of membrane glycoproteins using glycan malignant tumors in the world. The majority of hepatocel- biotinylation labeling on intact cell surfaces. To characterize lular carcinoma cell surface proteins are modified by glyco- the cell surface glycoproteome and probe the mechanism of sylation in the process of tumor invasion and metastasis. tumor invasion and metastasis of HCC, we have modified Therefore, characterization of cell surface glycoproteins can and evaluated the cell surface-capturing strategy, and ap- provide important information for diagnosis and treatment plied it for surface glycoproteomic analysis of hepatocellu- of liver cancer, and also represent a promising source of lar carcinoma cells. In total, 119 glycosylation sites on 116 potential diagnostic biomarkers and therapeutic targets for unique glycopeptides were identified, corresponding to 79 hepatocellular carcinoma. However, cell surface glycopro- different protein species. Of these, 65 (54.6 %) new pre- teins of HCC have been seldom identified by proteomics dicted glycosylation sites were identified that had not pre- approaches because of their hydrophobic nature, poor solu- viously been determined experimentally. -

ADAM10 Site-Dependent Biology: Keeping Control of a Pervasive Protease
International Journal of Molecular Sciences Review ADAM10 Site-Dependent Biology: Keeping Control of a Pervasive Protease Francesca Tosetti 1,* , Massimo Alessio 2, Alessandro Poggi 1,† and Maria Raffaella Zocchi 3,† 1 Molecular Oncology and Angiogenesis Unit, IRCCS Ospedale Policlinico S. Martino Largo R. Benzi 10, 16132 Genoa, Italy; [email protected] 2 Proteome Biochemistry, IRCCS San Raffaele Scientific Institute, 20132 Milan, Italy; [email protected] 3 Division of Immunology, Transplants and Infectious Diseases, IRCCS San Raffaele Scientific Institute, 20132 Milan, Italy; [email protected] * Correspondence: [email protected] † These authors contributed equally to this work as last author. Abstract: Enzymes, once considered static molecular machines acting in defined spatial patterns and sites of action, move to different intra- and extracellular locations, changing their function. This topological regulation revealed a close cross-talk between proteases and signaling events involving post-translational modifications, membrane tyrosine kinase receptors and G-protein coupled recep- tors, motor proteins shuttling cargos in intracellular vesicles, and small-molecule messengers. Here, we highlight recent advances in our knowledge of regulation and function of A Disintegrin And Metalloproteinase (ADAM) endopeptidases at specific subcellular sites, or in multimolecular com- plexes, with a special focus on ADAM10, and tumor necrosis factor-α convertase (TACE/ADAM17), since these two enzymes belong to the same family, share selected substrates and bioactivity. We will discuss some examples of ADAM10 activity modulated by changing partners and subcellular compartmentalization, with the underlying hypothesis that restraining protease activity by spatial Citation: Tosetti, F.; Alessio, M.; segregation is a complex and powerful regulatory tool. -

The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target
Thrombosis and Circulation Open Access Cimmino et al., J Thrombo Cir 2017, 3:1 Review Article Open Access The Two Faces of Thrombosis: Coagulation Cascade and Platelet Aggregation. Are Platelets the Main Therapeutic Target? Giovanni Cimmino*, Salvatore Fischetti and Paolo Golino Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, Naples, Italy *Corresponding author: Giovanni Cimmino, MD, PhD, Department of Cardio-Thoracic and Respiratory Sciences, Section of Cardiology, University of Campania “Luigi Vanvitelli”, via Leonardo Bianchi, 180131 Naples, Italy. Tel: +39-081-7064175, Fax: +39-081-7064234; E-mail: [email protected] Received date: Dec 28, 2016, Accepted date: Jan 27, 2017, Published date: Jan 31, 2017 Copyright: © 2017 Giovanni C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Acute thrombus formation is the pathophysiological substrate underlying several clinical conditions, such as acute coronary syndrome (ACS) and stroke. Activation of coagulation cascade is a key step of the thrombotic process: vessel injury results in exposure of the glycoprotein tissue factor (TF) to the flowing blood. Once exposed, TF binds factor VII/VIIa (FVII/FVIIa) and in presence of calcium ions, it forms a tertiary complex able to activate FX to FXa, FIX to FIXa, and FVIIa itself. The final step is thrombin formation at the site of vessel injury with subsequent platelet activation, fibrinogen to fibrin conversion and ultimately thrombus formation. Platelets are the key cells in primary hemostasis. -

RIASTAP®, Fibrinogen Concentrate (Human) Lyophilized Powder for Solution for Intravenous Injection
HIGHLIGHTS OF PRESCRIBING INFORMATION -------------------------------------CONTRAINDICATIONS ------------------------------------ These highlights do not include all the information needed to use RIASTAP • Known anaphylactic or severe systemic reactions to human plasma-derived products (4). safely and effectively. See full prescribing information for RIASTAP. ---------------------------------WARNINGS AND PRECAUTIONS---------------------------- RIASTAP®, Fibrinogen Concentrate (Human) • Monitor patients for early signs of anaphylaxis or hypersensitivity reactions and if necessary, discontinue administration and institute appropriate treatment (5.1). Lyophilized Powder for Solution for Intravenous Injection • Thrombotic events have been reported in patients receiving RIASTAP. Weigh the benefits of administration versus the risks of thrombosis (5.2). Initial U.S. Approval: 2009 • Because RIASTAP is made from human blood, it may carry a risk of transmitting ------------------------------------RECENT MAJOR CHANGES--------------------------------- infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent Indications and Usage (1) 06/2021 and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent (5.3). Dosage and Administration (2.2) 07/2020 -------------------------------------ADVERSE REACTIONS-------------------------------------- ----------------------------------INDICATIONS AND USAGE----------------------------------- • The most serious adverse reactions observed are thrombotic episodes (pulmonary RIASTAP, Fibrinogen -

Factor V Leiden Thrombophilia
Factor V Leiden thrombophilia Description Factor V Leiden thrombophilia is an inherited disorder of blood clotting. Factor V Leiden is the name of a specific gene mutation that results in thrombophilia, which is an increased tendency to form abnormal blood clots that can block blood vessels. People with factor V Leiden thrombophilia have a higher than average risk of developing a type of blood clot called a deep venous thrombosis (DVT). DVTs occur most often in the legs, although they can also occur in other parts of the body, including the brain, eyes, liver, and kidneys. Factor V Leiden thrombophilia also increases the risk that clots will break away from their original site and travel through the bloodstream. These clots can lodge in the lungs, where they are known as pulmonary emboli. Although factor V Leiden thrombophilia increases the risk of blood clots, only about 10 percent of individuals with the factor V Leiden mutation ever develop abnormal clots. The factor V Leiden mutation is associated with a slightly increased risk of pregnancy loss (miscarriage). Women with this mutation are two to three times more likely to have multiple (recurrent) miscarriages or a pregnancy loss during the second or third trimester. Some research suggests that the factor V Leiden mutation may also increase the risk of other complications during pregnancy, including pregnancy-induced high blood pressure (preeclampsia), slow fetal growth, and early separation of the placenta from the uterine wall (placental abruption). However, the association between the factor V Leiden mutation and these complications has not been confirmed. Most women with factor V Leiden thrombophilia have normal pregnancies. -

Coagadex, Human Coagulation Factor X
26 July 2018 EMA/CHMP/455550/2018 Committee for Medicinal Products for Human Use (CHMP) CHMP extension of indication variation assessment report Coagadex International non-proprietary name: human coagulation factor X Procedure No. EMEA/H/C/003855/II/0007 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2018. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 5 1.1. Type II variation .................................................................................................. 5 1.2. Steps taken for the assessment of the product ......................................................... 6 2. Scientific discussion ................................................................................ 6 2.1. Introduction......................................................................................................... 6 2.2. Non-clinical aspects .............................................................................................. 7 2.3. Clinical aspects .................................................................................................... 7 2.3.1. Introduction ..................................................................................................... -

Factor V Leiden Thrombophilia Jody Lynn Kujovich, MD
GENETEST REVIEW Genetics in Medicine Factor V Leiden thrombophilia Jody Lynn Kujovich, MD TABLE OF CONTENTS Pathogenic mechanisms and molecular basis.................................................2 Obesity ...........................................................................................................8 Prevalence..............................................................................................................2 Surgery...........................................................................................................8 Diagnosis................................................................................................................2 Thrombosis not convincingly associated with Factor V Leiden....................8 Clinical diagnosis..............................................................................................2 Arterial thrombosis...........................................................................................8 Testing................................................................................................................2 Myocardial infarction.......................................................................................8 Indications for testing......................................................................................3 Stroke .................................................................................................................8 Natural history and clinical manifestations......................................................3 Genotype-phenotype -
![PROTEIN C DEFICIENCY 1215 Adulthood and a Large Number of Children and Adults with Protein C Mutations [6,13]](https://docslib.b-cdn.net/cover/8040/protein-c-deficiency-1215-adulthood-and-a-large-number-of-children-and-adults-with-protein-c-mutations-6-13-1348040.webp)
PROTEIN C DEFICIENCY 1215 Adulthood and a Large Number of Children and Adults with Protein C Mutations [6,13]
Haemophilia (2008), 14, 1214–1221 DOI: 10.1111/j.1365-2516.2008.01838.x ORIGINAL ARTICLE Protein C deficiency N. A. GOLDENBERG* and M. J. MANCO-JOHNSON* *Hemophilia & Thrombosis Center, Section of Hematology, Oncology, and Bone Marrow Transplantation, Department of Pediatrics, University of Colorado Denver and The ChildrenÕs Hospital, Aurora, CO; and Division of Hematology/ Oncology, Department of Medicine, University of Colorado Denver, Aurora, CO, USA Summary. Severe protein C deficiency (i.e. protein C ment of acute thrombotic events in severe protein C ) activity <1 IU dL 1) is a rare autosomal recessive deficiency typically requires replacement with pro- disorder that usually presents in the neonatal period tein C concentrate while maintaining therapeutic with purpura fulminans (PF) and severe disseminated anticoagulation; protein C replacement is also used intravascular coagulation (DIC), often with concom- for prevention of these complications around sur- itant venous thromboembolism (VTE). Recurrent gery. Long-term management in severe protein C thrombotic episodes (PF, DIC, or VTE) are common. deficiency involves anticoagulation with or without a Homozygotes and compound heterozygotes often protein C replacement regimen. Although many possess a similar phenotype of severe protein C patients with severe protein C deficiency are born deficiency. Mild (i.e. simple heterozygous) protein C with evidence of in utero thrombosis and experience deficiency, by contrast, is often asymptomatic but multiple further events, intensive treatment and may involve recurrent VTE episodes, most often monitoring can enable these individuals to thrive. triggered by clinical risk factors. The coagulopathy in Further research is needed to better delineate optimal protein C deficiency is caused by impaired inactiva- preventive and therapeutic strategies. -

PMP22 Earrying the Trembler Or Tremblerj Mutation Is Intracellularly Retained in Myelinating Schwann Cells in Vivo
PMP22 earrying the Trembler or TremblerJ mutation is intracellularly retained in myelinating Schwann cells in vivo by: Joshua Joseph Colby Center for Neuronal Survival Montreal Neurological Institute De partment of Pathology McGill University Montreai, Quebec, Canada Submitted in March, 2000 A thesis submitted to the Faculty of Graduate Studies and Research in partial Mfillment of the requirements for the degree of Master of Science (Pathology) O Joshua Colby, 2000 National Library Biiiothbque nationale du Canada Acquisitions arid Acquisitions et Bibliraphic Services services bibliographiques 395 W.lingtori Street 395. rwWeYingiMi OtIawaON KlAW OWawaON KlAONQ canada Canada The author has granteci a non- L'auteur a accordé une licence non exclusive licence aUowing the exclusive permettant à la National Lhrary of Canada to Bibliothèque nationaie du Canada de reproduce, 10- distri'bute or seii reproduire, prêter, distribuer ou copies of this thesis in microform, vendre des copies de cette thèse sous paper or electronic formats. la forme de microfiche/nIm, de reproduction sur papier ou sur format électronique. The author retains ownership of the L'autwr conserve la propriété du copyright in this thesis. Neither the droit d'auteur qui protège cette thèse. thesis nor substantial extracts fiom it Ni la îhèse ni des extraits substantiels may be printed or othecwise de celle-ci ne doivent être imprimés reproduced without the author's ou autrement reproduits saus son permission. autorisation. The most common cause of human hereditary neuropathies is a duplication in the peripheral myelin protein-22 (PMP22) gene. PM.22 is an integral membrane glycoprotein expressed primdy in the compact myelin of the mammalian peripheral nervous system. -
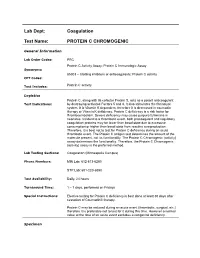
Lab Dept: Coagulation Test Name: PROTEIN C CHROMOGENIC
Lab Dept: Coagulation Test Name: PROTEIN C CHROMOGENIC General Information Lab Order Codes: PRC Protein C Activity Assay; Protein C Immunologic Assay Synonyms: 85303 – Clotting inhibitors or anticoagulants; Protein C activity CPT Codes: Test Includes: Protein C activity Logistics Protein C, along with its cofactor Protein S, acts as a potent anticoagulant Test Indications: by destroying activated Factors 5 and 8. It also stimulates the fibrinolytic system. It is Vitamin K dependent, therefore it is decreased in coumadin therapy or Vitamin K deficiency. Protein C deficiency is a risk factor for thromboembolism. Severe deficiency may cause purpura fulminans in neonates. Incident to a thrombotic event, both procoagulant and regulatory coagulation proteins may be lower than basal state due to excessive consumption or higher than basal state from reactive overproduction. Therefore, it is best not to test for Protein C deficiency during an acute thrombotic event. The Protein C antigen test determines the amount of the molecule present, not its functionality. The Protein C Chromogenic (activity) assay determines the functionality. Therefore, the Protein C Chromogenic (activity) assay is the preferred method. Lab Testing Sections: Coagulation (Minneapolis Campus) Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1 – 7 days, performed on Fridays Special Instructions: Elective testing for Protein C deficiency is best done at least 30 days after cessation of Coumadin® therapy. Protein C may be reduced during an acute event (thrombotic, surgical, etc.) therefore it is preferable not to test for it during this time. However a normal value at the time of an acute event excludes a congenital deficiency. -

Assessing Plasmin Generation in Health and Disease
International Journal of Molecular Sciences Review Assessing Plasmin Generation in Health and Disease Adam Miszta 1,* , Dana Huskens 1, Demy Donkervoort 1, Molly J. M. Roberts 1, Alisa S. Wolberg 2 and Bas de Laat 1 1 Synapse Research Institute, 6217 KD Maastricht, The Netherlands; [email protected] (D.H.); [email protected] (D.D.); [email protected] (M.J.M.R.); [email protected] (B.d.L.) 2 Department of Pathology and Laboratory Medicine and UNC Blood Research Center, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA; [email protected] * Correspondence: [email protected]; Tel.: +31-(0)-433030693 Abstract: Fibrinolysis is an important process in hemostasis responsible for dissolving the clot during wound healing. Plasmin is a central enzyme in this process via its capacity to cleave fibrin. The ki- netics of plasmin generation (PG) and inhibition during fibrinolysis have been poorly understood until the recent development of assays to quantify these metrics. The assessment of plasmin kinetics allows for the identification of fibrinolytic dysfunction and better understanding of the relationships between abnormal fibrin dissolution and disease pathogenesis. Additionally, direct measurement of the inhibition of PG by antifibrinolytic medications, such as tranexamic acid, can be a useful tool to assess the risks and effectiveness of antifibrinolytic therapy in hemorrhagic diseases. This review provides an overview of available PG assays to directly measure the kinetics of plasmin formation and inhibition in human and mouse plasmas and focuses on their applications in defining the role of plasmin in diseases, including angioedema, hemophilia, rare bleeding disorders, COVID- 19, or diet-induced obesity.